- Компании
- Takeda. О компании, буклеты, каталоги, контакты
- Olympus. О компании, буклеты, каталоги, контакты
- Boston Scientific. О компании, буклеты, каталоги, контакты
- Pentax. О компании, буклеты, каталоги, контакты
- Fujifilm & R-Farm. О компании, буклеты, каталоги, контакты
- Erbe. О компании, буклеты, каталоги, контакты
- Еще каталоги
- Мероприятия
- Информация
- Обучение
- Классификации
- Атлас
- Quiz
- Разделы
- Пациенту
QR-код этой страницы
Для продолжения изучения на мобильном устройстве ПРОСКАНИРУЙТЕ QR-код с помощью спец. программы или фотокамеры мобильного устройства
СанПин: INTERNATIONAL STANDARD ISO 15883-4
Полный текст статьи:
INTERNATIONAL STANDARD
ISO 15883-4
Second edition
2018-11
Washer-disinfectors —
Part 4:
Requirements and tests for washer- disinfectors employing chemical disinfection for thermolabile endoscopes
Laveurs désinfecteurs —
Partie 4: Exigences et essais pour les laveurs désinfecteurs destinés à la désinfection chimique des endoscopes thermolabiles
Reference number ISO 15883-4:2018(E)
Copyright International Organization for Standardization Provided by IHS Markit under license with ANSI
No reproduction or networking permitted without license from IHS
Order Number: 02223302
Sold to:CANTEL MEDICAL *DA [001612] - SMARTIN@MEDIVATORS.COM, Not for Resale,2018-12-18 15:39:13 UTC
© ISO 2018
ISO 15883-4:2018(E)
© ISO 2018
COPYRIGHT PROTECTED DOCUMENT
All rights reserved. Unless otherwise specified, or required in the context of its implementation, no part of this publication may be reproduced or utilized otherwise in any form or by any means, electronic or mechanical, including photocopying, or posting on the internet or an intranet, without prior written permission. Permission can be requested from either ISO at the address below or ISO’s member body in the country of the requester.
ISO copyright office
CP 401 • Ch. de Blandonnet 8 CH-1214 Vernier, Geneva Phone: +41 22 749 01 11 Fax: +41 22 749 09 47
Email: copyright@iso.org
Website: www.iso.org Published in Switzerland
Copyright Initiernational Organization for Standardization
Order Number: 02223302
© ISO 2018 – All rights reserved
Provided by IHS Markit under license with ANSI
No reproduction or networking permitted without license from IHS
Sold to:CANTEL MEDICAL *DA [001612] - SMARTIN@MEDIVATORS.COM, Not for Resale,2018-12-18 15:39:13 UTC
ISO 15883-4:2018(E)
Contents Page
5.4.4 WD with a minimum operating temperature for the washing and/or
Copyright International Org©anizIaStioOn fo2r S0ta1n8dar–dizAatiloln rights reserved
Provided by IHS Markit under license with ANSI
No reproduction or networking permitted without license from IHS
Order Number: 02223302
Sold to:CANTEL MEDICAL *DA [001612] - SMARTIN@MEDIVATORS.COM, Not for Resale,2018-12-18 15:39:13 UTC
ISO 15883-4:2018(E)
6.9.2 Test for operating cycle temperature limits on washing and chemical
6.12.5 Disinfection of liquid transport systems following failure of water
Annex B (normative) Microbiological testing of the efficacy of chemical disinfection of the load...40 Annex C (normative) Summary of test programmes ........................................................................................................................44
Copyright Initvernational Organization for Standardization
Order Number: 02223302
© ISO 2018 – All rights reserved
Provided by IHS Markit under license with ANSI
No reproduction or networking permitted without license from IHS
Sold to:CANTEL MEDICAL *DA [001612] - SMARTIN@MEDIVATORS.COM, Not for Resale,2018-12-18 15:39:13 UTC
ISO 15883-4:2018(E)
Annex D (normative) Methods for microbiological evaluation of disinfection of liquid
Annex F (informative) Additional notes on microbiological testing of chemical disinfection processes ...................................................................................................................................................................................................................55
--`,,,,````,``,,``,,,``,-`-``,```,,,`---
Copyright International Org©anizIaStioOn fo2r S0ta1n8dar–dizAatiloln rights reserved
Provided by IHS Markit under license with ANSI
No reproduction or networking permitted without license from IHS
Order Number: 02223302 v
Sold to:CANTEL MEDICAL *DA [001612] - SMARTIN@MEDIVATORS.COM, Not for Resale,2018-12-18 15:39:13 UTC
Foreword
ISO (the International Organization for Standardization) is a worldwide federation of national standards bodies (ISO member bodies). The work of preparing International Standards is normally carried out through ISO technical committees. Each member body interested in a subject for which a technical committee has been established has the right to be represented on that committee. International organizations, governmental and non-governmental, in liaison with ISO, also take part in the work. ISO collaborates closely with the International Electrotechnical Commission (IEC) on all matters of electrotechnical standardization.
The procedures used to develop this document and those intended for its further maintenance are described in the ISO/IEC Directives, Part 1. In particular, the different approval criteria needed for the different types of ISO documents should be noted. This document was drafted in accordance with the editorial rules of the ISO/IEC Directives, Part 2 (see www.iso.org/directives).
Attention is drawn to the possibility that some of the elements of this document may be the subject of patent rights. ISO shall not be held responsible for identifying any or all such patent rights. Details of any patent rights identified during the development of the document will be in the Introduction and/or on the ISO list of patent declarations received (see www.iso.org/patents).
Any trade name used in this document is information given for the convenience of users and does not
constitute an endorsement.
For an explanation of the voluntary nature of standards, the meaning of ISO specific terms and expressions related to conformity assessment, as well as information about ISO's adherence to the World Trade Organization (WTO) principles in the Technical Barriers to Trade (TBT) see www.iso
This document was prepared by Technical Committee ISO/TC 198, Sterilization of health care products.
This second edition cancels and replaces the first edition (ISO 15883-4:2008), which has been technically revised. The main changes compared to the previous edition are as follows:
— additional annexes for establishing endoscope type test groups and endoscope product families
have been included.
A list of all the parts in the ISO 15883 series can be found on the ISO website.
Any feedback or questions on this document should be directed to the user’s national standards body. A
complete listing of these bodies can be found at www.iso.org/members.html.
Copyright Invteirnational Organization for Standardization
Order Number: 02223302
© ISO 2018 – All rights reserved
Provided by IHS Markit under license with ANSI
No reproduction or networking permitted without license from IHS
Sold to:CANTEL MEDICAL *DA [001612] - SMARTIN@MEDIVATORS.COM, Not for Resale,2018-12-18 15:39:13 UTC
Introduction
This introduction is intended to be read in conjunction with the introduction to ISO 15883-1.
The washer-disinfectors specified in this document are intended to process devices that can be immersed in water or aqueous solutions. For some devices this will require that, prior to processing, relevant parts of the device are protected from immersion in accordance with the device manufacturer’s operating instructions.
Fields of application within the scope of the ISO series include laboratory, veterinary, dental and pharmaceutical applications and other specific applications, such as washer-disinfectors for bedsteads and transport carts and the disinfection of crockery and cutlery intended for use with immunologically compromised patients.
Requirements for washer-disinfectors for other applications are specified in other parts of ISO 15883. Safety requirements for washer-disinfectors are given in IEC 61010-2-040.
In respect of the potential adverse effects on the quality of water intended for human consumption caused by the washer-disinfector and its intended use, it is noteworthy that:
a) until verifiable international criteria are adopted, the existing national regulations concerning the use and/or characteristics of the washer-disinfectors remain in force, and
b) the ISO 15883 series provides no information as to whether the washer-disinfectors can be used
without restriction in any of the ISO member states.
|
© ISO 2018 – All rights reserved |
--`,,,,````,``,,``,,,``,-`-``,```,,,`---
Copyright International Organization for Standardization Provided by IHS Markit under license with ANSI
No reproduction or networking permitted without license from IHS
Order Number: 02223302
Sold to:CANTEL MEDICAL *DA [001612] - SMARTIN@MEDIVATORS.COM, Not for Resale,2018-12-18 15:39:13 UTC
vii
Copyright International Organization for Standardization Provided by IHS Markit under license with ANSI
No reproduction or networking permitted without license from IHS
Order Number: 02223302
Sold to:CANTEL MEDICAL *DA [001612] - SMARTIN@MEDIVATORS.COM, Not for Resale,2018-12-18 15:39:13 UTC
INTERNATIONAL STANDARD ISO 15883-4:2018(E)
Washer-disinfectors —
Part 4:
Requirements and tests for washer-disinfectors employing chemical disinfection for thermolabile endoscopes
1 Scope
This document specifies the particular requirements, including performance criteria for washer- disinfectors (WD) that are intended to be used for cleaning and chemical disinfection of thermolabile endoscopes.
This document also specifies the performance requirements for the cleaning and disinfection of the washer-disinfector and its components and accessories which can be required to achieve the necessary performance criteria.
The methods, instrumentation and instructions required for type testing, works testing, validation (installation, operational and performance qualification on first installation), routine control and monitoring, and requalification of WD periodically and after essential repairs, are also specified.
NOTE 1 In addition, Annex A gives guidance on an appropriate division of responsibility for the range of activities covered by this document.
NOTE 2 WD complying with this document can also be used for cleaning and chemical disinfection of other thermolabile re-usable medical devices for which the device manufacturer has recommended and validated this method of disinfection.
WD complying with the requirements of this document are not intended for cleaning and disinfection of medical devices, including endoscopic accessories, which are heat stable and can be disinfected or sterilized by thermal methods (see ISO 15883-1:2006+Amd 1:2014, 4.1.5).
The specified performance requirements of this document do not ensure the inactivation or removal of
the causative agent(s) (prion protein) of transmissible spongiform encephalopathies.
NOTE 3 If it is considered that prion protein might be present, particular care is needed in the choice of cleaning agents and disinfectants to ensure that the chemicals used do not react with the prion protein and/or other protein in a manner that can inhibit its removal or inactivation from the load or washer-disinfector.
NOTE 4 This document can be used by prospective purchasers and manufacturers as the basis of agreement on the specification of the WD, manufacturers of endoscopes, cleaning products, and disinfecting products.
2 Normative references
The following documents are referred to in the text in such a way that some or all of their content constitutes requirements of this document. For dated references, only the edition cited applies. For undated references, the latest edition of the referenced document (including any amendments) applies.
ISO 14971, Medical devices — Application of risk management to medical devices
ISO 15883-1:2006+Amd 1:2014, Washer-disinfectors — Part 1: General requirements, terms and definitions and tests
ISO/TS 15883-5:2005, Washer-disinfectors — Part 5: Test soils and methods for demonstrating cleaning efficacy
Copyright International Org©anizIaStioOn fo2r S0ta1n8dar–dizAatiloln rights reserved
Provided by IHS Markit under license with ANSI
No reproduction or networking permitted without license from IHS
Order Number: 02223302 1
Sold to:CANTEL MEDICAL *DA [001612] - SMARTIN@MEDIVATORS.COM, Not for Resale,2018-12-18 15:39:13 UTC
IEC 61010-2-040, Safety requirements for electrical equipment for measurement, control, and laboratory use — Part 2-040: Particular requirements for sterilizers and washer-disinfectors used to treat medical materials
EN 12353, Chemical disinfectants and antiseptics — Preservation of test organisms used for the determination of bactericidal (including Legionella), mycobactericidal, sporicidal, fungicidal and virucidal (including bacteriophages) activity
EN 13727, Chemical disinfectants and antiseptics — Quantitative suspension test for the evaluation of bactericidal activity in the medical area — Test method and requirements (phase 2, step 1)
3 Terms and definitions For the purposes of this document, the terms and definitions given in ISO 15883-1 and the following apply. ISO and IEC maintain terminological databases for use in standardization at the following addresses:
— ISO Online browsing platform: available at http://www.iso.org/obp
— IEC Electropedia: available at http://www.electropedia.org/
3.1
air break
physical separation in water supply pipes to prevent back flow from equipment [SOURCE: ISO 11139:2018, 3.8]
3.2
analyte
chemical substance that is the subject of chemical analysis [SOURCE: ISO 11139:2018, 3.12]
3.3
block
<endoscope> group of channels comprising part of an endoscope with specified lengths, diameters and
interconnections
[SOURCE: ISO 11139:2018, 3.30]
3.4
channel separator
<endoscope> device used to keep apart interconnected fluid pathways
EXAMPLE A device inserted in a trumpet valve cylinder where multiple channels meet in order to separate the air and water pathways in the air/water valve assembly.
[SOURCE: ISO 11139:2018, 3.40]
3.5
colony forming unit CFU
visible aggregation of microorganisms arising from a single cell or multiple cells
[SOURCE: ISO 11139:2018, 3.53]
3.6
disinfecting agent
physical or chemical agent used for disinfection [SOURCE: ISO 11139:2018, 3.83]
Copyright In2ternational Organization for Standardization
Order Number: 02223302
© ISO 2018 – All rights reserved
Provided by IHS Markit under license with ANSI
No reproduction or networking permitted without license from IHS
Sold to:CANTEL MEDICAL *DA [001612] - SMARTIN@MEDIVATORS.COM, Not for Resale,2018-12-18 15:39:13 UTC
ISO 15883-4:2018(E)
3.7
disinfection
process to inactivate viable microorganisms to a level previously specified as appropriate for a defined purpose
[SOURCE: ISO 11139:2018, 3.84]
3.8
endoscope connector
device to interface with the fluid entry port of a channel of an endoscope that, where applicable, includes the tubing connected to the channel irrigation system of the washer-disinfector
[SOURCE: ISO 11139:2018, 3.94]
3.9
endoscope leak test
set of actions to identify a loss of integrity
Note 1 to entry: The test is intended to establish that the surface covering the device and/or lining a device channel is intact to the extent necessary to maintain a slightly positive pressure.
[SOURCE: ISO 11139:2018, 3.95, modified — Note 1 to entry has been added.]
3.10
endoscope port
part of an endoscope to which the irrigation system of the washer-disinfector is connected to irrigate
all or part of a channel
[SOURCE: ISO 11139:2018, 3.96]
3.11
endoscope product family
group of endoscopes with comparable design, including the number, construction and purpose of the
different endoscope channels
[SOURCE: ISO 11139:2018, 3.97]
3.12
endoscope surrogate device
item designed to represent construction elements of endoscope specific characteristics affecting the flow conditions in endoscope channels
Note 1 to entry: Elements can include channel length and diameter, connectors, channel separators, port closures, return valves, etc.
