- Компании
- Takeda. О компании, буклеты, каталоги, контакты
- Olympus. О компании, буклеты, каталоги, контакты
- Boston Scientific. О компании, буклеты, каталоги, контакты
- Pentax. О компании, буклеты, каталоги, контакты
- Fujifilm & R-Farm. О компании, буклеты, каталоги, контакты
- Erbe. О компании, буклеты, каталоги, контакты
- Еще каталоги
- Мероприятия
- Информация
- Обучение
- Классификации
- Атлас
- Quiz
- Разделы
- Пациенту
QR-код этой страницы
Для продолжения изучения на мобильном устройстве ПРОСКАНИРУЙТЕ QR-код с помощью спец. программы или фотокамеры мобильного устройства
Документы и приказы: JGES guidelines for colorectal endoscopic submucosal dissection/endoscopic mucosal resection

Полный текст статьи:
JGES guidelines for colorectal endoscopic submucosal dissection/endoscopic mucosal resection
Shinji Tanaka,1,2 Hiroshi Kashida,1 Yutaka Saito,1 Naohisa Yahagi,1 Hiroo Yamano,1 Shoichi Saito,1 Takashi Hisabe,1 Takashi Yao,2 Masahiko Watanabe,2,3 Masahiro Yoshida,4 Shin-ei Kudo,1 Osamu Tsuruta,1 Ken-ichi Sugihara,2 Toshiaki Watanabe,2 Yusuke Saitoh,1 Masahiro Igarashi,1 Takashi Toyonaga,1 Yoichi Ajioka,2 Masao Ichinose,1 Toshiyuki Matsui,1,3 Akira Sugita,3 Kentaro Sugano,4 Kazuma Fujimoto1 and Hisao Tajiri1
1Japan Gastroenterological Endoscopy Society, 2Japanese Society for Cancer of the Colon and Rectum, 3Japanese Society of Coloproctology and 4Japanese Society of Gastroenterology, Tokyo, Japan
Colorectal endoscopic submucosal dissection (ESD) has become common in recent years. Suitable lesions for endoscopic treat-ment include not only early colorectal carcinomas but also many types of precarcinomatous adenomas. It is important to establish practical guidelines in which the preoperative diagnosis of colorectal neoplasia and the selection of endoscopic treatment procedures are properly outlined, and to ensure that the actual endoscopic treatment is useful and safe in general hospitals when carried out in accordance with the guidelines. In coopera-tion with the Japanese Society for Cancer of the Colon and Rectum, the Japanese Society of Coloproctology, and the Japa-nese Society of Gastroenterology, the Japan Gastroenterological Endoscopy Society has recently compiled a set of colorectal
ESD/endoscopic mucosal resection (EMR) guidelines using evidence-based methods. The guidelines focus on the diagnostic and therapeutic strategies and caveat before, during, and after ESD/EMR and, in this regard, exclude the specific procedures, types and proper use of instruments, devices, and drugs.
Although eight areas, ranging from indication to pathology, were originally planned for inclusion in these guidelines, evidence was scarce in each area. Therefore, grades of recommendation were determined largely through expert consensus in these areas.
Key words: colorectal tumor, early colorectal carcinoma, endo-scopic mucosal resection (EMR), endoscopic submucosal dissec-tion (ESD), guidelines
A
T PRESENT, WE can select various techniques in endoscopic treatment for colorectal tumors. Basically, complete en bloc resection is indicated for early colorectal carcinoma regardless of tumor size. Although endoscopic submucosal dissection (ESD) has made it possible, colorec-tal ESD is technically more difficult to carry out than upper-gastrointestinal ESD and, hence, it is essential to prevent complications such as perforation. However, among epithe-lial colorectal tumors that can be treated by endoscopic treat-ment, there are many adenomatous lesions that may be
regarded as precarcinomatous in addition to early carcino-mas. Therefore, accurate and qualitative preoperative diag-nosis of lesions and the selection of appropriate treatment on the basis of a precise diagnosis are essential.
In this capacity the Guidelines Committee of the Japan Gastroenterological Endoscopy Society (JGES) drafted the Colorectal ESD/EMR Guidelines (hereinafter referred to as the Guidelines) with the aim of ensuring the appropriate clinical introduction of colorectal ESD in relation to endo-scopic mucosal resection (EMR). These guidelines focus on the diagnostic and therapeutic strategies and stipulations before, during, and after EMR and ESD and do not contain specific information about the procedures, types and proper use of instruments, devices, and drugs. In the Guidelines, differences between colorectal EMR and ESD, preoperative diagnosis, and perioperative care are also described on the basis and strength of clinical evidence.
We created the Guidelines in accordance with the Proce-dures for the Evaluation, Selection, and Publication of
Corresponding: Shinji Tanaka, Endoscopy and Medicine, Hiro-shima University, 1-2-3 Kasumi, Minami-ku, Hiroshima 734-8551, Japan. Email: colon@hiroshima-u.ac.jp These guidelines have been published in Gastroenterol. Endosc. 2014: 56; 1598–1617 (in Japanese).
Received 12 November 2014; accepted 2 February 2015.
bs_bs_banner
Digestive Endoscopy 2015; 27: 417–434 doi: 10.1111/den.12456
© 2015 The Authors Digestive Endoscopy © 2015 Japan Gastroenterological Endoscopy Society
417
Japanese Clinical Practice Guidelines in Medical Informa-tion Network Distribution Service (MINDS) 2007,1 taking into account levels of evidence and grades of recommenda-tion with regard to evaluating evidence-based medicine (Table 1), as reported previously.2 Although eight areas, ranging from indication to pathology, were originally planned for inclusion in the guidelines, evidence in each area was scarce, which has resulted in the grades of recommen-dation being mostly determined through expert consensus.
We established six categories for evaluation, as follows: indications, techniques, complications, treatment outcome (recurrence, metastasis, and prognosis), postoperative follow up, and pathology. For each clinical question (CQ), system-atic document retrieval was done by searching PubMed and Igaku Chuozasshi for articles published from 1985 to 2012.
For insufficient or unsearchable documents, hand searching was also done. The retrieved documents were evaluated, and pertinent documents were adopted. Subsequently, a state-ment and an explanation were created for each CQ. Members of the Guidelines Creation Committee set the levels of evidence and the grades of recommendations in their respon-sible fields by using the MINDS Grade of Recommenda-tions, as described above. For the created statements, nine members of the Guidelines Creation Committee voted by using the Delphi method, as reported previously.2
INDICATION FOR ENDOSCOPIC OR
SURGICAL TREATMENT
Basic principles
W
HEN EARLY COLORECTAL carcinoma is diag-nosed, the patient is recommended to undergo endo-scopic or surgical treatment (level of evidence: IVb, grade of recommendation: B). When surgical treatment was carried out, the 5-year survival rate of colorectal carcinoma was reported to be 94.3% for stage 0 and 90.6% for stage I.