[SOURCE: ISO 11139:2018, 3.98]
3.13
endoscope type test group
endoscopes for which the general channel design and specific characteristics affecting the flow
conditions in the endoscope are similar
Note 1 to entry: The general channel design includes lengths and diameters. Characteristics affecting the flow conditions in the endoscope are, for example, connectors, channel separators, port closures, return valves.
Note 2 to entry: Similar implies that small variations can be possible. Endoscopes that show small variations in channel specifications that do not lead to a significant variation in the flow and pressure characteristic through the channels could be in the same endoscope type test group.
[SOURCE: ISO 11139:2018, 3.99]
Copyright International Org©anizIaStioOn fo2r S0ta1n8dar–dizAatiloln rights reserved
Provided by IHS Markit under license with ANSI
No reproduction or networking permitted without license from IHS
Order Number: 02223302 3
Sold to:CANTEL MEDICAL *DA [001612] - SMARTIN@MEDIVATORS.COM, Not for Resale,2018-12-18 15:39:13 UTC
ISO 15883-4:2018(E)
3.14
inoculated carrier
supporting material on or in which a specified number of viable test microorganisms has been deposited [SOURCE: ISO 11139:2018, 3.144]
3.15
irrigation plan
<endoscope washer-disinfector> stipulated direction of flow of process fluids through the specified
channels of an endoscope
[SOURCE: ISO 11139:2018, 3.148]
3.16
liquid transport systems
<washer-disinfector> components of equipment used to store, pump or transport water and/or solutions, excluding pipework before the air break
[SOURCE: ISO 11139:2018, 3.154]
3.17
microbial inactivation factor
measured change in microbial population caused by the lethal effect of the disinfection or
sterilization process
Note 1 to entry: It is expressed as log10. [SOURCE: ISO 11139:2018, 3.173] 3.18
microbial reduction factor
extent to which the bioburden is reduced in tenfold increments
Note 1 to entry: It is expressed as log10.
Note 2 to entry: This can be caused by the combination of the microbial inactivation factor and the physical
removal of microorganisms.
[SOURCE: ISO 11139:2018, 3.174, modified — Note 2 to entry has been added.]
3.19
microbial resistance
ability of a microorganism or population of microorganisms to withstand a microbial reduction process
Note 1 to entry: This refers to resistance of microorganisms to disinfectants used in a WD. [SOURCE: ISO 11139:2018, 3.175, modified — Note 1 to entry has been added.] 3.20
minimum effective concentration
MEC
lowest concentration of a chemical or product, used in a specified process, that achieves a claimed activity
[SOURCE: ISO 11139:2018, 3.177]
3.21
minimum recommended concentration MRC
lowest concentration of a chemical or product specified for use in a process
[SOURCE: ISO 11139:2018, 3.178]
Copyright In4ternational Organization for Standardization
Order Number: 02223302
© ISO 2018 – All rights reserved
Provided by IHS Markit under license with ANSI
No reproduction or networking permitted without license from IHS
Sold to:CANTEL MEDICAL *DA [001612] - SMARTIN@MEDIVATORS.COM, Not for Resale,2018-12-18 15:39:13 UTC
3.22
obstruction
<endoscope channel> partial or complete blockage [SOURCE: ISO 11139:2018, 3.187]
3.23
port closure
<endoscope> device to close an endoscope port during processing in order to maintain the flow of process fluids throughout the length of the endoscope
EXAMPLE To close the suction valve port.
[SOURCE: ISO 11139:2018, 3.198]
3.24
self-disinfection cycle
operating cycle intended to disinfect all liquid transport systems’ piping, chamber(s), tanks and other components which come into contact with the water and/or solutions used for cleaning, disinfecting and rinsing the load
Note 1 to entry: The self-disinfection cycle is used without a load in a washer-disinfector.
[SOURCE: ISO 11139:2018, 3.249]
3.25
thermolabile
readily damaged by heat [SOURCE: ISO 11139:2018, 3.302]
3.26
washer-disinfector accessory
items or attachments, including connectors, required to process a medical device in a washer-disinfector [SOURCE: ISO 11139:2018, 3.320]
4 Performance requirements
4.1 General
4.1.1 The WD shall conform to ISO 15883-1:2006+Amd 1:2014 with the exception of the following
subclauses:
a) 4.2.3 (washing stage, modified by 4.3.3 of this document);
b) 4.3.1 (specification for thermal disinfection of the load carrier and chamber walls during a standard cleaning and disinfection cycle is not applicable to this document);
c) 4.3.3 (chemical and thermal disinfection, modified by 5.4 of this document);
d) 5.3.2.5 (microbial quality of final rinse water, modified by 4.5 of this document);
e) 5.11.4 (process verification, modified by 5.6 of this document);
f) 6.4.2.1 (test for quality of final rinse water – sampling, modified by 6.3 and Annex E of this document);
g) 6.5.6 (test for chamber venting to prevent pressurization by steam is not applicable to this
document);
Copyright International Org©anizIaStioOn fo2r S0ta1n8dar–dizAatiloln rights reserved
Provided by IHS Markit under license with ANSI
No reproduction or networking permitted without license from IHS
Order Number: 02223302 5
Sold to:CANTEL MEDICAL *DA [001612] - SMARTIN@MEDIVATORS.COM, Not for Resale,2018-12-18 15:39:13 UTC
ISO 15883-4:2018(E)
h) 6.8.2 (load temperature test, modified by 6.9.1 of this document);
i) 6.8.3 (chamber wall temperature test, replaced by 6.9.1 of this document);
j) 6.10.2 (cleaning efficacy test 1; modified by 6.11 of this document).
Means shall be provided to position temperature sensors for test purposes. Depending on the type of washer design the manufacturer can decide to follow ISO 15883-1:2006+Amd 1:2014, 5.1.11 or provide an alternative solution better fit to the purpose.
4.1.2 Each device, including any device channels and/or cavities, shall be processed by the WD as
follows:
a) leak testing (where appropriate) in accordance with 4.2;
b) cleaning (which may include several stages) in accordance with 4.3;
c) disinfecting in accordance with 4.4;
d) final rinsing in accordance with 4.5;
e) purging of rinse water in accordance with 4.6;
f) drying (when appropriate) in accordance with 4.7.
4.1.3 After the complete process in the WD the endoscope shall be safe for its intended use. The combination of the cleaning, disinfection and rinsing process shall be designed to achieve this condition, recognizing the high level of microbial and other contamination that might exist, see References [33],
[34] and [35]. It shall be necessary to take into account other factors such as the design of connectors. This capability shall be demonstrated during type testing for endoscopes that the WD is designed to process [see also 8 a), 8 b) and 8 c)].
Where the disinfection of the water supplied to the WD is performed by adding a low dosage of a disinfectant to the water, compliance with this document shall be demonstrated with and without the water disinfectant. Any variation in water disinfectant concentration due to local environmental conditions that might change the result of the test shall be taken into account.
Demonstration of the capability of the complete cycle efficacy shall be provided during additional type testing by employing a modification of the methods described in Annex B with added test soil and/or ISO/TS 15883-5:2005, Annex I, using the organism(s) previously established during in vitro tests as most resistant to the disinfectant under in-use conditions and on endoscopes that are representative for each relevant endoscope type test group [see 8 a) and Annex H].
According to the nature of the most resistant microorganism selected the minimum log10 reduction
obtained after a complete standard cycle for that microorganism(s) shall be:
— 9 log10 for vegetative bacteria;
— 6 log10 for fungal spores;
— 6 log10 for mycobacteria; or
— 4 log10 for bacterial endospores.
NOTE 1 In order to limit the work load the type tests can be performed on representative endoscopes from endoscope type test groups (see Annex H to establish relevant endoscope type test groups).
NOTE 2 The efficacy of the process (including cleaning and disinfection) depends on a number of factors which
include:
a) the nature (characteristics) of the device being processed;
b) the extent and nature of the soiling to be removed;
Copyright In6ternational Organization for Standardization
Order Number: 02223302
© ISO 2018 – All rights reserved
Provided by IHS Markit under license with ANSI
No reproduction or networking permitted without license from IHS
Sold to:CANTEL MEDICAL *DA [001612] - SMARTIN@MEDIVATORS.COM, Not for Resale,2018-12-18 15:39:13 UTC
c) the temperature of the process;
d) the mechanical energy (type, output);
e) purging to remove rinse water;
f) the detergent system;
g) the nature, volume, concentration and temperature of the cleaning and disinfectant solutions and their ability to wet the surfaces to be cleaned and disinfected;
h) the duration of the various process stages;
i) the removal of suspended soil.
4.1.4 The instructions for use of the WD shall recommend that the actions necessary to ensure effective and safe processing of the endoscope and its accessories in the WD be followed, e.g. leak testing, any pre- treatment, manual cleaning and/or disassembly, of the endoscope [see 8 k) 8)].
It shall be specified, which of the pre-treatment steps, as listed in the endoscope manufacturer’s processing instructions for use, shall be performed in order to ensure effective and safe processing of the endoscope.
NOTE National guidelines can require certain pre-cleaning steps (e.g. brushing of endoscopes channels prior
to processing inside WD).
4.1.5 The value of any process variable that affects the efficacy of the cycle shall be pre-set and adjustment shall require the use of a key, code or tool (see also ISO 15883-1:2006+Amd 1:2014, 5.18.3, 5.18.8 and 5.18.12).
4.1.6 The means to control the total volume of water admitted per stage shall be controlled to a
manufacturer defined level of accuracy.
4.1.7 The means to control the volume of process chemicals admitted shall deliver the set volume to an
accuracy of ± 5 % or better.
4.1.8 When the WD uses two or more different process chemicals, means other than labelling and/or colour coding alone of connectors, containers and/or tubing, shall be provided to ensure that connection is made to the correct container of process chemical.
4.1.9 The instructions for use of the WD shall include a recommendation that heat-stable endoscopic
accessories for thermolabile medical devices should be thermally disinfected and/or sterilized.
4.1.10 The design of the washer-disinfector or any device or washer-disinfector accessories provided with the WD shall not impair the quality of the water supplying the WD.
4.2.1 These requirements shall apply only to WD intended to process endoscopes that require a test to verify that the device is watertight.
NOTE This test is intended to demonstrate that the endoscope will not be damaged by liquid ingress during the WD operating cycle. It is regarded only as a test of the integrity of the endoscope when all parameters of the WD leak test (e.g. pressure, duration, maximum leak accepted) are consistent with those specified for the endoscope.
Copyright International Org©anizIaStioOn fo2r S0ta1n8dar–dizAatiloln rights reserved
Provided by IHS Markit under license with ANSI
No reproduction or networking permitted without license from IHS
Order Number: 02223302 7
Sold to:CANTEL MEDICAL *DA [001612] - SMARTIN@MEDIVATORS.COM, Not for Resale,2018-12-18 15:39:13 UTC
ISO 15883-4:2018(E)
4.2.2 The WD shall be provided with either:
a) means to carry out an automatic leak test on the endoscope which shall be completed before the load comes into contact with process fluids in the WD;
or
b) instructions for use that include the requirement to carry out the test manually prior to processing
through the WD.
NOTE 1 An alternative method specified for the endoscope can be used for determining the integrity of the
endoscope when appropriate.
NOTE 2 WD with an automatic leak test can include a user selectable option to repeat the leak test at the end of the process and/or independently of a normal process cycle.
NOTE 3 An automated leak test is the preferred option.
4.2.3 For WD having an automatic leak test, the automatic controller shall prevent the continuation of the operating cycle and operate an audible and visible alarm indicating a leak test failure if a leak is detected in an endoscope.
Variations in temperature that might adversely affect the sensitivity of the leak test and the temperature range permitted in the WD during the automatic leak test, if fitted, shall be stated [see 8 g)].
NOTE 1 A leak test failure indicates that the device is likely to be damaged by further processing. However, a satisfactory leak test does not provide absolute assurance that the device will not be damaged by further processing.
NOTE 2 An automatic leak test which maintains a positive pressure throughout the cycle can provide an additional safety level.
4.2.4 In WD provided with an automatic leak test:
a) the WD shall be designed so that the connectors provided for irrigation of the endoscope channel(s)
cannot be connected to the endoscope leak test connection port on the endoscope;
b) the connection system between the endoscope and the WD shall be designed so that the leak test
connector on the WD cannot be connected to the endoscope channel(s) to be irrigated;
c) the means used to monitor the pressure inside the device (e.g. pressure transducer) shall be independent from the means used to control the pressure applied to the endoscope to perform the leak test (e.g. pressure regulating valve);
d) the system used to pressurize the device during each leak test shall be provided with a means of preventing over-pressurization of the device in the event of failure of the pressure control system;
e) the extent and duration of pressurization and the pressure drop or air flow which will be used to indicate a failure shall be either in accordance with the device manufacturer’s instructions for the devices that the WD is intended to process, or independently verified.
4.2.5 For WD with an automatic leak test, means shall be provided to automatically warn the user with an audible and/or visible alarm after the initiation of the operating cycle if the leak test connectors are not connected to the endoscopes.
4.2.6 WD with an automatic leak test shall be tested in accordance with 6.5.
Copyright In8ternational Organization for Standardization
Order Number: 02223302
© ISO 2018 – All rights reserved
Provided by IHS Markit under license with ANSI
No reproduction or networking permitted without license from IHS
Sold to:CANTEL MEDICAL *DA [001612] - SMARTIN@MEDIVATORS.COM, Not for Resale,2018-12-18 15:39:13 UTC
4.3.1 General
All surfaces (internal and external) of the endoscope(s) which are required to be disinfected by the WD
shall be cleaned (see 6.11 of this document, and ISO 15883-1:2006+Amd 1:2014, 4.2.1.1, 5.1.10).
Some endoscope(s) have components (e.g. electronic connectors) that their manufacturer recommends cannot be immersed in water or aqueous solutions. These component parts should be processed in accordance with the manufacturer’s instructions and then protected from immersion during processing in the WD.
Cleaning shall comprise washing with a detergent solution that may, when necessary, be preceded by flushing. Washing shall be followed by rinsing unless the conditions specified in 4.3.4 have been met.
4.3.2 Flushing
When necessary, the WD shall provide means to flush the internal and external surfaces of the
endoscope.
NOTE Flushing before washing might be necessary to eliminate soils or to avoid any interaction between the chemicals used during pre-treatment and those of the WD processing cycle.
The flushing water or solution shall be discharged during or after each operating cycle and shall not be
re-used.
The detergent(s) to be used shall be specified, as established during type testing; additional detergents may be used if established by further type testing [see 8 n)].
The detergent solution shall be discharged during or after each operating cycle and shall not be re-used.
The temperature of the detergent solution throughout the washing stage shall be monitored to ensure that it remains within the specified limits of the detergent and be compatible with the temperature limits for the device(s) to be processed.
This shall be achieved either:
a) by controlling the temperature of the detergent solution;
or
b) where appropriate, by operating the WD at ambient temperature with a means of preventing operation of the WD when the detergent temperature is outside the specified temperature range.
Rinsing between washing and disinfection shall be used to reduce the concentration of residues (process chemicals and soiling including microbial contamination) to a level that does not impair the efficacy of the disinfection stage.
Rinsing shall take place between washing and disinfection unless it can be demonstrated that:
a) there is no adverse reaction between process chemicals being used for each of these stages;
b) there is no adverse reaction between suspended or residual soiling and the disinfectant that can compromise the disinfection stage.
The rinse water quality shall be specified. This shall be of, at least, potable quality [see 8 q)].
Copyright International Org©anizIaStioOn fo2r S0ta1n8dar–dizAatiloln rights reserved
Provided by IHS Markit under license with ANSI
No reproduction or networking permitted without license from IHS
Order Number: 02223302 9
Sold to:CANTEL MEDICAL *DA [001612] - SMARTIN@MEDIVATORS.COM, Not for Resale,2018-12-18 15:39:13 UTC
4.3.5 Determination of cleaning efficacy
Cleaning efficacy shall be determined in accordance with 6.11.
4.4.1 General
National regulatory requirements can specify approval procedures for disinfectants to be used in WD for medical devices. Compliance with these national requirements shall be deemed to meet the requirements of 4.4 within the territory where these requirements apply.
The capability of the WD to provide disinfection of the device shall be deemed to have been established if, when the WD is tested as specified in 6.12.6 under the specified conditions of disinfectant concentration, volume, temperature and contact time, the required microbial inactivation factor is attained (see 4.4.2.5).
The choice of disinfectant shall ensure that the spectrum of activity is appropriate for the intended use.
The efficacy of disinfectants can be seriously impaired by residual soiling, inorganic salts etc. remaining on the device(s) and therefore an effective cleaning prior to disinfection is necessary.
NOTE Other process chemicals, e.g. detergents can react with and seriously impair the activity of disinfectants if they are not removed before the disinfection stage.
4.4.2 Efficacy of the disinfectant
4.4.2.1 The following tests are based on the use of aqueous solutions of a disinfectant. Other systems,
e.g. based on gaseous disinfectants are not excluded; equivalent tests are required.
4.4.2.2 When tested in accordance with 6.12.2, the bactericidal, mycobactericidal, fungicidal and virucidal in vitro efficacy of the disinfectant shall be demonstrated with standardized test methods under the conditions of use in the WD and, if required by national regulations, at the MEC and mandatory test conditions (e.g. potency tests – see Note 1).
The disinfectant chosen shall also be active against bacterial endospores. The disinfectant should reduce the population of bacterial endospores by not less than 6 log10 within 5 h of exposure, or at an equivalent rate, under the use conditions.
NOTE 1 Demonstration by the disinfectant manufacturer that the disinfectant meets the above requirements can be made employing methods based on relevant published standards or other relevant publications, e.g. EN 13624, EN 13727, EN 14348, EN 14476, EN 14561, EN 14562, EN 14885, EN 14563, AOAC Use dilution test,
ASTM E2197 virucidal test, OECD Guideline.
NOTE 2 Suitable methods include the AOAC sporicidal test (method 966.04), ASTM E2111-05, EN 14347, EN 13704, etc.
NOTE 3 National regulatory authorities can require different inactivation values and test methods, in which case, the tests listed in Notes 1 and 2 might need to be modified to demonstrate efficacy.
4.4.2.3 A specific neutralization method for the disinfectant shall be validated in accordance with
NOTE These data can be provided by the disinfectant manufacturer.
4.4.2.4 Interfering substances
4.4.2.4.1 The experimental conditions of tests intended to demonstrate the microbicidal activity of
the disinfectant in vitro shall consider the conditions of use of the disinfectant, which should include
Copyright In1ter0national Organization for Standardization
Order Number: 02223302
© ISO 2018 – All rights reserved
Provided by IHS Markit under license with ANSI
No reproduction or networking permitted without license from IHS
Sold to:CANTEL MEDICAL *DA [001612] - SMARTIN@MEDIVATORS.COM, Not for Resale,2018-12-18 15:39:13 UTC
the effect on microbial efficacy of re-use, and if applicable the absence of rinsing between cleaning and
disinfection.
NOTE 1 National regulatory authorities can require rinsing between cleaning and disinfection. NOTE 2 EN 14885 provides examples of test conditions.
4.4.2.4.2 The efficacy of the disinfectant and the interaction between the disinfectant and residues (e.g. soil, detergents) shall be tested under conditions in which residues are at or above the maximum level that might occur in use and the disinfectant is at or below the minimum specified in-use concentration.
4.4.2.5 When tested in accordance with 6.12.6 for the minimum exposure time at the MRC and the minimum temperature to be used in the WD, the disinfection stage shall demonstrate:
— at least 6 log10 inactivation of the most resistant Mycobacterium sp. to the disinfectant. Variations in volume of water and disinfectant shall be considered.
NOTE National regulatory authorities can require testing on additional strains, and different
inactivation values.
The temperature of the disinfecting agent throughout the disinfection stage shall be monitored to ensure that it remains within the specified limits of the disinfectant and be compatible with the temperature limits for the device(s) to be processed.
![]()
This shall be achieved either by controlling the temperature of the disinfectant solution or, where appropriate, by operating the WD at ambient temperature with means to prevent operation of the WD when the disinfectant temperature is outside the specified temperature range.
The process monitoring of each operating cycle by the automatic controller shall include verification that the process conditions specified by the WD manufacturer as necessary and sufficient for disinfection to take place (e.g. disinfectant concentration, temperature and contact time) were attained (see also 5.5).
Microbial testing (e.g. with biological indicators or inoculated carriers) of the disinfection stage on each
cycle shall not be used to meet this requirement.
NOTE Confirmation of the concentration of disinfectant can require, for example, measurement of the volume of disinfectant and water admitted together with a certificate of conformity from the disinfectant supplier for the concentration of the disinfectant, together with data to support the shelf life, expiry date etc. (see also 4.4.5.2).
4.4.5.1 General
The disinfectant(s) to be used shall be specified, as established during type testing. Additional disinfectants may be used if established by further type testing [see 8 n)].
Disinfectant solutions shall either be discharged after a single use during each cycle or re-used for a limited number of cycles (see 4.4.5.2). Discharge after a single use, during each cycle, is the preferred option.
4.4.5.2 Re-use of disinfectant solutions
If the WD is designed to allow the same disinfectant solution to be used on two or more consecutive
operating cycles then steps shall be taken to ensure that the activity and safety (e.g. accumulation
Copyright International Org©anizIaStioOn fo2r S0ta1n8dar–dizAatiloln rights reserved
Provided by IHS Markit under license with ANSI
No reproduction or networking permitted without license from IHS
Order Number: 02223302 11
Sold to:CANTEL MEDICAL *DA [001612] - SMARTIN@MEDIVATORS.COM, Not for Resale,2018-12-18 15:39:13 UTC
of foreign material, device compatibility) of the disinfectant solution are not impaired during its working life.
This shall include the following:
a) Means shall be specified to ensure that the disinfectant solution has retained the required antimicrobial activity. These means shall be based on validation studies, which would normally be carried out by the disinfectant manufacturer, to determine a suitable parameter, or parameters, to be monitored to indicate the antimicrobial activity of the disinfectant. Suitable parameters include e.g. pH, stability, concentration of the active ingredient, and adjuvants that could also affect performance.
NOTE Minor changes in formulation of the disinfectant can have a significant effect on storage life, antimicrobial activity etc.
b) The maximum period or number of operating cycles for which the disinfectant may be used shall be recommended to the user. This shall be based on validated experimental data.
c) When validated use conditions (maximum period or number of operating cycles) are exceeded, the automatic controller shall operate an audible and visible alarm and prevent the use of the operating cycle until chemicals are changed.
It shall be recommended that the user monitors the disinfectant concentration using the method provided by the disinfectant manufacturer, e.g. an indicator test strip, specific for the disinfectant to show that the disinfectant is at or above the MRC (see also 4.4.4). It shall be recommended that the user replaces the disinfectant solution with fresh solution when it reaches its maximum number reuse days/ maximum number of operating cycles or the MRC, whichever comes first [see 4.4.5.2 c)].
4.5.1 The chemical purity of the final rinse water in contact with the load shall be specified.
When the water for the final rinse is disinfected by adding a chemical disinfectant to the water, it shall be demonstrated that residues of this disinfectant will not cause any harm to the user or the patient.
4.5.2 The final rinse water shall meet the requirements for microbiological quality as given in 4.9.2.3.
4.5.3 Depending upon the intended site of use of the endoscope (e.g. sterile body site) the level of bacterial endotoxins in the final rinse water shall be controlled and monitored within the limits specified in national regulations, using the method described in ISO 15883-1:2006+Amd 1:2014, 6.4.2.3.
NOTE It is the dose of endotoxin that ultimately impacts on the patient and this includes the exposure surface area of an endoscope as well as the endotoxin concentration in the final rinse water.
4.5.4 On completion of the final rinse stage the water shall not be stored for subsequent re-use in the rinsing stage of subsequent cycles.
4.6 Purging to remove rinse water
4.6.1 The WD shall include a means of purging rinse water from the channels of the endoscope(s) at
the end of the final rinse stage.
4.6.2 Whenever the channels of the device are purged with air, the air shall be oil free and shall be filtered through a filter, Class H13 or higher as specified in EN 1822-1:2009 (see ISO 15883-1:2006+Amd 1:2014,4.5.4).
NOTE This HEPA filter provides not less than 99,99 % arrestance to particles of 0,2 µm and larger.
Copyright In1ter2national Organization for Standardization
Order Number: 02223302
© ISO 2018 – All rights reserved
Provided by IHS Markit under license with ANSI
No reproduction or networking permitted without license from IHS
Sold to:CANTEL MEDICAL *DA [001612] - SMARTIN@MEDIVATORS.COM, Not for Resale,2018-12-18 15:39:13 UTC
4.7.1 Where the WD has no drying stage or has a user selectable drying stage, the instructions for use shall indicate that the device and the channels of the device shall be dried prior to storage in accordance with 8 k), 2).
NOTE 1 Automatic cycles in which the device is not dried are intended for use on devices which will be used
without storage.
NOTE 2 Purging with 0,2 µm filtered alcohol (e.g. 70 % isopropanol) can be used to aid drying, if compatible
with the medical device.
4.7.2 The quality of air used during the drying stage shall be at least that defined in 4.6.2.
4.7.3 When tested in accordance with 6.8 there shall be no visible droplets of moisture.
4.8.1 A self-disinfection cycle shall be provided to ensure that the WD does not become a focus for contamination of the load and to provide a means of disinfecting the WD after interventions for maintenance, repairs or testing (see also ISO 15883-1:2006+Amd 1:2014, 5.3.1.2).
NOTE 1 The self-disinfection process is intended also to deal with the situation where the WD has become contaminated. The piping used to convey rinse water to the endoscope, if contaminated, can easily develop a layer of biofilm containing many microorganisms in a state in which they are highly resistant to chemical disinfection.
NOTE 2 Thermal disinfection using moist heat is the preferred method. The temperature used can be higher
than the normal maximum operating temperature available for the loaded WD.
When chemical self-disinfection is used a disinfectant containing a disinfecting agent different from that used for disinfecting the endoscope or the same disinfectant under different conditions (e.g. formulation, increased temperature, higher concentration, extended contact time etc.) shall be used.
NOTE 3 The use of the same disinfecting agent used under the same conditions can carry the risk of allowing
organisms resistant to that particular disinfectant to proliferate.
4.8.2 A WD in which the endoscope process cycle provides for disinfection of the chamber and all piping and tanks which come into contact with the water or solutions used for cleaning, disinfecting and rinsing the load shall be deemed to meet this requirement (see 4.8.1) without the provision of an additional self-disinfection cycle. The standard cycles shall then be subject to the same test as the self- disinfection cycle (see 6.12.5).
4.8.3 Details of the parts of the WD subjected to the self-disinfection cycle and whether this cycle includes the water treatment equipment shall be provided [see 4.9 and 8 h)].
4.8.4 When different from the normal operating cycle the WD self-disinfection cycle shall:
a) be operated under the control of the automatic controller;
b) be a user selectable cycle;
c) provide for disinfection of the chamber and all liquid transport systems up to the air break;
d) include means to warn the user that the WD shall be operated without any load in the chamber and, so far as practicable, include means to verify that no device is present before the cycle will operate;
e) in the case of thermal self-disinfection of the WD, ensure that all the parts of the heating system and the associated pipework, via which the water or the steam reach the WD tank, attain an A0 value of at least 600.
Copyright International Org©anizIaStioOn fo2r S0ta1n8dar–dizAatiloln rights reserved
Provided by IHS Markit under license with ANSI
No reproduction or networking permitted without license from IHS
Order Number: 02223302 13
Sold to:CANTEL MEDICAL *DA [001612] - SMARTIN@MEDIVATORS.COM, Not for Resale,2018-12-18 15:39:13 UTC
4.8.5 The self-disinfection cycle shall ensure that a WD that has become contaminated through failure of the water treatment equipment can be effectively disinfected. Compliance shall be verified by testing in accordance with 6.12.5. After carrying out a self-disinfection cycle, the performance shall be deemed to be satisfactory if the final microbial count is 10 CFU/100 ml or fewer, and free from Pseudomonas aeruginosa in 100 ml, and if required for operational and routine testing, the sample is free from (atypical) Mycobacterium sp. in 100 ml (see 6.12.5).
NOTE Methods for microbiological evaluation of disinfection of the liquid transport system are specified in Annex D.
4.8.6 Thermal disinfection systems shall be evaluated by thermometric monitoring of the system with sensors placed at those parts of the system specified as representative of the lowest temperatures in the system. The entire system subjected to thermal disinfection shall attain the required disinfection temperature [see 8 l)].
4.8.7 For chemical disinfection systems a microbiological test shall be required. The test shall be designed to ensure that the self-disinfection cycle will disinfect contaminated tubing by evaluating the effect of the cycle against a biofilm containing Pseudomonas aeruginosa (see ISO/TS 15883-5:2005, Annex F). The capability of the WD to provide self-disinfection shall be deemed to have been established if, when tested in accordance with 6.12.3, the required microbial reduction factor has been achieved.