Curability was reported to be 92.7% when endoscopic treat-ment was carried out.3 Thus, excellent results could be obtained from both surgical treatment and endoscopic treatment.4,5 In cases where the risk exceeds the benefit of endoscopic treatment, such as when a patient’s general condition is extremely poor, it is recommended to abandon the treatment (level of evidence: V, grade of recommendation: C1). In particular, the application of endoscopic treatment to elderly patients (≥65 years) must be carefully considered. Many elderly patients have poor general condition and suffer from comorbidities. The frequency of complications associated with endoscopic treatment is high in these patients.6 In con-trast, some reports have indicated that endoscopic treatment could be safely carried out even for elderly patients.7,8 For very elderly patients (≥85 years), endoscopic treatment should be done only when the expected advantage is likely to outweigh the risk of complications associated with the resec-tion, while also considering the average life expectancy, comorbidities, and body age of the patient.
When carrying out endoscopic treatment, a patient’s general condition and medications must be verified, and informed consent must be obtained (level of evidence: VI, grade of recommendation: C1). Before carrying out endo-scopic treatment, a patient’s comorbidities and medications must be thoroughly evaluated. In particular, hemorrhage may develop when a patient taking an antithrombotic agent (anticoagulant or antiplatelet) undergoes endoscopic treat-ment without discontinuing the drug, whereas a cerebrocar-diovascular event may occur if the patient discontinues the medication. After evaluating both risks, the decision should be made regarding whether the patient should continue to take the medication. If drug discontinuation is decided, the optimal timing for drug discontinuation and resumption must be carefully evaluated.2 The risk of thromboembolism differs depending on the status of the patient’s underlying disease, and the type and time of placement of artificial valves or stents. The risk of hemorrhage differs depending on the kind of endoscopic examination and treatment. Both ESD and EMR are considered to have a high risk of hemorrhage.
Table 1 Levels of evidence and grades of recommendations: MINDS Grade of Recommendations Levels of evidence I: Systematic review/meta-analysis II: Several randomized controlled trials III: Non-randomized controlled trial IVa: Analytical epidemiological study: cohort study IVb: Analytical epidemiological study: case–control study, cross-sectional study V: Descriptive study (case report and case series) VI: Opinions of special committees and individual experts that are not based on patient data Grades of recommendations A: Strong scientific evidence exists and the therapy is strongly recommended B: Scientific evidence exists and the therapy is recommended C1: No scientific evidence exists but the therapy is recommended C2: No scientific evidence exists and the therapy is not recommended D: Scientific evidence of ineffectiveness or danger exists and the therapy is not recommended MINDS, Medical Information Network Distribution Service.
418 S. Tanaka et al. Digestive Endoscopy 2015; 27: 417–434
© 2015 The Authors Digestive Endoscopy © 2015 Japan Gastroenterological Endoscopy Society
As a general rule, written informed consent (IC) for car-rying out endoscopic treatment must be obtained from the patient. The IC form must contain the following items: (i) name and condition of the patient’s disease; (ii) reasons for recommending endoscopic treatment; (iii) actual details of the procedure to be carried out; (iv) expected outcomes; (v) predicted risks; (vi) alternative methods that could substitute for endoscopic treatment and information on the compari-son; and (vii) prognosis if the patient does not undergo endoscopic treatment.9 When it is difficult to sufficiently communicate with a patient, IC must be obtained from an appropriate representative. With regard to the use of sedation during endoscopic treatment, it is advisable to obtain IC in which the expected effect and risk of complications are com-pletely explained in a written document.
Indication for endoscopic treatment Non-carcinoma
Resection is recommended for adenomas ≥6 mm in size.
Resection is recommended for superficial depressed-type lesions (type 0–IIc) even when the lesion is ≤5 mm in size.
Typical hyperplastic polyps ≤5 mm in size that are present in the distal colon may be left untreated (level of evidence: IVb, grade of recommendation: B). Among adenomas and early carcinomas, the carcinoma rate of protruded-type and super-ficial elevated-type lesions ≤5 mm in size is low, and these adenomas are very unlikely to become a T1 (submucosal [SM]) carcinoma. However, the rate of SM invasion (i.e. the T1 [SM] carcinoma rate of lesions >6 mm) increases as the size of the lesion increases.10–15 Despite an extensive search of the literature, we could find no clear evidence regarding the carcinoma rate and prognosis of microlesions ≤5 mm in size in cases where it is left untreated. Some studies reported that colorectal adenomas ≤5 mm in size that had been fol-lowed for several years showed minimal changes.16–18 There-fore, prompt treatment is not required for protruded-type and superficial protruded-type adenomas ≤5 mm in size. Super-ficial depressed-type lesions exhibit a certain carcinoma rate and a certain rate of SM invasion even when their size is ≤5 mm.10,11,13,14 Although adenomas themselves are benign, it is expected that their removal will prevent the development of colorectal carcinoma.19,20 Most colorectal neoplasms are adenomas,9 and these adenomas can be cured by using EMR or piecemeal EMR techniques.21,22 For some neoplasms, endoscopic treatment is technically difficult to carry out depending on the site or size of the lesion.
According to genetic-pathological analyses, some colorectal carcinomas are assumed to develop from serrated lesions through the so-called serrated pathway. However, the natural history and carcinoma rate of serrated lesions have not been sufficiently elucidated. The risk for colorectal car-cinoma is reported to be high in patients with sessile serrated adenoma/polyp (SSA/P).23–27 However, data on how often
and how fast carcinoma development occurs within the SSA/P itself have been insufficient.28–32 Large or dysplastic SSA/P has the potential of developing into a carcinoma. In contrast, the possibility of carcinoma development is consid-ered to be extremely low for typical hyperplastic polyps ≤5 mm in size present in the distal colon or rectum.33
Carcinoma
Among early colorectal carcinomas (Tis/T1), lesions with little possibility of lymph node metastasis and higher expec-tancy of curability with en bloc resection on the basis of the size and the location are usually treated endoscopically because such cases are expected to be curable. Obvious clinical T1b carcinomas (submucosal invasion depth ≥1000 μm) are usually treated surgically. When endoscopic treatment is carried out for colorectal carcinomas, en bloc resection is the principal approach; however, piecemeal resection is also acceptable when the possibility of submu-cosal invasion can be definitively excluded and if the treat-ment is appropriately carried out (level of evidence: IVb, grade of recommendation: B).
In early colorectal carcinomas, lymph node metastasis is difficult to predict. In contrast, invasion depth can be very precisely predicted when image-enhanced endoscopy, mag-nifying endoscopy, and/or endoscopic ultrasonography (EUS) are used concurrently (discussed below).
Among the endoscopic treatments, ESD is the most suit-able method for en bloc resection.34–40 Piecemeal EMR may make it difficult to establish a pathological diagnosis of the invasion depth and to determine a free resection margin. The number of resected pieces must be minimized, and the region suspected to contain a carcinoma should not be sectioned.
With a larger tumor size and a greater number of resected pieces, the local recurrence rate increases.41–43 When carry-ing out piecemeal EMR, magnifying endoscopic observa-tion, which is the best way to identify the carcinomatous part of the lesion, should be carried out before the treatment, and the carcinomatous area should not be sectioned. Otherwise, it would be difficult to evaluate the invasion depth or vessel invasion, and an additional treatment such as lymph node dissection might not be done even when it is necessary in case of submucosal invasive carcinoma.