4.8.8 National regulatory requirements can specify approval procedures for validating self-disinfection of WD for medical devices. Compliance with these national requirements shall be deemed to meet the requirements of 4.8 within the territory where these requirements apply.
4.9.1 General
The water treatment equipment (softeners, de-ionizers, filters etc.) shall be operated within the specified limits (e.g. flow rates, supply pressures).
NOTE See ISO 15883-1:2006+Amd 1:2014, 5.23.
4.9.2 Disinfection of water treatment equipment
4.9.2.1 When the water treatment equipment is a part of the WD, the former shall be designed and constructed so that it can be periodically submitted to a disinfection procedure. Guidance on the minimum frequency with which the equipment shall be disinfected shall be stated according to the information supplied by the purchaser for the quality of the water supply and the manufacturer of the water treatment equipment [see 8 i)].
NOTE The disinfection of the water treatment equipment can be carried out during a self-disinfection cycle.
The actual frequency shall be specified based on, e.g. seasonal variations in the quality of water supplied to the WD and the operational history of the water treatment equipment.
The disinfection method shall not cause any damage to, nor impair the efficacy of, the treatment equipment.
The efficacy of the water treatment equipment disinfection procedure to provide self-disinfection shall be deemed to have been established when tested in accordance with the methods given in 6.12.4 and 6.12.5. There shall be less than 10 CFU recovered from each of the two 100 ml samples and other controlling parameters shall be achieved.
Copyright In1ter4national Organization for Standardization
Order Number: 02223302
© ISO 2018 – All rights reserved
Provided by IHS Markit under license with ANSI
No reproduction or networking permitted without license from IHS
Sold to:CANTEL MEDICAL *DA [001612] - SMARTIN@MEDIVATORS.COM, Not for Resale,2018-12-18 15:39:13 UTC
4.9.2.2 If the water treatment equipment is not part of the WD, then the requirements for water supplied to the WD shall be specified. This shall include specification of the permissible microbial contamination of the water supply [see 4.3.4 and 8 p)].
NOTE To meet the specification of the permissible microbial contamination of the water supply, it can be necessary to make provision for maintenance of the external water treatment equipment (e.g. filter replacement, disinfection, ultraviolet sources, calibration of dosing system).
4.9.2.3 Means shall be provided to disinfect incoming water used for the final rinse. The disinfection
process shall ensure that:
a) there are less than 10 CFU/100 ml sample of final rinse water when tested in accordance with
E.3.2; and
b) the water is free from Pseudomonas aeruginosa in 100 ml, and (atypical) Mycobacterium sp. in 100 ml when tested in accordance with E.3.3 (see 6.3).
NOTE The following methods can be suitable for control of the microbial contamination of rinse water. The rinse water will be:
— maintained in a dedicated reservoir at a temperature not less than 65 °C for the time demonstrated to
achieve disinfection of the incoming supply; or
— disinfected immediately prior to use; or
— filtered to remove suspended particles of a size greater than 0,2 µm; or
— sterile, in a closed container, with a connection to the WD designed and constructed to provide aseptic
transfer.
4.9.2.4 The connection between the water supply, which has been treated to remove microbial contamination, and the circulation system for rinsing the endoscope, shall be designed and constructed to prevent recontamination of the water.
Provision shall be made for disinfection of this connection to be made periodically. The frequency and method of carrying out this disinfection shall be specified [see 8 h) and 8 i)].
4.9.2.5 If the water treatment equipment is part of the WD, then where possible, the final rinse water treatment used to fulfil the requirements of 4.5 shall be monitored by the WD automatic controller to verify that the parameters affecting the efficacy of the water treatment equipment remain within specification. If the monitoring cannot be done by the automatic controller, then all the parameters to be verified during validation and routine monitoring shall be specified [see 8 s)].
The planned preventive maintenance required on the piping that is part of the WD and is used to convey final rinse water to the endoscope shall be specified. This shall include the frequency at which such piping should be replaced [see 8 m)].
5 Mechanical and process requirements
5.1 Materials ― Design, manufacture and construction
5.1.1 The maximum temperature of any process fluid in contact with the load shall be controlled below the temperature that would cause degradation of the device(s) which the WD is intended to process (see ISO 15883-1:2006+Amd 1:2014, 4.1.4).
Copyright International Org©anizIaStioOn fo2r S0ta1n8dar–dizAatiloln rights reserved
Provided by IHS Markit under license with ANSI
No reproduction or networking permitted without license from IHS
Order Number: 02223302 15
Sold to:CANTEL MEDICAL *DA [001612] - SMARTIN@MEDIVATORS.COM, Not for Resale,2018-12-18 15:39:13 UTC
5.1.2 The load carrier intended to accommodate the device(s) to be processed shall be designed and constructed to minimize the possibility of damage to the device(s) at the time of loading, during processing and during the course of unloading.
5.2 Device channel irrigation system
5.2.1 General
5.2.1.1 The connectors for each of endoscopes that the WD is designed to process shall be provided [see 8 a) and 8 b)]. The connectors shall be of the same design as the connectors used in the type testing of the WD.
NOTE 1 Connectors from a source other than the WD manufacturer might not be of the same design as the connectors used in the type test. The type test results might therefore not be valid when these third party connectors are used, and this can result in an inadequately processed endoscope.
During at least part of each of the cleaning, disinfection and rinsing stages, the device channel irrigation system shall ensure that the various process fluids flow through each of the internal channels and/or cavities of the devices that are required to be cleaned and disinfected. Assurance that this has taken place shall be provided either by:
a) the automatic controller providing means to verify the flow of process fluids through each channel
(see 5.2.2);
or
b) requiring in the instructions for use that the user:
1) verifies that all channels allow the free passage of process fluids before the device is loaded
into the WD;
2) confirms that all necessary connections were made before, and were still in place at the end of the cycle;
3) confirms by reference to the WD process record that the supply of process fluids was
maintained during each stage of the process (see 5.6);
4) verifies flow through each endoscope channel at the end of each operational cycle or immediately before use.
For some endoscopes the automatic flow verification system might not work properly due to technical limitations. Those endoscope lumens and devices shall be clearly identified [see 8 a)] and prescribed that for these particular endoscopes the user reverts to method b) to verify the irrigation of the channels.
NOTE 2 Option a) above is the preferred method. Option b) will burden the user with additional requirements for staff training, and staff resources needed to perform these additional steps in processing. Further, it will likely increase the incidence of user error and will degrade the quality and completeness of independent documentation that the process was completed correctly.
5.2.1.2 A diagram shall be provided of the circulation pathway of the fluids for all channels of each medical device that the WD is intended to process (see 4.1.2) based on information from the manufacturer of each device [see 8 j)].
Where an endoscope is part of an existing endoscope type test group, it shall be sufficient to provide a flow diagram for that endoscope type test group (see Annex H).
The flow diagram and/or instructions shall show any limitations on how, or to which endoscope port on the WD, the endoscope channels shall be connected [see 8 r)].
Copyright In1ter6national Organization for Standardization
Order Number: 02223302
© ISO 2018 – All rights reserved
Provided by IHS Markit under license with ANSI
No reproduction or networking permitted without license from IHS
Sold to:CANTEL MEDICAL *DA [001612] - SMARTIN@MEDIVATORS.COM, Not for Resale,2018-12-18 15:39:13 UTC
5.2.1.3 Minimum and maximum flow and maximum pressure that the WD is designed to deliver to each channel or channel system shall be specified. If the WD is intended to process a specific medical device then the specified maximum pressure(s) and flow(s) shall not be exceeded [see 8 d)].
In cases where different channels are irrigated at different pressures, the connection systems shall be
designed to prevent incorrect connections.
5.2.2 Verification of device channel irrigation by the automatic controller
5.2.2.1 The maximum extent of flow reduction permissible (e.g. change in flow volumes, pressures, rates) that will not impair the efficacy of the process for each channel or channel systems shall be specified [see 8 e)].
To enable determination of the flow that will occur through the unobstructed channels of the medical device, relevant data shall be obtained, e.g. dimensions of connectors, internal dimensions of channels, and maximum pressures to which channels may be subjected.
When one or more channels of the device are obstructed to an extent that would impair the efficacy of the process, the automatic controller shall cause a fault to be indicated.
Compliance with this requirement shall be demonstrated by testing in accordance with 6.6.
NOTE With some designs of endoscope a blockage in one channel could cause the flow to be diverted to another channel or endoscope port. Under these circumstances detection of an obstruction by the automatic controller might not be reliable. The user might need to refer to the device manufacturer’s instructions for the method to be used to verify that all channels are free from obstructions.
5.2.2.2 When one or more channels of the device are not connected to the WD, the automatic controller
shall cause a fault to be indicated.
Compliance with this requirement shall be demonstrated by testing in accordance with 6.7.
5.2.2.3 The automatic controller shall verify that the duration of flow of the relevant process fluids met or exceeded the minimum exposure times established during type testing as necessary for each process stage. Failure to achieve the required flow shall cause a fault to be indicated.
5.2.2.4 When there is a common connection for fluid at the same supply pressure to more than one channel, evidence shall be provided that the flow through each of the channels meets, or exceeds, the minimum required for effective cleaning, disinfection and rinsing of each device channel to be processed.
5.3 Venting and drainage systems
The WD shall be designed and constructed to ensure that there is no noxious discharge as specified in
IEC 61010-2-040.
NOTE Attention is drawn to local regulations concerning the concentration of process chemicals discharged
to waste and the temperature of drain effluent.
Throughout the operating cycle, when tested as specified in 6.9.1, the temperature recorded on the surface of the chamber and on all surfaces of the device being processed shall be within the specified operating temperature range for each stage of the operating cycle.
--`,,,,````,``,,``,,,``,-`-``,```,,,`---
Copyright International Org©anizIaStioOn fo2r S0ta1n8dar–dizAatiloln rights reserved
Provided by IHS Markit under license with ANSI
No reproduction or networking permitted without license from IHS
Order Number: 02223302 17
Sold to:CANTEL MEDICAL *DA [001612] - SMARTIN@MEDIVATORS.COM, Not for Resale,2018-12-18 15:39:13 UTC
5.4.2 Temperature control of the washing stage
Throughout the washing stage, when tested as described in 6.9.1, the temperature recorded on the surface of the chamber and on all surfaces of the device being processed shall be within the specified washing temperature band. If the temperature band is wider than 5 °C, the efficacy of the washing stage shall be demonstrated during type testing at the minimum and maximum temperature of the specified washing stage temperature band.
The temperature during washing stage shall be within the limits specified for the detergent(s) and
compatible endoscopes.
5.4.3 Temperature control of the disinfection stage
Throughout the disinfection stage, when tested as described in 6.9.1, the temperature recorded on the surface of the chamber and on all surfaces of the device being processed shall be within the specified disinfection temperature band. If the temperature band is wider than 5 °C, the efficacy of the disinfection stage shall be demonstrated during type testing at the minimum and maximum temperature of the specified disinfection stage temperature band.
The temperature during the disinfection stage shall be within the limits specified for the disinfectant(s)
and compatible endoscopes.
5.4.4 WD with a minimum operating temperature for the washing and/or disinfection stage
Throughout the washing and/or disinfection stage, when tested as described in 6.9.2, a fault shall be indicated when the temperature on the surface of the chamber and of the liquid process medium are below the minimum temperature specified for the device.
The conditions of use (temperature, concentration etc.) within the WD for all process chemicals (detergent, disinfectant etc.) shall be within their specified limits.
Where required for testing purposes the method(s) to be used to neutralize the process chemical (e.g. to stop any further anti-microbial activity) shall be obtained for that process chemical(s) and be made available to the user.
NOTE These data can be provided by the process chemical manufacturer.
The WD shall be fitted with means to verify and record the attainment of the specified process conditions. The conditions critical to the satisfactory outcome of the process shall be determined during type testing and shall be based on a documented risk analysis in accordance with ISO 14971. The critical process conditions shall be verified and recorded by the process verification system. The process verification system shall operate independent of the process controller with separate sensors. The signals from these sensors shall be processed in separate signal processing systems or in separate tasks in a single processing system.
NOTE 1 A process verification system in accordance with ISO 15883-1:2006+Amd 1:2014, 5.11.4 c) is deemed to meet these requirements.
NOTE 2 The control sensor and the verification sensor can be linked to the same control system provided that the signal treatment of each sensor is treated by distinct software tasks.
Copyright In1ter8national Organization for Standardization
Order Number: 02223302
© ISO 2018 – All rights reserved
Provided by IHS Markit under license with ANSI
No reproduction or networking permitted without license from IHS
Sold to:CANTEL MEDICAL *DA [001612] - SMARTIN@MEDIVATORS.COM, Not for Resale,2018-12-18 15:39:13 UTC
For those WD in which the required dose of process chemical is contained in a single-dose container which is replaced before each cycle, means shall be provided to ensure that the intended volume has been dispensed.
When tested in accordance with 6.10 there shall be an indication of a fault.
For WD in which process chemicals are supplied in multi-dose containers, ISO 15883-1:2006+Amd 1:2014,
5.7 applies.
6 Testing for conformity
6.1 General
The tests described in this clause are in addition to the tests described in ISO 15883-1 and are specific for WD intended to process thermolabile endoscopes. They are reference tests intended for use in demonstrating compliance with the specified requirements of this document. They may be used in type tests, works tests and in validation and requalification tests, or in routine tests carried out by, or on behalf of, the user. Other tests and methods providing equivalent assurance may be used by the manufacturer as the basis of claiming compliance with this document. In any case of dispute the reference tests given in this document shall be used. If the performance of the WD is reduced due to tolerance variations within the specified acceptable range the worst-case condition shall be used for type testing only.
NOTE 1 Examples of worst-case conditions include minimal flow per channel, process chemical(s) at end of shelf life, MEC or MRC, minimum temperature, etc.
The summary of tests in addition to those given in ISO 15883-1 is shown in Annex C.
NOTE 2 A number of the tests can be carried out simultaneously with each other and/or with those required by IEC 61010-2-040.
6.2 Test equipment
6.2.1 General
The equipment specified is external to the WD and intended for use in testing the WD. The overall accuracy of the system chosen shall be such that the error is less than ± 2 % of the value to be measured unless otherwise specified for the specific measuring system.
6.2.2 Pressure measurement
The sensor and/or measuring system shall be temperature compensated. The sensor error shall not exceed 0,25 % of full scale deflection.
The recorder for pressure measurement shall have an overall limit of error not exceeding 1 % of the maximum specified operating pressure for the variable being measured.
6.2.3 Flow measurement
6.2.3.1 Water
ISO 15883-1:2006+Amd 1:2014, 6.4.4 applies.