Laterally spreading tumors (LST) are classified into granular type (LST-G) and non-granular type (LST-NG). In LST-NG, the pseudo-depressed type (PD), which is expressed as IIc+IIa or IIa+IIc according to the Japanese Classification of Colorectal Carcinoma,44 is associated with multifocal invasion, the foci of which are often difficult to predict. In addition, LST-NG (PD) is frequently associated with fibrosis. Therefore, in many cases, EMR is not suitable for LST-NG (PD).45 Considering the high possibility of deep submucosal invasion in LST-NG (PD), whether the lesion is indicated for surgical operation or for endoscopic treatment should be carefully considered. To determine the indication
Digestive Endoscopy 2015; 27: 417–434 Colorectal ESD/EMR guidelines 419
© 2015 The Authors Digestive Endoscopy © 2015 Japan Gastroenterological Endoscopy Society
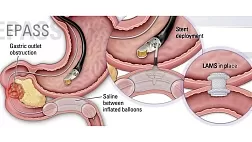
for ESD or EMR for LST, overall judgment based on the subclassification of LST (Fig. 1) and on the pit pattern diag-nosis by using magnifying observation is useful.46 The details of evaluating lesions for the ESD technique are pre-sented in a draft proposed by the Colorectal ESD Standard-ization Implementation Working Group (Table 2).34,35,38,47,48
PREOPERATIVE DIAGNOSIS
Distinction between adenoma and adenocarcinoma
B
EFORE CARRYING OUT colorectal ESD or EMR, it is important to distinguish between adenoma and adenocarcinoma in order to determine whether the lesion is benign or malignant and to characterize the marginal demar-cation of the lesion. In the large intestine, adenoma and ‘carcinoma in/with adenoma’ lesions are often detected in addition to early carcinomas without adenoma. Therefore, not only the malignancy of an entire lesion but also the carcinomatous and adenomatous parts of the lesion must be correctly assessed and distinguished. Consequently, thera-peutic strategies such as the use of ESD or EMR, selection of piecemeal EMR, and a deliberate planned sectioning line can be determined.49 When image-enhanced endoscopy and magnifying observation are used, a distinction between adenoma and
Figure 1 Subtypes of laterally spread-ing tumors (LST) (classification should be done on the basis of images obtained by using indigocarmine dye spraying). (a) Homogeneous type: LST-G (Homo). (b) Nodular mixed type: LST-G (Mix). (c) Flat-elevated type: LST-NG (F). (d) Pseudo-depressed type: LST-NG (PD). LST-G, laterally spreading tumor granular type; LST-NG, laterally spread-ing tumor non-granular type.
Table 2 Indications for ESD for colorectal tumors† Lesions for which endoscopic en bloc resection is required 1) Lesions for which en bloc resection with snare EMR is difficult to apply Ë LST-NG, particularly LST-NG (PD) Ë Lesions showing a VI-type pit pattern Ë Carcinoma with shallow T1 (SM) invasion Ë Large depressed-type tumors Ë Large protruded-type lesions suspected to be carcinoma‡ 2) Mucosal tumors with submucosal fibrosis§ 3) Sporadic localized tumors in conditions of chronic inflammation such as ulcerative colitis 4) Local residual or recurrent early carcinomas after endoscopic resection †Partially modified from the draft proposed by the Colorectal ESD Standardization Implementation Working Group. ‡Including LST-G, nodular mixed type. §As a result of a previous biopsy or prolapse caused by peristalsis of the intestine.
EMR, endoscopic mucosal resection; ESD, endoscopic submucosal dissection; LST-G, laterally spreading tumor granular type; LST-NG, laterally spreading tumor non-granular type; PD, pseudo-depressed; SM, submucosal.
420 S. Tanaka et al. Digestive Endoscopy 2015; 27: 417–434
© 2015 The Authors Digestive Endoscopy © 2015 Japan Gastroenterological Endoscopy Society
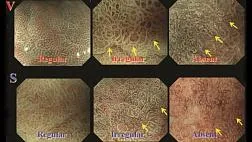
adenocarcinoma with high accuracy can be achieved (level of evidence: IVb, grade of recommendation: B). For distinc-tion between adenoma and adenocarcinoma, lesion color, surface unevenness, presence of depression, and fold con-vergence must be confirmed by ordinary observation and chromoendoscopic observation. At present, magnifying observation (pit pattern diagnosis) using dye spraying (indi-gocarmine, crystal violet etc.) and image-enhancement tech-nology (narrow band imaging [NBI], blue laser imaging [BLI] etc.) could be used for diagnosing lesions on the basis of a detailed visualization of fine surface structures (surface pattern) and microvessels.50–52 The diagnostic accuracy rate of discriminating neoplastic from non-neoplastic lesions was reported to be approximately 80% for standard observation, including magnifying chromoendoscopic observation, 96–98% for pit pattern observation, and 95% for magnifying observation using NBI and BLI.53–59 The accuracy rate of discrimination between adenoma and carcinoma was 70–90% for pit pattern observation, and a similar rate was obtained for NBI. Thus, distinction between adenoma and adenocarcinoma with high accuracy can be achieved with magnifying endoscopic observation.60–64 However, it was recently indicated that some lesions that had been previously diagnosed as non-neoplastic exhibited neoplastic prolifera-tion (SSA/P). Research on the diagnosis and treatment of these lesions is currently ongoing.65,66 In addition, it is better to avoid carrying out a biopsy in order to distinguish between adenoma and adenocarcinoma (level of evidence: V, grade of recommendation: C1). In the case of superficial-type lesions, because biopsy as a preop-erative diagnosis may cause fibrosis in the submucosal layer and lead to a positive non-lifting sign, subsequent endo-scopic treatment will be difficult. Therefore, it is better to avoid carrying out a biopsy for making a preoperative diag-nosis.38,47 For large lesions such as LST-G,44 which, in many cases, are ‘carcinoma in adenoma’, a simple biopsy may not show an accurate yield as a qualitative diagnosis. Therefore, a diagnosis based on magnifying endoscopic observation as an optical biopsy (histological diagnosis by endoscopic imaging without forceps biopsy) is more effective.
Diagnosis of invasion depth
For early colorectal carcinoma, it is necessary to estimate the degree of SM invasion before carrying out endoscopic treat-ment (level of evidence: IVb, grade of recommendation: B).
The risks of vascular invasion and lymph node metastasis differ according to the SM invasion depth of the carcinoma.
For deep invasive T1 (SM) carcinoma, the risk of incomplete resection is high in endoscopic treatment. Therefore, the degree of SM invasion must be estimated before carrying out endoscopic treatment. Furthermore, to carry out accurate
pathological evaluation of endoscopically resected speci-mens, it is important to indicate the part of SM invasion in the whole lesion.49 When diagnosing invasion depth, if a deep depression, expansive appearance, submucosal tumor-like margin, or defective extension is detected during ordinary or chromo-endoscopic observation, deep SM invasion may be consid-ered; the accuracy rate of deep SM invasion is 70–80%.67,68 In pit pattern diagnosis with dye-spraying magnifying endo-scopic observation, an accuracy rate of approximately 90% can be obtained if the VN-type pit pattern is observed. The accuracy rate of protruded-type lesions tends to be slightly lower than that of superficial-type lesions.69–71 Although magnifying observation using NBI/BLI is slightly inferior to pit pattern diagnosis in terms of accuracy, a similar outcome can be obtained.72–74 The accuracy rate is approximately 80% when ultrasonography is used; however, the visualization capacity is affected by the condition and morphology of the lesion.75–79 These diagnostic methods have certain advan-tages and disadvantages. As diagnostic accuracy differs according to the macroscopic type and growth type of the lesion, appropriate diagnostic methods should be combined as the situation requires.
TECHNIQUES
Definition of ESD and EMR
I
N EMR,80,81 a physiological saline solution or a sodium hyaluronate solution82–84 is locally injected into the sub-mucosa of a superficial-type tumor through the injection needle. The lesion is strangled with a snare and then resected by applying high-frequency current. Although polyp resection in cold polypectomy is carried out without applying high-frequency current, high-frequency current is essential in EMR and is fundamentally applied. In piece-meal EMR, a large nodule or carcinomatous region is first cut into a large piece to accurately carry out histological diagnosis, and the residual flat part is then deliberately cut into pieces; this is also known as planned piecemeal EMR.
In ESD, a physiological saline solution or a sodium hyal-uronate solution is locally injected into the submucosa of a tumor through the injection needle. The circumference of the lesion is then incised using a needle-type knife for ESD with electrical cutting current produced by the equipment, and the submucosal layer is then dissected. This technique can resect the lesion in one piece regardless of its size.37,39,85–88 In April 2012 in Japan, the National Health Insurance scheme began offering coverage for expenses incurred for ESD procedures for early-stage malignant colorectal tumors 20–50 mm in size.
Digestive Endoscopy 2015; 27: 417–434 Colorectal ESD/EMR guidelines 421
© 2015 The Authors Digestive Endoscopy © 2015 Japan Gastroenterological Endoscopy Society
In the Guidelines, specific terminology is used to distin-guish several forms of ESD, as follows. A technique in which dissection of the submucosal layer is completed without using a snare is defined as ‘actual (narrowly defined) ESD’.89,90 Likewise, a technique in which snaring is done without dissecting the submucosal layer after incising the circumference of the lesion alone, by using a knife for ESD or the tip of a snare, is defined as ‘precutting EMR’.91 Finally, a technique in which the submucosal layer is dissected and snaring is carried out after the ESD procedure (mucosal incision + submucosal dissection), by using a knife for ESD or the tip of a snare, is defined as ‘hybrid ESD’.89,90,92 Other terminologies for precutting EMR91 and hybrid ESD are reported in the literature, but the Guidelines use the terms defined above.
Choosing between ESD and EMR
En bloc resection is desirable as an endoscopic treatment for early colorectal carcinoma. However, piecemeal EMR is per-missible for some adenoma and ‘carcinoma in adenoma’ lesions when appropriately carried out. When carrying out piecemeal EMR, magnifying endoscopic observation should be carefully carried out before the treatment, and the carci-nomatous area should never be cut into pieces (level of evidence: III, grade of recommendation: B).
The reason for this restriction is that if SM invasive car-cinoma was cut into pieces, pathological diagnosis for the invasion depth and lymph-vascular invasion would be diffi-cult, and necessary additional treatment might not be done.21,39,45,93,94 Previous reports showed that when piecemeal EMR was carried out, magnifying endoscopic observation of the lesion margin and ulcer base after the resection is useful to decrease the local residual/recurrence rate.95 To confirm local residual/recurrence, follow-up colonoscopy should be done approximately 6 months after the treatment.42,96–98 The frequency of T1 (SM) carcinoma increases as the tumor size increases. With multi-piecemeal resection, which makes the pathological reconstruction of a tumor difficult, histological evaluation is also difficult and the local residual/ recurrence rate is higher.42,92,96,97 For large lesions with a size greater than half of the circumference of the colorectal lumen, piecemeal EMR should be avoided, and ESD or a surgical operation should be done based on the skill level of the endoscopist, the therapeutic environment of the hospital, the condition of patient, and the status of the lesion.38,86,87 Following the development of the requisite devices and the establishment of appropriate methods, colorectal ESD can be safely and accurately carried out by experts. However, when carrying out ESD, it is important to prepare various devices (ESD knives, devices, distal attachments, local injec-tion agents such as sodium hyaluronate,82–84 a carbon dioxide
insufflator,85 and endoscopic clips to prevent and treat adverse events, such as perforation, and to ensure that there are appropriate facilities for hospitalization and surgical treatment.
Endoscopic treatment for lesions positive for non-lifting sign
Although the majority of such lesions are T1 carcinomas, a lesion exhibiting a positive non-lifting sign can potentially be a mucosal tumor (adenoma or mucosal carcinoma).
Therefore, if a lesion is endoscopically judged as a mucosal tumor, ESD/EMR is appropriate (level of evidence: III, grade of recommendation: B).
For mucosal lesions that are non-lifting sign positive99–101 (including adenomas) and residual/recurrence lesions, ESD can resect those lesions for which EMR is generally difficult to apply and for which en bloc resection is desirable (in particular, lesions suspected to be early carcinoma and LST-NG). However, ESD must be carefully carried out while checking for perforation.37,45,102–104 The non-lifting sign, first reported by Uno et al.,99,100 is a sign that helps diagnose the depth of carcinoma invasion and is often used in clinical practice. However, one multicenter study101 that compared the diagnostic accuracy based on conventional endoscopic observation with that based on the non-lifting sign has shown that the diagnostic ability of the non-lifting sign for deep SM invasive carcinoma had a sen-sitivity of 61.5%, specificity of 98.4%, positive predictive value of 80.0%, negative predictive value of 96.0%, and diagnostic accuracy of 94.8%.
For conventional endoscopic observation for deep SM invasive carcinoma, the above measures were 84.6%, 98.8%, 88.0%, 98.4%, and 97.4%, respectively. Therefore, conven-tional endoscopic observation was superior to the non-lifting sign in terms of sensitivity (84.6% vs 61.5%). Superficial-type colorectal tumors sometimes exhibit a positive non-lifting sign as a result of peristaltic motion or fibrosis caused by biopsy, although such lesions are usually of the mucosal type.99,100 Therefore, preoperative endoscopic diagnosis should be made carefully by magnifying endoscopic obser-vation before endoscopic treatment for neoplastic lesions.
Once the lesion targeted is diagnosed as carcinoma, then the invasion depth should be diagnosed by magnifying endos-copy, and biopsy should be avoided.