--`,,,,````,``,,``,,,``,-`-``,```,,,`---
Copyright International Org©anizIaStioOn fo2r S0ta1n8dar–dizAatiloln rights reserved
Provided by IHS Markit under license with ANSI
No reproduction or networking permitted without license from IHS
Order Number: 02223302 19
Sold to:CANTEL MEDICAL *DA [001612] - SMARTIN@MEDIVATORS.COM, Not for Resale,2018-12-18 15:39:13 UTC
6.2.3.2 Process chemical
ISO 15883-1:2006+Amd 1:2014, 6.9 applies.
6.3 Water used for final rinsing
6.3.1 Principle
The water used for final (post-disinfection) rinsing shall conform to 4.9.2.3 and E.3.2. In addition, any
growth shall be characterized.
6.3.2 Material/procedure
The water shall be tested for total viable count, and the presence of Pseudomonas aeruginosa and
(atypical) Mycobacterium sp. at the point of discharge into the WD chamber in accordance with Annex E.
NOTE Tests for other microorganisms that can be of clinical significance might also need to be performed.
(e.g. gram-negative Enterobacteriaceae, Legionella sp).
Where residual detergent or disinfectant is present it is necessary to use a neutralization method to eliminate any antimicrobial activity (see 5.5).
6.3.3 Results/acceptance criteria
Results shall be recorded as the number of colony forming units per 100 ml of water for the total viable count and the presence or absence of Pseudomonas aeruginosa in 100 ml, and (atypical) Mycobacterium spp. in 100 ml.
It is recommended that the tests be carried out after installation and at regular intervals thereafter. Until it has been established that the water supply is consistently within specification, these tests may be performed approximately weekly, then at less frequent intervals thereafter.
6.4 Hardness of water used during type testing
6.4.1 Principle
6.4.1.1 If the limit of hardness for water supplied to the WD is specified (see ISO 15883-1:2006+Amd 1:2014, 5.23.1), type tests shall be performed using water of the specified hardness. The water hardness shall be recorded.
6.4.1.2 When no limit is specified hard water for dilution of detergents or disinfectants shall be prepared as follows and used as the water supply to the WD during type testing to verify conformity with this document.
a) Solution A:
— MgCl2 anhydrous: 19,84 g;
— CaCl2 anhydrous: 46,24 g;
— sterile purified water: to 1 l;
— sterilize at 121 °C, 15 min.
b) Solution B:
— NaHCO3: 35,02 g;
Copyright In2ter0national Organization for Standardization
Order Number: 02223302
© ISO 2018 – All rights reserved
Provided by IHS Markit under license with ANSI
No reproduction or networking permitted without license from IHS
Sold to:CANTEL MEDICAL *DA [001612] - SMARTIN@MEDIVATORS.COM, Not for Resale,2018-12-18 15:39:13 UTC
— sterile purified water to 1 l;
— sterilize by filtration.
6.4.3 Procedure
Put not less than 600 ml of sterile purified water into a sterile 1 000 ml volumetric flask, add 6 ml of solution A and 8 ml of solution B and make up to 1 000 ml with sterile purified water.
Adjust the pH of the solution to 7,0 ± 0,2 using sodium hydroxide or hydrochloric acid as necessary.
NOTE 1 800 ml of hard water as prepared above, plus 200 ml of the disinfectant solution gives a final solution
containing 300 mg CaCO3/ l.
NOTE 2 National regulatory authorities can specify water hardness concentration for disinfectant efficacy
testing.
6.5.1 Principle
This test is based on the use of a test piece.
NOTE The test piece might not adequately represent all possible types of endoscope.
6.5.2 Material
6.5.2.1 Test piece, consisting of a length of tubing terminated at one end with a connector suitable for connection to the WD and at the other end with a flow control valve; the internal volume of the tube shall be within ± 10 % of the internal volume of the largest endoscope that the WD is intended to process.
6.5.2.2 Pressure transducer (sensor), capable of reading to ± 1 mbar (±0,1 kPa) over the range of the system’s operating pressure.
6.5.3 Procedure
6.5.3.1 Calibration
Verify the calibration of the pressure transducer (sensor).
6.5.3.2 Testing the pressure relief device
Connect the test piece (see 6.5.2.1) to the WD with the flow control valve fully closed. The pressure regulation system shall be disabled. Initiate the leak test. Record the pressure at which the pressure relief system operates as pmax.
6.5.3.3 Testing the leak tester fault and pass conditions
6.5.3.3.1 Fault condition
Connect the test piece to the leak tester and activate the leak test procedure in order to reach the leak
test pressure level (p1).
Open the flow control valve on the test piece in order to allow the pressure to drop to a level of ∆p > 0,8
(p2 – p3) in the leak test period (t3 – t2).
Copyright International Org©anizIaStioOn fo2r S0ta1n8dar–dizAatiloln rights reserved
Provided by IHS Markit under license with ANSI
No reproduction or networking permitted without license from IHS
Order Number: 02223302 21
Sold to:CANTEL MEDICAL *DA [001612] - SMARTIN@MEDIVATORS.COM, Not for Resale,2018-12-18 15:39:13 UTC
6.5.3.3.2 Pass condition
Connect the test piece to the leak tester and activate the leak test procedure in order to reach the leak test pressure level (p1). Open the flow control valve on the test piece in order to allow the pressure to drop to a level of ∆p ≤ 0,8 (p2 – p3) in the leak test period (t3 – t2).
6.5.3.4 Leak test for non-connection
Connect an endoscope to the WD, except for the leak test connector. Initiate an operating cycle.
6.5.4 Results/acceptance criteria
6.5.4.1 Verification of testing the pressure relief device (see 6.5.3.2)
Verify that the pressure (p) does not exceed the specified maximum pressure (pmax). (See 4.2.1 NOTE).
6.5.4.2 Verification of testing the leak tester “fault” and “pass” conditions
6.5.4.2.1 Fault condition
Verify from readings taken from the pressure transducer that a fault condition has been indicated.
Copyright In2ter2national Organization for Standardization
Order Number: 02223302
© ISO 2018 – All rights reserved
Provided by IHS Markit under license with ANSI
No reproduction or networking permitted without license from IHS
Sold to:CANTEL MEDICAL *DA [001612] - SMARTIN@MEDIVATORS.COM, Not for Resale,2018-12-18 15:39:13 UTC
ISO 15883-4:2018(E)
6.5.4.2.2 Pass condition
Verify that the WD indicates a pass condition. The leak test criteria can be shown as a pressure/time graph as shown in Figure 1. Verify from readings taken from the pressure transducer that a pass condition has been produced.
Figure 1 — Pressure versus time graph for leak test
NOTE With the pump, or other air supply, in continuous operation the pressure relief system prevents the
endoscope being pressurized above pmax.
Then the leak rate test pass criteria shall be in accordance with Formula (1):
(t3 - t 2 )
Key to Figure 1 and Formula (1).
po atmospheric pressure;
p1 pressure to which the endoscope is pressurized for the leak test;
p2 pressure after an initial equilibration period;
p3 pressure at the end of the leak test period;
pmax pressure at or below which the pressure relief system should operate;
to start of leak test;
t1 start of the leak test equilibration period;
t2 start of the leak test pressure monitoring period;
t3 end of the leak test pressure monitoring period;
Δp/t the maximum rate of leakage permitted for processing to continue.
6.5.4.3 Verification of leak test for non-connection (see 6.5.3.4)
Record whether or not a warning was indicated.
(1)
Copyright International Org©anizIaStioOn fo2r S0ta1n8dar–dizAatiloln rights reserved
Provided by IHS Markit under license with ANSI
No reproduction or networking permitted without license from IHS
Order Number: 02223302 23
Sold to:CANTEL MEDICAL *DA [001612] - SMARTIN@MEDIVATORS.COM, Not for Resale,2018-12-18 15:39:13 UTC
6.6 Channels non-obstruction test
6.6.1 Principle
The test is intended to determine the correct functioning of the system for detecting that channels
within the device are not obstructed.
Surrogate devices conforming to Annex H are used for the type test. See Annex G for typical specifications of trumpet valves and connection ports.
Each channel is provided with a means to place obstructions in the channels. The position of the obstructions shall be defined depending on the construction of the surrogate device. See Figure 2 for illustrations of obstruction positions.
a) Block A2 (see Table H.2)
Key
A air/water valve cylinder
B water bottle connector
C distal end
D air connector
1, 2, 3, 4, 5 positions of obstructions and test pieces for cleaning and disinfection testing using connection points
Copyright In2ter4national Organization for Standardization
Order Number: 02223302
© ISO 2018 – All rights reserved
Provided by IHS Markit under license with ANSI
No reproduction or networking permitted without license from IHS
Sold to:CANTEL MEDICAL *DA [001612] - SMARTIN@MEDIVATORS.COM, Not for Resale,2018-12-18 15:39:13 UTC
b) Block B2 (see Table H.2)
Key
A suction valve cylinder
B suction port
C distal end
D biopsy port
6, 7, 8, 9 positions of obstructions and test pieces for cleaning and disinfection testing using connection points
Figure 2 — Examples for placement of obstructions based on Annex H, Table H.2
For each endoscope type test group defined according to Annex H, the test shall be performed with a surrogate device representative of that endoscope type test group.
For WD on which the automatic controller includes provision to detect obstructed channels (see 5.2.2) repeat the operating cycle with the surrogate device with obstruction of one channel in order to reach the minimum flow specified [see 5.2.2.1 and 8 e)]. Repeat this test so that each available channel in turn has been obstructed.
NOTE National regulatory authorities can require these tests.
If operational and/or routine testing is necessary according to the instructions of the WD manufacturer
then this procedure should be followed.
6.6.4 Results/acceptance criteria
Record whether or not a fault was indicated when each channel was obstructed.
If the automatic controller is not able to detect a specific obstruction then this shall be indicated in the
instructions for use with reference to the applicable endoscope(s).
Endoscopes that belong to an endoscope type test group for which the channels non-obstruction test was not successful, shall be identified in the compatibility list [see 8 a)], or in the user manual, or by any other means.
6.7 Channels non-connection test
6.7.1 Principle
All channels of a surrogate device or an endoscope from a model representative of each endoscope type test group are connected to the channel irrigation system of the WD. Channels are disconnected one by one in order to verify if a fault is indicated.
Copyright International Org©anizIaStioOn fo2r S0ta1n8dar–dizAatiloln rights reserved
Provided by IHS Markit under license with ANSI
No reproduction or networking permitted without license from IHS
Order Number: 02223302 25
Sold to:CANTEL MEDICAL *DA [001612] - SMARTIN@MEDIVATORS.COM, Not for Resale,2018-12-18 15:39:13 UTC
6.7.2 Material
Testing shall be done using a surrogate device or an endoscope from a model representative of each endoscope type test group (see Annex H) and where all connections of the channel irrigation system of the WD can be connected.
6.7.3 Procedure
Place the surrogate device or the endoscope into the WD and connect all channels to the channel
irrigation system of the WD. Disconnect one of the channels and start the operating cycle. Repeat the operating cycle with every other channel of the endoscope.
6.7.4 Result/acceptance criteria
Record whether or not a fault was indicated when each channel in turn was not connected.
For testing, if the automatic controller is not able to detect a specific non-connection then this shall be
indicated within the instructions for use with reference to the applicable endoscope(s).
6.8.1 Principle
WD designed to dry the endoscope (interior and exterior surfaces) shall be tested using the test methods specified in 6.8.3 and 6.8.4.
6.8.2 Material
6.8.2.1 Anhydrous Copper (II) sulfate paper.
6.8.2.2 Compressed air.
6.8.3.1 Procedure
Carry out a normal operating cycle with an endoscope relevant to each endoscope type test group. Immediately, at the end of the recommended drying period (see 4.7), use a piece of anhydrous copper (II) sulfate paper to test the presence of moisture on the load exterior surfaces. When removing the load from the WD, and as the individual load items are being inspected, observe and record any water being discharged. Examine the paper for colour change (i.e. anhydrous copper (II) sulfate paper from white or light blue to deep blue) as evidence of residual water.
Place a piece of anhydrous copper (II) sulfate paper in any crevice between the control knobs on the endoscope housing or any crevices where water can linger (e.g. valve housing) and subsequently check the paper for blue spots.
NOTE 1 This test can be used for routine testing but in this case the endoscopes used are required to be
processed before patient use.
NOTE 2 The test is intended to be performed in the worst-case scenario with the most challenging load in the WD.
6.8.3.2 Result/Acceptance criteria
Record if residual water was observed or not.
Copyright In2ter6national Organization for Standardization
Order Number: 02223302
© ISO 2018 – All rights reserved
Provided by IHS Markit under license with ANSI
No reproduction or networking permitted without license from IHS
Sold to:CANTEL MEDICAL *DA [001612] - SMARTIN@MEDIVATORS.COM, Not for Resale,2018-12-18 15:39:13 UTC
There shall be no blue spots on the anhydrous copper (II) sulfate paper.
6.8.4.1 Procedure
At the end of the drying stage, the endoscope or surrogate relevant to each endoscope type test group (see Annex H) shall be removed from the WD. Direct the distal end of the endoscope towards a horizontal piece of anhydrous copper (II) sulfate paper at a distance of 50 mm to 100 mm and flush medical grade air at a positive pressure up to 120 kPa through each channel system. The full length of each channel in each endoscope shall be tested.
NOTE 1 For type testing compressed air is sufficient (see 4.6.2).
NOTE 2 The sensitivity of the test can be increased by pre-wetting the paper with > 99,97 % isopropanol.
6.8.4.2 Result/Acceptance criteria
Record if residual water was observed or not.
There shall be no blue spots on the anhydrous copper (II) sulfate paper.
6.9.1 Test for chamber and load temperature during operating cycle
6.9.1.1 Principle
The temperature on the surface of the chamber and on all surfaces of the load being processed are recorded during an operating cycle to verify if they are within the specified operating temperature range for each stage of the operating cycle.
Temperature sensors complying with ISO 15883-1:2006+Amd 1:2014, 6.2.1 but with the overall diameter such that the temperature sensor(s) within the channels of the endoscope(s) do not reduce the flow to an extent that impairs the efficacy of the process (see 5.2.2.1).
Locate the temperature sensors (6.9.1.2) as follows:
a) at two diagonally opposite positions in the chamber;
b) one in the approximate geometric centre of the surface of the door or lid;
c) one adjacent to each automatic control temperature sensor;
d) one adjacent to each process recorder temperature sensor;
e) one on the control head of the endoscope in contact with a metal component;
f) one in at least one channel of the endoscope at the distal end to a depth of not less than 100 mm;
g) the remaining sensors on the outer surface of the insertion tube and umbilical cord of the endoscope
at intervals not exceeding 750 mm.