Endoscopists who carry out colorectal ESD should be registered with the JGES or must possess skills similar to those of registered endoscopists in Japan. Familiarity with esophageal and gastric ESD alone may be insufficient. The minimum requirements for endoscopists are as follows: (i) having sufficient understanding of the anatomical features of the large intestine; (ii) having the ability to carry out the
422 S. Tanaka et al. Digestive Endoscopy 2015; 27: 417–434
© 2015 The Authors Digestive Endoscopy © 2015 Japan Gastroenterological Endoscopy Society
axis-keeping shortening technique when inserting a colono-scope; (iii) having the skill to carry out an insertion tech-nique by which the colorectal endoscope could be smoothly and accurately advanced to the cecum in the shortest dis-tance possible; and (iv) having familiarity with the basic techniques of polypectomy, EMR, piecemeal EMR, hemo-stasis, and clip suture. Experience with gastric ESD is helpful in preparation for colorectal ESD. If the experience of the endoscopist is limited to colorectal examination, colorectal ESD should be carried out only after sufficient training in ESD by using living or isolated porcine stomach or colon.105–107
COMPLICATIONS DURING PROCEDURES
M
AIN ACCIDENTAL COMPLICATIONS during colonoscopic treatment are perforation and bleeding.
Perforation is the condition in which the abdominal cavity is visible from the colorectal lumen because of mural tissue defects. The presence of free air is not always detected on X-ray examination. In contrast, the condition in which the tissue defect reaches other parenchymal organs is defined as penetration. Various definitions have been proposed for bleeding, such as a decrease in hemoglobin by >2 mg/dL or the requirement for blood transfusion. However, these defi-nitions have not been established on the basis of solid evi-dence. The presence of marked bloody stool after treatment or the requirement for a certain measure for hemostasis after treatment is often defined as delayed bleeding. With regard to the frequency of these accidental complications, perforation rates during endoscopic resection are reported to be 0.05%, 0.58–0.8%, and 2%–14% for polypectomy, EMR, and ESD, respectively. Moreover, the delayed bleeding rates are reported to be 1.6%, 1.15%–1.7%, and 0.7%–2.2% for pol-ypectomy, EMR, and ESD, respectively.40,88,108–110
Prevention and management of perforation
As the colonic wall is thinner than that of the stomach, the risk of perforation during the procedure is higher in the colon than in the stomach. Before the procedure, sufficient pre-treatment is required to prepare for the possibility of perfo-ration. During the procedure, it is essential to ensure good maneuverability of the scope. It is important to select a scope according to the location and morphology of the tumor, and it is necessary to use appropriate devices, local injection agents, and a carbon dioxide insufflator for a successful procedure.85,111 When perforation occurs during the proce-dure, clipping should be carried out as far as possible, regardless of the location (level of evidence: IVb, grade of recommendation: B). When closure of the perforation is complete, surgical rescue can usually be avoided by giving
i.v. antibiotics and fasting.108,112,113 The presence of free air within the abdominal cavity after perforation on computed tomography (CT) evaluation cannot be used to guide the decision for emergency surgery.113 It is necessary to decide the timing of the emergency surgery carefully in cooperation with surgeons. Nevertheless, in cases of incomplete closure of the perforation, emergency surgery should be carried out as soon as possible as the risk of pan-peritonitis is extremely high in this situation.
In cases of rectal lesion below the peritoneal reflection, perforation into the abdominal cavity would not occur as a result of anatomical features; however, penetration into the retroperitoneum occurs and, consequently, mediastinal emphysema or subcutaneous emphysema may occur.114
Prevention and management of bleeding
For bleeding associated with endoscopic resection, clipping or coagulation is appropriate. In case of minor bleeding from a small vessel, contact coagulation with the tip of a knife or coagulation with hemostatic forceps is usually used for hemostasis. In cases of severe bleeding from a large vessel or artery, hemostatic forceps are indispensable. To avoid delayed perforation caused by thermal damage, the bleeding point should be grasped precisely with hemostatic forceps, and application of electrocoagulation should be minimized.
Generally, severe bleeding seldom occurs in the colon in comparison with the stomach. However, in the rectum, espe-cially below the peritoneal reflection, a pulsating large exposed vessel is sometimes present within the resection wound. Therefore, clipping is sometimes used in such cases to prevent delayed bleeding. Serious delayed bleeding that requires blood transfusion seldom occurs in the colon. Emer-gency endoscopy is usually required to treat exposed blood vessels in the case of continuous bloody stool.
A randomized controlled trial reported that preventive clipping after endoscopic resection did not decrease the delayed bleeding rate (0.98% with clipping and 0.96% without clipping).115 However, target lesions included in that trial were relatively small (mean size, 7.8 mm). A retrospec-tive analysis reported that preventive clipping was useful for lesions >2 cm in size (1.8% with clipping and 9.7% without clipping).116 Another retrospective analysis also suggested the potential usefulness of preventive clipping for patients undergoing endoscopic resection at an outpatient clinic.117 However, at present, no firm evidence has been obtained by randomized controlled trials for the efficacy of suturing the ESD/EMR wound to prevent delayed bleeding. In addition, one report showed that preventive clipping after polypec-tomy is poorly cost-effective in subjects who are not taking antithrombotic medication.118 Therefore, prophylactic clip-ping in EMR seems to be effective to some extent for high-
Digestive Endoscopy 2015; 27: 417–434 Colorectal ESD/EMR guidelines 423
© 2015 The Authors Digestive Endoscopy © 2015 Japan Gastroenterological Endoscopy Society
risk patients and may be effective for patients with large lesions or for those undergoing antithrombotic therapy (level of evidence: IVb, grade of recommendation: B).
PERIOPERATIVE CARE BEFORE AND AFTER
ENDOSCOPIC TREATMENT
D
URING PERIOPERATIVE CARE after endoscopic treatment, attention should be given to delayed perfo-ration and delayed bleeding, and patients should be hospital-ized if necessary (level of evidence: IVb, grade of recommendation: B). Perioperative care should be consid-ered during the clinical practice of ESD/EMR, including the hospitalization period.119 For patients using antithrombotic drugs who will undergo ESD/EMR, the reader is referred to the ‘Guidelines for Gastroenterological Endoscopy in Patients Undergoing Antithrombotic Treatment’ published by the JGES.2
Antithrombotic drugs
The guidelines mentioned above propose a strategy in which patients who undergo ESD/EMR are divided into high- and low-risk groups according to the predicted risk of thrombo-embolism. The way in which antithrombotic drugs are handled in pre-/post-ESD/EMR procedures is dependent on the risk for thromboembolism in subjects, and published JGES guidelines should be referred to for further details. In brief, withdrawal of aspirin monotherapy even in subjects who undergo ESD/EMR is not required when those subjects are deemed at high risk for thromboembolism, whereas it can be withdrawn for 3–5 days in low-risk patients. Thieno-pyridine derivatives are recommended to be replaced with aspirin or cilostazol for 5–7 days in high-risk subjects who undergo ESD/EMR procedures. However, in low-risk sub-jects, thienopyridine derivatives can be withdrawn for 5–7 days for the procedures. The procedures planned in patients taking aspirin in combination with warfarin or dabigatran should be postponed until the antithrombotics can be with-drawn. The procedures can be carried out in patients taking aspirin or cilostazol if warfarin or dabigatran is replaced with heparin. After the withdrawal of an antithrombotic drug, the drug can be given again when hemostasis is endoscopically confirmed. Careful observation against post-procedure hem-orrhage must be taken after antithrombotic drugs are resumed.
Bowel preparation
After confirming that no stenosis of the digestive tract is present, a diet preparation for colonoscopy (or food in accor-dance with the diet) and a laxative are given at bedtime on the night before the procedure. On the day of colonoscopy,
2 L of an intestinal lavage solution is given. In cases where pretreatment is incomplete, an additional intestinal lavage should be considered.
With regard to premedication and sedation, as intestinal peristalsis may hinder the treatment, if possible, a spasmo-lytic (scopolamine Buscopan®, Boehringer Ingelheim, Tokyo, Japan) is i.v. or i.m. injected after confirming that no contraindication (glaucoma, prostatic hypertrophy, and arrhythmia) is present. The use of a sedative/analgesic is determined according to the endoscopist’s judgment and the patient’s wishes. However, excessive sedation should be avoided in colorectal ESD/EMR because position changes are often required. Abdominal fullness can be reduced through carbon dioxide insufflation, decreasing the amount of sedatives required.85,111
Instruments and drugs to be prepared
When a sedative is used during the procedure or when treatment is predicted to take a considerable time, it is desirable to monitor the patient’s oxygen saturation and electrocardiogram.
Postoperative management
In the Japanese situation, EMR for lesions <2 cm in size can be carried out for outpatients. EMR and ESD for lesions >2 cm in size should be done after the patient is hospitalized.
However, no recommendations are provided in these guide-lines for the length of hospitalization and the timing of oral ingestion after endoscopic procedures. One report regarding ESD found that no adverse event occurred in a clinical pathway where the length of hospitalization was 4 nights and 5 days with oral ingestion starting 2 days after the opera-tion.119 A meal is given after confirming the absence of inflammatory findings, such as level of serum C-reactive protein (CRP), abdominal pain, and fever, while checking for delayed perforation and delayed bleeding. Both the length of hospitalization and the fasting period should be considered with regard to each specific situation.
Post-polypectomy electrocoagulation syndrome
Even in cases where no perforation has developed, abdomi-nal pain or fever may occur if the muscular layer is ruptured or thermally denatured. Pain and fever may be caused by inflammation of the peritoneum, which sometimes occurs after electrocoagulation, even when no subsequent perfora-tion occurs.120 Although for most patients conservative treat-ment can generally be carried out, it is important to adopt careful measures such as prolongation of the fasting period while considering the possibility of delayed perforation.
424 S. Tanaka et al. Digestive Endoscopy 2015; 27: 417–434
© 2015 The Authors Digestive Endoscopy © 2015 Japan Gastroenterological Endoscopy Society
Delayed perforation
Delayed perforation is an intestinal perforation that develops a certain period of time after the operation (i.e. intestinal perfo-ration that is detected after the scope has been withdrawn following completion of ESD/EMR during which perforation did not occur). Delayed perforation is diagnosed on the basis of abdominal pain, abdominal findings, presence of fever, and inflammatory response. Most cases of delayed perforation occur within 14 h after the operation. However, approximately one-third of delayed perforation cases are confirmed 24 h after the treatment. Free air, which cannot be detected by simple X-ray imaging, is sometimes found on abdominal CT. There-fore, in cases where delayed perforation is suspected, abdominal CT should be carried out. Surgeons must be called for emer-gency surgery, which is essential in cases of delayed perforation.
The incidence of delayed perforation is 0% in EMR (no data have been reported) and 0.1–0.4% in ESD (i.e. indicating that delayed perforation seldom occurs).37,88,121
Delayed bleeding
Delayed bleeding is defined as a decrease in hemoglobin by >2 g/dL or confirmation of marked hemorrhage a certain period of time after endoscopic treatment.122 Delayed bleeding does not include small amounts of bleeding such as the presence of trace amounts of blood in the stool.The incidence of delayed bleeding is reported to be 1.4–1.7% in EMR88,97 and 1.5–2.8% in ESD.37,88,97,121 Delayed bleeding is mainly observed during the period between 2 and 7 days after the operation, and a hemor-rhage observed within 10 days after the operation may be considered delayed bleeding. The effect of application of a prophylactic clip on delayed bleeding has been discussed pre-viously. A study reported that prophylactic clip application was effective for lesions >20 mm in size.123 However, the effective-ness of prophylactic clip application for high-risk lesions must be evaluated through prospective studies.
Fournier’s syndrome (fulminant necrotizing fasciitis)
In cases where the rectum is below the peritoneal reflection, perforation into the abdominal cavity does not occur because of anatomical features; however, penetration into the retro-peritoneum occurs and, consequently, mediastinal emphy-sema or subcutaneous emphysema may occur.114 Moreover, the possibility of fulminant necrotizing fasciitis (Fournier’s syndrome) cannot be dismissed, although it is extremely rare, and no study has reported its development after endo-scopic resection.124 However, when fulminant necrotizing fasciitis develops, it causes septicemia and disseminated intravascular coagulation, and the associated mortality is reported to be 20–40%. Therefore, broad-spectrum antibiot-ics and immediate surgical treatment are required.125
ASSESSMENT OF CURABILITY
C
URABILITY IS EVALUATED based on the tumor margin of the resected specimen and risk factors for lymph node/distant metastasis (level of evidence: IVb, grade of recommendation: B).
Tis (M) carcinoma
With regard to colorectal tumors, Tis (M) carcinomas gen-erally do not metastasize to lymph nodes or other organs.
These lesions can be radically cured by endoscopic local resection. However, in cases with positive lateral tumor margin or piecemeal resection, local recurrence has been reported.42,124,126 Previous reports have compared the rates of en bloc resection in EMR (piecemeal EMR) with those in ESD for mucosal lesions with tumor sizes <20 mm and >20 mm. Consequently, the rates of en bloc resection were determined to be as high as 66.5–80% in EMR when the tumor sizes were <20 mm.88,127 When the tumor sizes were ≥20 mm, the en bloc resection rate in EMR decreased as tumor size increased, and the residual/recurrence rate was 2.7–27.2%.125,128 In contrast, the en bloc resection rate in ESD was within the range of 84–94.5% (i.e. the results were
excellent).35,39,88,92,125,128
T1 (SM) carcinoma
When pT1 (SM) carcinoma is detected in a pathological examination after endoscopic treatment, the subsequent therapeutic course should be determined in accordance with the 2014 JSCCR Guidelines for the Treatment of Colorectal Cancer.129 An additional surgical operation should be carried out for deep tumor margin-positive lesions as a result of incomplete endoscopic resection. In the case of complete endoscopic resection, pT1 (SM) carcinoma can be judged to have been radically cured when all of the following condi-tions are satisfied on histological analysis: (i) vertical tumor margin-negative (histological complete resection); (ii) pap-illary adenocarcinoma or tubular adenocarcinoma; (iii) SM invasion depth <1000 μm; (iv) no vascular invasion; and (v) tumor budding grade 1 (low grade). If even one of these five conditions is not satisfied, the estimated rate of lymph node metastasis of the lesion and the background of the patient (i.e. age, coexisting disease, physical activity, intention, and quality of life after an operation that includes factors such as the construction of an artificial anus) are comprehensively evaluated and the indication for additional surgical resection is considered. Additional surgical resection is never forcibly carried out. These conditions are comprehensively evaluated, and a course involving either follow up or additional resec-tion is selected accordingly.