© ISO--2`,,0,,`1```8,``,–,``A,,,l``l,-r`-i``g,`h``,t,,s`--r-eserved 27
Copyright International Organization for Standardization Provided by IHS Markit under license with ANSI
No reproduction or networking permitted without license from IHS
Order Number: 02223302
Sold to:CANTEL MEDICAL *DA [001612] - SMARTIN@MEDIVATORS.COM, Not for Resale,2018-12-18 15:39:13 UTC
The sensors shall be in direct physical contact with the item or installed sensor in each position being monitored and shall be placed, as far as possible, in or on the part that will be slowest to achieve the specified temperature.
Record the temperatures obtained throughout a process cycle. Perform the test in triplicate.
6.9.1.4 Results/acceptance criteria
Record the maximum deviation for each sensor from the specified temperature for each stage of the process and check for compliance with 5.4.1, 5.4.2 and 5.4.3.
6.9.2 Test for operating cycle temperature limits on washing and chemical disinfection stages
6.9.2.1 Principle
The test shall be applied only to those WD in which the washing and/or disinfection stage is not thermostatically regulated.
6.9.2.2 Material
Test equipment in accordance with 6.9.1.2.
6.9.2.3 Procedure
Locate the temperature sensors as specified in 6.9.1.3. Run a cycle. Supply the detergent and/or disinfectant solution at a temperature 2 °C to 4 °C below the minimum temperature specified for the washing/disinfection stage. Run a second cycle. Supply the detergent and/or disinfectant solution at a temperature 2 °C to 4 °C above the minimum temperature specified for the washing/disinfection stage.
6.9.2.4 Results/acceptance criteria
Record the minimum temperature attained by the load and chamber surface during the washing and/ or disinfection stage and whether or not a fault was indicated by the automatic controller.
Check for compliance with 5.4.4.
6.10 Chemical dosing tests for single-dose containers
6.10.1 Principle
For those WD in which the required dose of process chemical is contained in a single-dose container that is replaced before each cycle, means shall be provided to ensure that the intended volume has been dispensed.
6.10.2 Material
The test shall be performed with a single-dose chemical container that contains 90 % to 95 % of the
intended volume.
6.10.3 Procedure
Place a single-dose container into the WD and run a cycle using a container that contains 90 % to 95 %
of the intended volume.
Repeat the test three (3) times but replace the single-dose container before each cycle.
Copyright In2ter8national Organization for Standardization
Order Number: 02223302
© ISO 2018 – All rights reserved
Provided by IHS Markit under license with ANSI
No reproduction or networking permitted without license from IHS
Sold to:CANTEL MEDICAL *DA [001612] - SMARTIN@MEDIVATORS.COM, Not for Resale,2018-12-18 15:39:13 UTC
6.10.4 Results/acceptance criteria
Record whether a fault is indicated (see 5.7).
6.11 Tests of cleaning efficacy
6.11.1 General
Cleaning efficacy testing shall follow the requirements of ISO 15883-1:2006+Amd 1:2014, 6.10 with the exception of 6.10.2 (replaced by 6.11 in this document) but including 6.10.3.
6.11.2 Principle
To claim that particular device(s) can be processed in the WD, data shall be required to establish that the particular device(s) can be effectively cleaned in the WD.
The test procedure and test loads described below are designed to demonstrate compliance with the requirements of cleaning efficacy in accordance with ISO 15883-1:2006+Amd 1:2014, 6.10 but take into consideration the complex nature of the endoscope.
The measurement of cleaning efficacy shall be made on the cleaning stage alone. This shall include any stages that take place in the WD prior to admission of the disinfectant.
Cleaning efficacy tests shall be carried out on the surrogate devices that are representative for each relevant endoscope type test group (see 6.6.2) and on endoscopes of each relevant endoscope type test group as defined according to Annex H.
NOTE 1 These tests provide a basic assessment of the cleaning efficacy of the process.
NOTE 2 It might be inappropriate to include bacteria in some test soils while performing tests on installed,
operational WD.
NOTE 3 Where the WD manufacturer’s instructions for use with a particular endoscope requires a pre- treatment, e.g. manual cleaning of a particular component or channel, that pre-treatment can be included as part of the test procedure.
6.11.3 Material
6.11.3.1 Load carrier
The load carrier chosen for the test load shall be of the type recommended for the device to be processed.
The type test shall be done:
a) on at least one surrogate device specified according to Annex H and including at least block B2 [see Figure 2 b)]; the test pieces shall be the biofilm test pieces as specified in ISO/TS 15883-5:2005, Annex F incorporated into the surrogate device; the test pieces shall be placed at the same locations as the blockages indicated in Figure 2;
b) on surrogate devices of each relevant endoscope type test group as defined according to Annex H using test pieces contaminated with clinically relevant thermolabile (flexible) endoscope test soil(s) (see 6.11.3.3);
c) in addition, test loads composed of endoscopes from the relevant endoscope type test groups, according to Annex H, contaminated (internal and external surfaces) with the appropriate test soil (see 6.11.3.3), shall be used.
Copyright International Org©anizIaStioOn fo2r S0ta1n8dar–dizAatiloln rights reserved
Provided by IHS Markit under license with ANSI
No reproduction or networking permitted without license from IHS
Order Number: 02223302 29
Sold to:CANTEL MEDICAL *DA [001612] - SMARTIN@MEDIVATORS.COM, Not for Resale,2018-12-18 15:39:13 UTC
Under no circumstances shall the test pieces be installed in such a way that they unduly influence the correct flow of process fluids inside the channels.
NOTE 1 To minimize the possibility of damaging an endoscope it might be prudent to establish the efficacy of the process using a surrogate device before using an endoscope to verify the cleaning process.
For operational qualification testing, a surrogate device defined according to Annex H shall be used.
The appropriate surrogate device shall be specified.
NOTE 2 Alternatively, endoscopes can be selected according to Annex I.
Devices to constitute a test load shall be contaminated with one or more test soils that simulate the use of thermolabile (flexible) endoscopes. ISO/TS 15883-5 specifies examples of test soils. The rationale for the choice of test soil(s) shall be documented.
NOTE 1 ISO/TS 15883-5 is currently under revision as ISO 15883-5 to reflect current state-of-the-art. Local requirements can require the use of particular test soils and methods. Test soil formulations can be chosen based on a review of the literature and demonstration of its relevance based on the use of the devices in clinical practice. (Refer also to References [17], and [22] to [30] and [36]).
NOTE 2 The attention of manufacturers is drawn to the user's choice of test soil(s) and method(s) for operational testing. This can indicate a need to carry out similar testing before the WD is supplied.
The test soil(s) used for the load, chamber wall and load carriers may be the same or different. Where
different test soils are used the rationale for the choice of each test soil shall be documented.
The choice of test soil(s), its method of application, and conditioning (e.g. drying) shall simulate the worst-case clinical conditions of actual use of the devices. The method of test soil recovery (sampling/ extraction from devices) and detection of analytes shall be validated.
6.11.4 Procedure
Place the test load contaminated with the test soil in the chamber. Connect the endoscope ports to the channel irrigation devices in accordance with the WD manufacturer’s instructions and process. Tests using contaminated devices shall only be carried out after satisfactory completion of the tests using the surrogate device.
NOTE The use of endoscopes that are in clinical use for any testing that includes the application of test soils and/or test contamination can represent a risk in further use of the endoscope.
Start a normal operating cycle for the load type under test. Interrupt the cycle just prior to the start of the disinfection stage. Then examine the test load for the presence of residual soil.
6.11.5 Results/acceptance criteria
Record the adequacy of the cleaning stage using the criteria specified for the particular test soil used.
6.12 Tests of disinfection efficacy
6.12.1 General
The conditions of use of disinfectants within the WD shall be within the specified and validated
conditions (see 4.4.2.2).
--`,,,,````,``,,``,,,``,-`-``,```,,,`---
Copyright In3ter0national Organization for Standardization
Order Number: 02223302
© ISO 2018 – All rights reserved
Provided by IHS Markit under license with ANSI
No reproduction or networking permitted without license from IHS
Sold to:CANTEL MEDICAL *DA [001612] - SMARTIN@MEDIVATORS.COM, Not for Resale,2018-12-18 15:39:13 UTC
Tests conducted on disinfectants shall be carried out at the end of the specified shelf life, after the disinfectant has been stored under the specified worst-case storage conditions.
NOTE 1 Subject to national regulatory requirements, these conditions can be simulated by the use of validated accelerated ageing when necessary or, when a validated stability study is available, by diluting the disinfectant to the minimum concentration observed at the end of the specified shelf life.
Tests conducted on disinfectants produced or activated immediately prior to use shall be carried out at
the minimum concentration available in normal use.
NOTE 2 National regulatory authorities can have additional requirements for approval of disinfectants
used in WD.
6.12.2 Preliminary tests on chemical disinfectants
6.12.2.1 Principle
An initial series of tests, as set out in 6.12.2.2 to 6.12.2.3, intended to verify, in vitro, the microbicidal activity of the disinfectant solution under conditions identical to those that will be applied at the time of the cycle's disinfection stage shall be carried out unless adequate data under relevant conditions can be supplied for shorter contact time(s).
The disinfectant solution shall be verified as virucidal, bactericidal, fungicidal, mycobactericidal and active against bacterial endospores as specified in 4.4.2.2.
During these tests experimental conditions intended to simulate the conditions within the WD shall
be used.
6.12.2.2.1 Disinfectants
Each product provided in the list of usable disinfectants shall be tested.
6.12.2.2.2 Neutralizing agent
An appropriate neutralizing agent shall be employed for each disinfectant tested.
6.12.2.2.3 Test organisms
Test organisms shall be selected on the basis of the following criteria:
a) documented high resistance to the disinfectant under investigation;
b) species typically found on item to be processed;
c) species of clinical significance typically found on item to be processed;
d) representative species of the major groups of microorganisms.
As a minimum, the test organisms shall include Gram-positive and Gram-negative vegetative bacteria, Mycobacterium sp., enveloped and non-enveloped viruses, fungi, and bacterial endospores. The test organism strains shall be selected from B.2.1.1. A rationale is required for the use of strains other than those listed in B.2.1.1.
NOTE Guidance on choice of organisms can be obtained from relevant published standards on disinfectant efficacy testing e.g. EN 13624, EN 13727, EN 14347, EN 14348, EN 14476, AOAC International 2012, ASTM E1052- 11, ASTM E1053 - 11, DVV 2015.
--`,,,,````,``,,``,,,``,-`-``,```,,,`---
Copyright International Org©anizIaStioOn fo2r S0ta1n8dar–dizAatiloln rights reserved
Provided by IHS Markit under license with ANSI
No reproduction or networking permitted without license from IHS
Order Number: 02223302 31
Sold to:CANTEL MEDICAL *DA [001612] - SMARTIN@MEDIVATORS.COM, Not for Resale,2018-12-18 15:39:13 UTC
ISO 15883-4:2018(E)
6.12.2.3.1 Concentration
The product shall be tested at the MRC.
In the case where it is intended that a disinfectant solution be re-used, the efficacy of the solution shall be determined as a function of its MRC, and if required, at the MEC.
6.12.2.3.2 Temperature
Two cases shall be considered:
a) if the disinfection temperature stage is carried out under ambient conditions, the test temperature shall be the minimum temperature permitted during the cycle's disinfection stage;
b) if the disinfection stage is carried out under temperature controlled conditions, the test temperature shall correspond to the lower limit of the specified disinfection temperature.
6.12.2.3.3 Contact time
Two cases shall be considered:
a) if the disinfection stage is carried out under ambient conditions, the contact time observed during the tests shall be equal to the minimum duration of the disinfection stage;
b) if the disinfection stage is carried out under temperature controlled conditions, the contact time observed during the tests shall be equal to the minimum duration of the disinfection stage and the temperature of the disinfectant solution shall be constantly at the minimum temperature specified for the disinfection stage.
The above applies unless adequate data under relevant conditions can be supplied for shorter contact
time(s).
6.12.2.3.4 Water quality
If applicable, evidence shall be documented to demonstrate the efficacy of the disinfectant in the
presence of hard water (see 6.4.2).
Before commencing an investigation of the efficacy of the disinfectant a method of neutralizing the disinfectant at the end of the exposure period shall be demonstrated and documented. This shall include demonstration that, for any neutralizing agent used, neither the neutralizing agent nor its reaction product with the disinfectant, are microbicidal or microbiostatic. When a secondary host, such as a cell culture, is used as the detection system for the survival of test organisms, the absence of carry over effects on the cell culture system and detection of low numbers of test organisms added as a challenge to the test system shall be demonstrated.
6.12.2.3.6 Presentation of test organisms
While initial tests may be carried out using a suspension of test organisms, the demonstration of activity on contaminated surfaces shall be required.
NOTE Guidance on carrier tests can be obtained from relevant published standards on disinfectant efficacy testing e.g. EN 14885, EN 14561, EN 14562, ASTM E1053-11, ASTM E2197-11, AOAC International 2012.
Copyright In3ter2national Organization for Standardization
Order Number: 02223302
© ISO 2018 – All rights reserved
Provided by IHS Markit under license with ANSI
No reproduction or networking permitted without license from IHS
Sold to:CANTEL MEDICAL *DA [001612] - SMARTIN@MEDIVATORS.COM, Not for Resale,2018-12-18 15:39:13 UTC
6.12.2.3.7 Detection of test organisms
The culture method used to enumerate the number of surviving microorganisms after exposure to the disinfectant shall be validated. The culture method shall be capable of recovering a low number (approximately 10 CFU) of the organisms for which it is intended to be used.
6.12.2.4 Results/acceptance criteria
Verify that the microbicidal activity of the disinfectant solution is compliant with the requirements specified in 4.4.2.2.
6.12.3 Self-disinfection tests
6.12.3.1.1 Principle
The type test is intended to verify that the WD “self-disinfection” mode will disinfect those parts of the WD which come into contact with fluids that are intended to, or could, contact the load.
NOTE The WD can be equipped with an automatic or manually selected thermal or chemical “self- disinfection” mode (see 4.8.1). The preferred method is thermal disinfection.
6.12.3.1.2 Material
The materials as described in ISO/TS 15883-5:2005, Annex F shall be used.
6.12.3.1.3 Procedure
The test method described in ISO/TS 15883-5:2005, Annex F shall be used.
6.12.3.2 Operational and routine test
6.12.3.2.1 Principle
The test on the final rinse water shall be sufficient to verify the self-disinfection cycle. (See 6.3).