When a resected specimen satisfies the five conditions mentioned above, lymph node metastasis and residual/
Digestive Endoscopy 2015; 27: 417–434 Colorectal ESD/EMR guidelines 425
© 2015 The Authors Digestive Endoscopy © 2015 Japan Gastroenterological Endoscopy Society
recurrence is extremely rare (level of evidence: IVb, grade of recommendation: B). In cases in which only the SM invasion depth does not satisfy the criteria for a radical cure, and where no other risk factors for metastasis are observed, the lymph node metastasis rate has been reported to be extremely low.130–134 At present, a research project of JSCCR concerning the stratification of risk factors for the metastasis of pT1b SM cancer (SM invasion depth >1000 μm) to other organs is ongoing.
POSTOPERATIVE FOLLOW UP
T
HE AIM OF follow up after colorectal ESD/EMR is early detection of local residual/recurrence, metastasis, and metachronous lesions.133,134 Some studies have reported that endoscopic treatment for colorectal tumors decreased the incidence of colorectal carcinoma and the risk of mor-tality.135,136 Surveillance after surgical resection for colorectal carcinoma was reported to improve prognosis.137,138 Although no evidence-based consensus on the actual follow-up methods after endoscopic treatment is available in Japan, the JSGE ‘Evidence-Based Clinical Guidelines for Management of Colorectal Polyps (in press)’ guidelines recommend that follow-up colonoscopy should be done within 3 years after polypectomy.139 The follow-up plan should be established with regard to therapeutic techniques such as en bloc resec-tion and piecemeal resection, curability evaluation based on pathological examination of the resected specimens, risk factors for multiple lesions and carcinomas, and underlying disease. In essence, the plan must give importance to the background of each patient.
Local residual/recurrence
For early detection of local residual/recurrence, periodic observation with colonoscopy is desirable, and endoscopic measures are applicable to many early detection cases. In adenoma or pTis (M) carcinoma, when piecemeal resection is used or the tumor margin after resection is unclear and the curability cannot be accurately evaluated, colonoscopy should be done approximately 6 months after the endoscopic treatment (level of evidence: IVb, grade of recommendation: B). Compared with complete en bloc resection, histological evaluation is more difficult and the local residual/recurrence rate is higher in piecemeal resection.42,92,96,140,141 The recur-rence rates were reported to be 18.4%, 23.1%, and 30.7% at 5, 12, and 24 months after piecemeal resection, respectively.96 When the horizontal tumor margin is difficult to evaluate or when piecemeal resection is carried out, it is recommended to carry out colonoscopy within 6–12 months.49,142 No local residual/recurrence was detected in the case of adenoma or pTis (M) carcinoma for which complete en bloc
resection had been carried out and for which curative resection was concluded based on histological examination.49,129 However, in the case of pT1a (SM) carcinoma (SM invasion depth <1000 μm), histological evaluation of vascular invasion and SM invasion depth cannot be accurately carried out as resected specimens are inadequately handled; consequently, local residual/recurrence may occur. Although such cases are rare, careful handling of resected specimens must be ensured.
Recurrence or metastasis of pT1 (SM) carcinoma occurs even in cases where surgical resection including lymph node dissection has been carried out. The recurrence rate in the rectum (4.2–4.5%) is higher than in the colon (1.5%– 1.9%).143,144 In the case of endoscopic treatment, recurrence or metastasis is reported to occur mainly within 3–5 years.130,132,134,145 Therefore, in the case of pT1 (SM) carcinoma after endoscopic treatment, not only local observation with colonoscopy but also periodic follow up should be systemati-cally carried out using tumor markers such as carcinoembryonic antigen (CEA), abdominal ultrasonography, and thoracic and abdominal CT. However, no clear consensus has been reached on the actual method and time of surveillance.
Metachronous lesions
No optimal examination interval has been established to detect metachronous colorectal tumors. However, colonos-copy should be carried out within 3 years after endoscopic treatment (level of evidence: IVb, grade of recommendation: B). After endoscopic treatment, metachronous lesions and residual lesions must be monitored. As colonoscopy might not be able to detect all lesions,133,146,147 periodic endoscopic observation is essential. A retrospective surveillance study148 showed that after endoscopic treatment for T1 carcinoma, metachronous adenoma and early carcinoma were detected in 54.8% and in 11.9% of cases, respectively. This suggests that colonoscopy cannot detect all lesions. Multiple metachronous carcinomas were reported in 3.4–26.5% of early colorectal carcinomas in the period between 25.6 and 102.8 months after endoscopic treatment for T1 carcinomas.148,149 Therefore, long-term follow up should be considered. The risk of meta-chronous colorectal tumors is known to be high in cases of multiple (>3) colorectal adenomas with lesions >10 mm in size and a history of colorectal carcinoma.146,150–152 A follow-up schedule must be established on the basis of each patient’s background, including risk factors, age, and comor-bidities. In the USA, follow up after endoscopic resection is stratified according to risk, and colonoscopy is recommended to be carried out for multiple (3–10) adenomas, adenomas >10 mm in size, villous adenomas, and high-grade dysplasia 3 years after endoscopic treatment. Moreover, colonoscopy is recommended to be carried out for multiple (>10) adenomas within 3 years after endoscopic treatment.142
426 S. Tanaka et al. Digestive Endoscopy 2015; 27: 417–434
© 2015 The Authors Digestive Endoscopy © 2015 Japan Gastroenterological Endoscopy Society
PATHOLOGY
Handling of specimens
T
O JUDGE THE curability of a lesion and the necessity for additional treatment, accurate histological diagnosis is critical, and resected specimens must be appropriately handled (level of evidence: VI, grade of recommendations: C1). The resected specimen is pinned on a rubber or cork sheet so that the mucous membrane surrounding the lesion is evenly flattened and the mucous membrane surface can be observed (Figs 2,3). Subsequently, the specimen is fixed with a 10–20% formaldehyde solution for 24–48 h at room temperature.153 As a specimen rapidly autolyzes after resection, it must be fixed as quickly as possible. To prevent drying of the
specimen, it should be soaked in a physiological saline solution. Thereafter, the endoscopist is required to appro-priately display the specimen so that the difference between the specimen and the clinical images is minimized and the tumor margin of the specimen can be judged. Specimens obtained from piecemeal resection must be reconstructed to the greatest extent possible so that the tumor margin can be judged.
To carry out histological diagnosis precisely and in detail, specimens must be appropriately cut (level of evi-dence: VI, grade of recommendation: C1). An endoscopist must provide documentation (an explanatory text or an illustration) to a pathologist so that the basic information on preoperative diagnosis (including the result of biopsy), the site and morphology of the lesion, and the tumor size as well as the clinical evaluation can be accurately con-veyed. It is helpful to indicate the location that most clearly exhibits the malignancy of the lesion in clinical and imaging findings in the above documentation.