NOTE In order to detect any biofilm, it might be necessary to wait to take samples after the WD is left unused at least six hours after completion of the self-disinfection cycle.
6.12.3.2.2 Material
See E.2.
6.12.3.2.3 Procedure
After the water has circulated through the components to be disinfected, the sample shall be taken from the chamber using the method specified in the instructions for use [see 8 k) 6)].
The sample shall be tested in accordance with E.3.
6.12.3.2.4 Results/acceptance criteria
See 6.3.3.
Copyright International Org©anizIaStioOn fo2r S0ta1n8dar–dizAatiloln rights reserved
Provided by IHS Markit under license with ANSI
No reproduction or networking permitted without license from IHS
Order Number: 02223302 33
Sold to:CANTEL MEDICAL *DA [001612] - SMARTIN@MEDIVATORS.COM, Not for Resale,2018-12-18 15:39:13 UTC
6.12.4 Test of microbial quality of final rinse water treatment equipment
6.12.4.1.1 Principle
The efficacy of the treatment system shall be challenged by inoculation with a suitable test organism. Escherichia coli K12 is recommended to be added upstream of the treatment system providing it is first demonstrated that this bacterium can persist in the water being used and is not inactivated by the water itself.
6.12.4.1.2 Material
Escherichia coli K12 cultivated according to EN 12353 and EN 13727.
6.12.4.1.3 Procedure
Escherichia coli K12 is added upstream of the treatment system. The inoculum shall be sufficient to produce a population of 1 × 106 CFU per millilitre in the final rinse water if there was no effect from the treatment system.
A sample of the final rinse water (not less than 200 ml) shall be collected during an operating cycle. Analyse two 100 ml aliquots for the number of remaining organisms using a 0,2 µm filter.
6.12.4.1.4 Results
Record the number of colony forming units recovered from each of the two tests.
6.12.4.1.5 Acceptance criteria
There shall be less than 10 CFU and no Escherichia coli K12 recovered from each of two 100 ml
aliquots tested.
Various treatment methods are used to ensure that the water from water treatment equipment is of appropriate microbial quality before use.
The test shall verify the performance of the particular system by the specified method. This shall include, as necessary:
a) verification of filter performance by an integrity test (e.g. bubble point test);
b) verification of thermal disinfection by thermometric testing.
6.12.5 Disinfection of liquid transport systems following failure of water treatment equipment
6.12.5.1.1 Procedure
The test methods specified in D.3.6.1 and D.3.6.2 shall be used to evaluate the disinfection of the water
treatment equipment.
Copyright In3ter4national Organization for Standardization
Order Number: 02223302
© ISO 2018 – All rights reserved
Provided by IHS Markit under license with ANSI
No reproduction or networking permitted without license from IHS
Sold to:CANTEL MEDICAL *DA [001612] - SMARTIN@MEDIVATORS.COM, Not for Resale,2018-12-18 15:39:13 UTC
6.12.5.1.2 Results/acceptance criteria
The performance shall be deemed to be satisfactory if the microbial count is less than 10 CFU/100 ml
and absence of Pseudomonas aeruginosa in 100 ml.
6.12.5.2 Operational and routine test
The test on the final rinse water as specified in 6.3 and Annex E shall be sufficient to verify the self- disinfection cycle.
6.12.5.2.2 Material/procedure
The sample taken to verify the attainment of this requirement shall be taken from the final rinse water of the first normal operating cycle following the self-disinfection cycle. If the final rinse consists of multiple stages the sample shall be taken from the last stage [see 8 k)].
6.12.5.2.3 Results/acceptance criteria
Performance criteria shall comply with 4.8.5.
6.12.6 Chemical disinfection of the load
The test shall be carried out in accordance with Annex B.
The test method shall use a surrogate device that complies with Annex H for each relevant endoscope type test group to simulate the load. Inoculated carriers shall be incorporated as part of the surrogate device to monitor the efficacy of the disinfection stage.
Tests shall be performed with the strain of Mycobacterium sp. demonstrated to be the most resistant to the disinfectant.
NOTE For further information on microbial testing of chemical disinfection processes, see Annex F.
6.12.6.2 Operational qualification
Operational qualification shall establish that the levels of all controlling variables that affect the disinfection of the load are within the limits established during type testing.
6.12.6.3 Performance qualification and routine test
For performance qualification and routine tests the process shall be verified by sampling endoscopes that have been used on patients after processing. The post-disinfection microbial contamination shall be estimated by analysis of samples taken immediately after the post-disinfection rinsing stage but without the drying stage. Sufficient samples for each test shall be used to provide assurance of disinfection of the processed endoscopes.
When required by national regulation, a surrogate device shall be used to simulate the load items. Inoculated carriers shall be incorporated as part of the surrogate device to monitor the efficacy of the disinfection stage (see 6.12.6.1).
NOTE 1 Microorganisms incorporated into test soils can be used instead of, or as well as, the use of inoculated
carriers (see ISO/TS 15883-5).
NOTE 2 Guidance on a suitable sampling protocol can be seen in References [31] and [32].
Copyright International Org©anizIaStioOn fo2r S0ta1n8dar–dizAatiloln rights reserved
Provided by IHS Markit under license with ANSI
No reproduction or networking permitted without license from IHS
Order Number: 02223302 35
Sold to:CANTEL MEDICAL *DA [001612] - SMARTIN@MEDIVATORS.COM, Not for Resale,2018-12-18 15:39:13 UTC
NOTE 3 Endoscopes can be selected by the user according to Annex I.
NOTE 4 Local and national requirements can specify the interpretation of microbiological test results and when the samples for routine testing are taken after a defined time period, e.g. at least 12 h after the operating cycle.
7 Documentation and inspection
Documentation and inspection shall be in accordance with ISO 15883-1:2006+Amd 1:2014, Clause 7.
8 Information to be supplied by the manufacturer
In addition to the information specified in ISO 15883-1:2006+Amd 1:2014, Clause 8, the following
information shall be provided:
a) the devices for which evidence is provided that they can be processed satisfactorily and any precautions necessary for particular devices or operational conditions [e.g. see 4.1.4, 5.2.1.1 b), and 5.2.2.1];
b) for each device listed in 8 a), it shall be specified whether the verification of device channel irrigation by the automatic controller (see 5.2.2) and/or the leak test system (see 4.2) function;
c) for each device, a description of the number and type of connections required for channel irrigation;
d) the minimum and maximum flow and the maximum pressure of fluids which may be delivered to
each channel during processing in the WD (see 5.2.1.3);
e) the maximum permissible restriction of flow through each channel before the automatic controller
will indicate a fault (see 5.2.2.1);
f) the maximum temperature of any process fluid in contact with the device during processing in the
WD and which can cause degradation of the device;
g) the maximum temperature variation permissible during the automatic leak test, if fitted (see 4.2.3);
h) details of which parts of the WD are subjected to disinfection during the self-disinfection cycle (see
i) guidance on the frequency at which any water treatment equipment that is part of the WD should
be disinfected (see 4.9.2.1 and 4.9.2.4);
j) diagram of the circulation of fluids in the WD used to irrigate channels in the device(s) (see 5.2.1.2);
k) instructions for use including:
1) the recommendation to use thermal disinfection for heat stable endoscopic accessories for medical devices (see 4.1.9);
2) guidance on the need for drying devices which are to be stored before use (see 4.7.1);
3) means to verify the flow of process fluids through each channel (see 5.2.1.1);
4) the method and frequency of self-disinfection (see 4.8);
5) the method and frequency for disinfection of the connection between the WD and the water supply for final rinse water (see 4.9.2.4);
6) the method to be used for collecting samples of final rinse water from the chamber (see
7) for WD not provided with an automatic leak test, the information that a manual leak test is required prior to processing [see 4.2.2 b)];
Copyright In3ter6national Organization for Standardization
Order Number: 02223302
© ISO 2018 – All rights reserved
Provided by IHS Markit under license with ANSI
No reproduction or networking permitted without license from IHS
Sold to:CANTEL MEDICAL *DA [001612] - SMARTIN@MEDIVATORS.COM, Not for Resale,2018-12-18 15:39:13 UTC
8) any pre-treatment recommended to ensure effective and safe processing of the endoscope and
its accessories;
l) locations of temperature sensors being representative of the lowest temperatures on the systems
(see 5.4);
m) maintenance instructions, including the planned preventive maintenance required on the piping used to convey final rinse water to the endoscope and the frequency at which such piping should be replaced (see 4.9.3); replacement of air and water filters at specified intervals or when integrity test indicates reduced performance;
n) the detergent(s) and disinfectant(s) type tested with the WD (see 4.3.3 and 4.4.5);
o) recommendation that the user monitors the disinfectant concentration using the method provided by the disinfectant manufacturer, e.g. an indicator test strip, specific for the disinfectant to show that the disinfectant is at or above the MRC (see also 4.4.4 and 4.4.5.2);
p) if the water treatment equipment is not part of the WD, the requirements for water supplied to the WD including the requirement to control the microbial contamination of the water supply (see 4.9.2.2);
q) quality of the rinse water used for post-washing rinsing (see 4.3.4);
r) details on how, or to which endoscope port on the WD, the endoscope channels are to be connected
(see 5.2.1.2);
s) if the water treatment is part of the WD and the parameters affecting the water treatment are not monitored by the automatic controller, then all parameters shall be specified to be verified by the user (see 4.9.2.5).
9 Marking, labelling and packaging
Marking, labelling and packaging shall be in accordance with ISO 15883-1:2006+Amd 1:2014, Clause 9.
10 Information to be requested from the purchaser by the manufacturer
The requirements of ISO 15883-1:2006+Amd 1:2014, Clause 10 apply.
In addition, the following information shall be requested from the purchaser:
a) the means that shall be provided to ensure that connection is made to the correct container of process chemical see (4.1.8);
b) list of all types of endoscopes and devices that the user intends to process in the WD.
Copyright International Org©anizIaStioOn fo2r S0ta1n8dar–dizAatiloln rights reserved
Provided by IHS Markit under license with ANSI
No reproduction or networking permitted without license from IHS
Order Number: 02223302 37
Sold to:CANTEL MEDICAL *DA [001612] - SMARTIN@MEDIVATORS.COM, Not for Resale,2018-12-18 15:39:13 UTC
Annex A
(informative)
Summary of activities covered by this document
A.1 General
This document covers a range of activities. The responsibilities for discharging these activities are not addressed within this document. This annex is intended to give guidance on an appropriate division of responsibility for these activities.
The key personnel are:
— the WD manufacturer;
— the endoscope manufacturer;
— the process chemical manufacturer (detergents, disinfectants);
— the purchaser/user.
A.2 Before installation of the WD
The overall responsibility for the design and construction of the WD is necessarily with the WD manufacturer. It is expected that the WD manufacturer will:
— state with which endoscopes the WD can be used; this is to be done in the light of information
provided by the endoscope manufacturer;
— provide test data demonstrating the performance of the WD with respect to both cleaning and disinfection using process chemicals specified by the WD manufacturer; this is to be done in the light of information provided by the process chemical manufacturer;
— seek information from the user on the quality of water available on the site where the WD is to be
installed;
— carry out type testing on each model of WD to establish compliance with the requirements of this
document;
— carry out works testing to establish that each WD released to the market is functioning to the standard established by type testing;
— provide information to the user to support the correct use of the WD (including, where necessary, reference to the endoscope manufacturer's instructions for processing).
A.3 Installation and operation of the WD
It is the responsibility of the purchaser/user facility to ensure that the WD is installed and operated correctly. These activities can be delegated.
Once the WD is installed on site, the overall responsibility for ensuring that the WD is correctly installed and functions correctly usually falls to the purchaser/user. This includes:
— installation qualification;
Copyright In3ter8national Organization for Standardization
Order Number: 02223302
© ISO 2018 – All rights reserved
Provided by IHS Markit under license with ANSI
No reproduction or networking permitted without license from IHS
Sold to:CANTEL MEDICAL *DA [001612] - SMARTIN@MEDIVATORS.COM, Not for Resale,2018-12-18 15:39:13 UTC
ISO 15883-4:2018(E)
— operational qualification;
— performance qualification;
— requalification;
— routine tests;
— use of the recommended process chemicals;
— operation of the WD in accordance with the WD manufacturer’s instructions (including limiting the
devices reprocessed through the WD to those which the WD manufacturer has specified).
Copyright International Org©anizIaStioOn fo2r S0ta1n8dar–dizAatiloln rights reserved
Provided by IHS Markit under license with ANSI
No reproduction or networking permitted without license from IHS
Order Number: 02223302 39
Sold to:CANTEL MEDICAL *DA [001612] - SMARTIN@MEDIVATORS.COM, Not for Resale,2018-12-18 15:39:13 UTC
Annex B
(normative)
Microbiological testing of the efficacy of chemical disinfection of the load
B.1 Principle
Artificially inoculated test pieces inserted within appropriate surrogate devices (see Annex H) are used
to test the physical removal of endospores and efficacy of the chemical disinfection process in the WD.
B.2 Material
B.2.1 Test organisms
B.2.1.1 A range of organisms representing the major groups and showing high resistance to the
disinfectant shall be used (see 6.12.2.3.6).
NOTE The organisms listed below are suggested as suitable. These are, for example, the organisms specified in EN 13624, EN 13727, EN 14347, EN 14348, EN 14476, EN 14561, EN 14562, EN 14563, ASTM E2197, and OECD
Guidelines. Additional organisms, or alternate organisms, that demonstrate high resistance to the disinfectant under the intended conditions of use (temperature, concentration etc.), or that are relevant for a particular application, can be used.
Preferred species are:
Pseudomonas aeruginosa (ATCC1) 15442) Serratia marcescens (ATCC 13880) Staphylococcus aureus (ATCC 6538) Enterococcus faecium (ATCC 12952) Enterococcus hirae (ATCC 10541) Mycobacterium terrae (ATCC 15755)
Mycobacterium avium (ATCC 15769)
Candida albicans (ATCC 10231)
Aspergillus (spores) brasiliensis (ATCC 10864) Adenovirus type 5 Adenoid 75 (ATCC VR-5) Poliovirus Type 1 LSc-2ab, or suitable surrogate
Bovine parvovirus strain Haden (ATCC VR-767) or Murine parvovirus strain Crawford (ATCC VR-1346)
1) ATCC refers to American Type Culture Collection, 10801 University Boulevard, Manassas, VA 20110-2209, USA, www.atcc.org. The ATCC numbers are the collection numbers of strains supplied by this reference culture collection. This information is given for the convenience of users of this document and does not constitute an endorsement by ISO of the product named.