After fixation, the entire specimen is sectioned into pieces at intervals of 2–3 mm, and all slides are prepared for histological diagnosis. Procedure of the actual cutting is as follows: (i) a tangent that touches the focus closest to the horizontal tumor margin is assumed, as shown in
Figure 2 Fixed endoscopic mucosal resection specimen.
Figure 3 Fixed endoscopic submucosal dissection specimen.
Digestive Endoscopy 2015; 27: 417–434 Colorectal ESD/EMR guidelines 427
© 2015 The Authors Digestive Endoscopy © 2015 Japan Gastroenterological Endoscopy Society
Figure 4; (ii) the first shallow cut is carried out in the directionperpendicular to the tangent; (iii) shallow cuts parallel to the first cut are carried out so that all slices are not completely separated from each other, after which the specimen is photographed; and (iv) deep cuts are carried out to completely separate all the slices for the preparation of slides. When a region of the lesion is unclear, observation with a stereoscopic microscope is recommended.44
Description of pathological findings
Histological diagnosis of tumors is carried out in accordance with the Japanese Classification of Colorectal Carcinoma (8th edition).44 The histological type, depth of wall invasion, vascular invasion (ly, v), and resection tumor margins (hori-zontal, vertical) of the carcinoma are judged. In the case of pT1 (SM) carcinoma, the invasion depth (pT1a: <1000 μm or pT1b: 1000 μm≤), tumor budding, amount of interstitial tissue, and pattern of invasion are also described.44,153,154 When multiple different histological types are present in a tumor, all the types are described in decreasing order of area (e.g. tub1>pap>por2). The depth of wall invasion is repre-sented based on the deepest layer of carcinoma invasion. In the case of pT1 (SM) carcinoma, the invasion depths of pedunculated and non-pedunculated lesions are evaluated separately.
Usefulness of special staining and immunostaining
In histological diagnosis, diagnosis of types with specia-lized histology, measurement of invasion depth, and special staining and immunostaining of vascular invasion are
informative. With regard to types with specialized histology, endocrine cell carcinoma with a high grade of malig-nancy and carcinoid tumor with a low grade of malignancy/ neuroendocrine tumor must be discriminated from adeno-carcinoma. For this discrimination, immunostaining (chro-mogranin A, synaptophysin, and CD56) is effective. In the case of conventional adenocarcinoma, the grade of budding is assessed using hematoxylin-eosin (HE)-stained specimens. Cytokeratin is useful for histological evaluation because cancer cells become distinctive after immunostaining.154,155 When measuring the invasion depth, immunostaining with desmin helps to identify the muscula-ris mucosae.156,157 Elastica van Gieson staining or Victoria blue/HE double staining can be used to confirm venous invasion. To verify lymphatic vessel invasion, immuno-staining with anti-lymphatic vessel endothelial antibody (D2-40) in combination with other staining methods is preferred.154–160
ACKNOWLEDGMENTS
W
E GREATLY APPRECIATE the affiliated congress and the secretary of the JGES for their cooperation.
The guidelines committee was formed as shown in the table below. The JGES entrusted the creation of the Guidelines to seven gastroenterological endoscopists, one colorectal surgeon, one gastroenterological pathologist, and one clini-cal oncologist (a total of 10) as members of the Guidelines Committee. Moreover, five gastroenterological endoscopists, two colorectal surgeons, and one gastroenterological pathologist (a total of eight) were in charge of evaluating the Guidelines as members of the Evaluation Committee, as follows.
Figure 4 Cut-out of a resected speci-men. , mucosal cancer region; , submucosal cancer region.
428 S. Tanaka et al. Digestive Endoscopy 2015; 27: 417–434
© 2015 The Authors Digestive Endoscopy © 2015 Japan Gastroenterological Endoscopy Society
Guidelines Committee, Japan Gastroenterological Endoscopy Society Responsible Director: Kazuma Fujimoto (Department of Internal Medicine, Saga University Faculty of Medicine) Chairman: Kazuma Fujimoto (Department of Internal Medicine, Saga University Faculty of Medicine) Working Committee Chairman: Shinji Tanaka (Endoscopy and Medicine, Hiroshima University) Chairman in charge of Guidelines creation: Shinji Tanaka (Endoscopy and Medicine, Hiroshima University) Deputy Chairman: Hiroshi Kashida (Department of Gastroenterology and Hepatology, Kinki University Faculty of Medicine) Members: Yutaka Saito (Endoscopy Division, National Cancer Center Hospital) Naohisa Yahagi (Tumor Center, Keio University Hospital) Hiroo Yamano (Digestive Disease Center, Akita Red Cross Hospital) Shoichi Saito (Department of Endoscopy, The Jikei University School of Medicine) Takashi Hisabe (Department of Gastroenterology, Fukuoka University Chikushi Hospital) Takashi Yao (Department of Pathology, Juntendo University) Masahiko Watanabe (Department of Surgery, Kitazato University) External member: Masahiro Yoshida (Chemotherapy Institute, Kaken Hospital) Chairman of the Evaluation Committee: Shin-ei Kudo (Digestive Disease Center, Showa University Northern Yokohama Hospital) Deputy Chairman: Osamu Tsuruta (Digestive Disease Center, Kurume University School of Medicine) Members: Ken-ichi Sugihara (Department of Surgical Oncology, Tokyo Medical and Dental University) Toshiaki Watanabe (Department of Surgical Oncology, The University of Tokyo) Yusuke Saitoh (Department of Gastroenterology, Asahikawa City Hospital) Masahiro Igarashi (Department of Endoscopy, Cancer Institute Ariake Hospital) Takashi Toyonaga (Division of Endoscopy, Kobe University Hospital) Yoichi Ajioka (Division of Molecular and Diagnostic Pathology, Niigata University)
Список литературы:
Рекомендуемые статьи
При эндоскопическом исследовании в случае бронхоэктазов в стадии ремиссии выявляется
частично диффузный бронхит I степени воспаления
Активируйте PUSH уведомления в браузер
Отключите PUSH уведомления в браузер
Содержание
Интернет магазин
Популярное
- О нас
- Правовые вопросы
- Политика
обработки персональных
данных EndoExpert.ru - Связаться с нами
- Стать партнером
© 2016-2022 EndoExpert.ru

Вы находитесь в разделе предназначенном только для специалистов (раздел для пациентов по ссылке). Пожалуйста, внимательно прочитайте полные условия использования и подтвердите, что Вы являетесь медицинским или фармацевтическим работником или студентом медицинского образовательного учреждения и подтверждаете своё понимание и согласие с тем, что применение рецептурных препаратов, обращение за той или иной медицинской услугой, равно как и ее выполнение, использование медицинских изделий, выбор метода профилактики, диагностики, лечения, медицинской реабилитации, равно как и их применение, возможны только после предварительной консультации со специалистом. Мы используем файлы cookie, чтобы предложить Вам лучший опыт взаимодействия. Файлы cookie позволяют адаптировать веб-сайты к вашим интересам и предпочтениям.
Я прочитал и настоящим принимаю вышеизложенное, хочу продолжить ознакомление с размещенной на данном сайте информацией для специалистов.














.jpg)


.png)















Комментарии