Copyright In4ter0national Organization for Standardization
Order Number: 02223302
© ISO 2018 – All rights reserved
Provided by IHS Markit under license with ANSI
No reproduction or networking permitted without license from IHS
Sold to:CANTEL MEDICAL *DA [001612] - SMARTIN@MEDIVATORS.COM, Not for Resale,2018-12-18 15:39:13 UTC
ISO 15883-4:2018(E)
Murine norovirus strain (S99)2), or suitable surrogate endospores of Clostridium difficile (NCTC3) 13366) endospores of Geobacillus stearothermophilus (ATCC 7953) endospores of Bacillus subtilis/atropheus (ATCC 6633)
An identical strain obtained from an alternative reference culture collection may be substituted for the ATCC strains specified.
B.2.1.2 Defined strains from a type culture collection shall be used.
B.2.1.3 Microbiological testing of the efficacy of chemical disinfection of the load shall be carried out either with a range of organisms (see examples given in B.2.1.1) identified as most resistant to the particular disinfectant in preliminary tests (see 6.12.2.3.6), or other organisms that have been determined to have particular resistance to the disinfection process.
NOTE 1 The test methods described below are not applicable to tests with viral strains. Guidance on appropriate test methods for viral strains can be found in e.g. EN 14476, ASTM E2197, and OECD Guidelines.
NOTE 2 Elimination of bacterial endospores is not expected from a disinfection process; however some sporicidal activity is expected (see 4.4.2.2). The low level of activity against endospores compared with vegetative cells makes the endospores a useful indicator of the extent of removal compared with kill. The use of a thermophilic endospore facilitates recovery without interference from mesophilic microorganisms, which are also present.
B.2.2 Test pieces
A surrogate device shall be used (see 6.6 and Annex H).
Test pieces for inoculation shall be formed from polytetrafluoroethylene (PTFE) tubing, 150 mm in length and of the same diameter as the channels they are placed in within the surrogate device (see 6.6.3).
B.2.3 Suspension media
Bacterial endospores shall be suspended in sterile distilled water.
It shall be confirmed by appropriate heat treatment or other methods that endospore suspensions contain sufficient endospores and only low numbers of vegetative cells of the same organism, i.e. the growth method used yields a high percentage of endospores; usually more than 95 %.
The other test organisms shall be suspended in a suitable sterile isotonic solution, e.g. for bacteria, peptone water with 10 % sodium glutamate.
B.2.4 Inoculum
The inoculum shall contain known high numbers of the test organism, e.g. for bacteria the inoculum shall contain not less than 108 CFU/ml. The population in the original inoculum and deposited on the test piece for exposure to the disinfection process shall be counted using a validated method.
2) Federal Research Institute of Animal Health, Department of Experimental Animal Facilities and Biorisk Management (ATB), Bio Bank, Virus Collection, Südufer10, D-17493 Greifswald, https://www.fli.de/de/institute/abteilung-fuer-experimentelle-tierhaltung-und-biosicherheit-atb/bio-bank/
3) NCTC refers to National Collection of Type Cultures, operated by Public Health, England, Porton Down,Salisbury, SP4 0JG UK. The NCTC number is the collection number of the strain supplied by this reference culture collection. This information is given for the convenience of users of this document and does not constitute an endorsement by ISO of the product.
--`,,,,````,``,,``,,,``,-`-``,```,,,`---
Copyright International Org©anizIaStioOn fo2r S0ta1n8dar–dizAatiloln rights reserved
Provided by IHS Markit under license with ANSI
No reproduction or networking permitted without license from IHS
Order Number: 02223302 41
Sold to:CANTEL MEDICAL *DA [001612] - SMARTIN@MEDIVATORS.COM, Not for Resale,2018-12-18 15:39:13 UTC
ISO 15883-4:2018(E)
B.2.5 Microsyringe
Use a microsyringe to dispense 25 µl aliquots into each of the 150 mm long test pieces. Allow the test pieces to dry (e.g. by rotation) and repeat the procedure three more times, for a total of four applications.
Processed test pieces shall be immersed in a sterile isotonic solution containing a suitable neutralizer for the disinfectant.
B.2.7 Recovery medium
After neutralization, lengthwise slit test pieces (see B.3.2) shall be immersed in 20 ml sterile 25 % Ringers solution containing 0,05 % polysorbate 80 in thin walled glass screw capped container (e.g. 25 ml universal bottle).
B.3 Procedure
B.3.1 General
Details of the methods of preparation of cultures shall be reported with the results. Standard published methods shall be used wherever possible.
Transfer the processed test piece to a sterile isotonic solution containing a suitable neutralizer for the disinfectant (see B.2.6).
Remove the processed test piece after the validated exposure time to the neutralizer.
Cut the 150 mm length of processed test piece in half and then cut one of the halves in half again and then slit lengthwise with a sterile scalpel. Transfer the split halves to 20 ml of sterile 25 % (quarter strength) Ringers solution containing 0,05 % polysorbate 80 in a thin walled glass screw capped container (e.g. 25 ml universal bottle).
Use a validated recovery method (see ISO 11737-1).
Use the eluate to prepare a dilution series from which a viable count shall be determined.
It is important in this dilution series to analyse the entire half-sample from each dilution to ensure that counts are adequately determined.
NOTE This can be done using membrane filtration rather than by using spread or pour plating.
Transfer the other half of the test piece to recovery medium (growth/no growth test).
Samples on which the inoculum is dried, but no disinfection treatment is performed, shall serve as
controls to demonstrate appropriate inactivation of microbial numbers.
B.3.3 Evaluation of initial inoculum
Test the test pieces prepared as described above by the recovery method to determine the population
of each test organism which can be recovered from the inoculum.
B.3.4 Evaluation of physical removal using endospores as an indicator organism
If the disinfectant is sporicidal, then it will be necessary to evaluate the physical removal of test organisms by repeating the study with Geobacillus stearothermophilus endospores with the disinfectant solution replaced by water.
Copyright In4ter2national Organization for Standardization
Order Number: 02223302
© ISO 2018 – All rights reserved
Provided by IHS Markit under license with ANSI
No reproduction or networking permitted without license from IHS
Sold to:CANTEL MEDICAL *DA [001612] - SMARTIN@MEDIVATORS.COM, Not for Resale,2018-12-18 15:39:13 UTC
ISO 15883-4:2018(E)
Expose the surrogate devices incorporating test pieces inoculated with Geobacillus stearothermophilus endospores to the disinfection stage, run with water instead of disinfectant solution, and recover by the method described. The difference in population between the two test pieces and the original inoculum is a measure of the extent to which test organisms are physically removed by the WD disinfection stage.
NOTE Thermophilic endospores are used during type testing in order to ensure that any endospores remaining in the WD do not interfere with subsequent tests employing mesophilic organisms.
There shall be not less than 105 endospores remaining on each of the test pieces exposed to the
simulated WD disinfection stage.
For some WD it can be necessary to reduce the rate and/or volume of flow through the surrogate device during this test in order to ensure that at least 105 endospores remain. When this is done it should be clearly indicated on the type test report.
B.3.5 Evaluation of disinfection efficacy
Expose the surrogate devices incorporating test pieces inoculated with test organism to the WD disinfection stage and recover by the method described. Carry out all tests in duplicate.
B.4 Results
Concerning the evaluation of physical removal using endospores as an indicator organism, there shall be not less than 105 endospores remaining on each of the test pieces exposed to the simulated WD disinfection stage.
Record the log10 reduction obtained for each test organism used.
Copyright International Org©anizIaStioOn fo2r S0ta1n8dar–dizAatiloln rights reserved
Provided by IHS Markit under license with ANSI
No reproduction or networking permitted without license from IHS
Order Number: 02223302 43
Sold to:CANTEL MEDICAL *DA [001612] - SMARTIN@MEDIVATORS.COM, Not for Resale,2018-12-18 15:39:13 UTC
Annex C
(normative)
Summary of test programmes
C.1 General
It is unrealistic and not practicable to perform type tests on all model/type of endoscopes.
Although surrogate devices, as defined in Annex H, are very close to real endoscopes, some aspects can remain different (e.g. trumpet valves, connectors), and not all internal design aspects of real endoscopes might be covered by surrogate devices. This means that not all aspects of cleaning and disinfection can be verified using surrogate devices only. Consequently, some tests need to be performed on real endoscopes.
It is necessary to:
1) verify the ability of the disinfectant to kill microorganisms according to in vitro tests (see Table C.1,
Type test, A - in vitro tests);
2) confirm using surrogate devices representing the relevant type test groups, as defined in Annex H that these flow conditions can be reached on all endoscope channels and for all endoscopes intended to be tested (see Table C.1, Type test, B – Surrogate devices);
3) confirm using real endoscopes that such flow conditions yield cleaned and disinfected endoscopes
(see Table C.1, Type test, C – Endoscopes, and Performance Qualification, Routine test, D - Endoscopes).
Copyright In4ter4national Organization for Standardization
Order Number: 02223302
© ISO 2018 – All rights reserved
Provided by IHS Markit under license with ANSI
No reproduction or networking permitted without license from IHS
Sold to:CANTEL MEDICAL *DA [001612] - SMARTIN@MEDIVATORS.COM, Not for Resale,2018-12-18 15:39:13 UTC
ISO 15883-4:2018(E)
Table C.1 — Summary of device to be used at each stage for specified tests
|
Stage |
Type test |
Performance qualification, routine test | ||
|
A in vitro tests |
B Surrogate devices (Annex H) |
C Endoscopes |
D Surrogate devices/ endoscopes | |
|
Channel non-obstruction |
Not required |
See 6.6b |
Not required |
See 6.6.3 |
|
Cleaning |
Not required |
Test on biofilm, (see 6.11.3.2 a)e, Test on other test soils, (see 6.11.3.2 b)g |
See 6.11.3.2 c)i |
See 6.11ad |
|
Disinfection |
See 6.12.2 |
Not required |
Not required | |
|
Complete process |
Not required |
See 4.1.3f |
See 4.1.3c |
See 6.12.6.3a |
|
a Annex H provides a useful tool to perform a risk analysis and verify if the WD processing fluids circulate through endoscope channels. Nevertheless, it is necessary to verify that the WD, as installed and operated in accordance with operational procedures, consistently performs in accordance with predetermined criteria and thereby yields product meeting its specification. Performance tests shall be performed with one model of each endoscope product family for which the same connector set is used. b Especially in case of complex designs, surrogate devices only shall be used. c Type tests shall be performed on a representative endoscope from each relevant endoscope type test group (see Annex H) to demonstrate compliance with 4.1.3. d This test may be done at the end of the complete cycle using one of the methods described in ISO 15883-1:2006+Amd 1:2014, Annex C, or any equivalent method. Some disinfectants react with proteins. Where reaction products are not detected by all methods described in ISO 15883-1:2006+Amd 1:2014, Annex C, an alternative method can be required. e This test shall be done on at least one surrogate device selected according to Annex H and including at least block B2 [see Figure 2 b)]. The test pieces may be placed at the same locations as the blockages indicated in Figure 2. f This test shall be done on at least one surrogate device selected according to Annex H and including at least blocks A2 and B2 (see Figure 2), modified to be in line with the 2 mm internal diameter used in ISO/TS 15883-5:2005, Annex I. The test pieces may be placed at the same locations as the blockages indicated in Figure 2. g This test shall be done on the surrogate devices of each relevant type test group as selected according to Annex H. h This test shall be done on at least one surrogate device selected according to Annex H and including at least blocks A2 and B2 (see Figure 2). i Endoscopes are used to cover aspects like outer surface, elevator section, etc. This test shall be done by using one representative of each relevant type test group as selected in Annex H. | ||||
Copyright International Org©anizIaStioOn fo2r S0ta1n8dar–dizAatiloln rights reserved
Provided by IHS Markit under license with ANSI
No reproduction or networking permitted without license from IHS
![]()
Order Number: 02223302 45
Sold to:CANTEL MEDICAL *DA [001612] - SMARTIN@MEDIVATORS.COM, Not for Resale,2018-12-18 15:39:13 UTC
ISO 15883-4:2018(E)
Table C.2 — Summary of tests in addition to ISO 15883-1:2006+Amd 1:2014
|
Brief description of test |
Requirement subclause |
Test subclause |
Type test |
Works test |
Operational qualification |
Performance qualification |
Routinea test |
|
1. Leak test failure alarm |
X |
X |
X |
B |
X (Q) | ||
|
2. Leak test non-connection test |
X |
X |
B |
X |
X(Q) | ||
|
3. Leak test over-pressurization prevention test |
4.2.4 d) |
X |
X |
B |
B |
B | |
|
4. Cleaning efficacy |
X |
B |
X |
X |
X (Q) | ||
|
5. in vitro disinfectant efficacy |
X |
B |
B |
B |
B | ||
|
6. Disinfection efficacy — Type test |
X |
B |
B |
B |
B | ||
|
7. Complete process — Operational and performance qualification |
O O |
B B |
X B |
O X |
X X (Q) | ||
|
8. Drying |
X |
O |
X |
B |
X | ||
|
9. Disinfection of liquid transport system — Type test |
X |
B |
B |
B |
B | ||
|
10. Disinfection of liquid transport system — Operational qualification and routine test |
O |
B |
X |
B |
X | ||
|
11. Self-disinfection test — Type test |
X |
B |
B |
B |
B | ||
|
12. Self-disinfection test — Operational qualification and routine test |
O |
B |
X |
B |
X | ||
|
13. Disinfection of water treatment equipment |
X |
B |
O |
B |
B | ||
|
14. Final rinse water treatment — Microbial quality |
O |
B |
X |
B |
B | ||
|
15. Channels non-obstruction test |
X |
X |
B |
X |
X(Q) | ||
|
16. Channels non- connection test |
X |
X |
B |
X |
X (Q) | ||
|
X – Recommended B – Not recommended O – Optional Q – Quarterly W – Weekly a Frequency of routine testing may be established based on risk assessment using trend analysis. | |||||||
Copyright In4ter6national Organization for Standardization
Order Number: 02223302
--`,,,,````,``,,``,,,``,-`-``,```,,,`---
© ISO 2018 – All rights reserved
Provided by IHS Markit under license with ANSI
No reproduction or networking permitted without license from IHS
Sold to:CANTEL MEDICAL *DA [001612] - SMARTIN@MEDIVATORS.COM, Not for Resale,2018-12-18 15:39:13 UTC
ISO 15883-4:2018(E)
Table C.2 (continued)
|
Brief description of test |
Requirement subclause |
Test subclause |
Type test |
Works test |
Operational qualification |
Performance qualification |
Routinea test |
|
17. Temperature throughout process |
X |
X |
X |
X |
X (Q) | ||
|
|
|
|
|
|
|
| |
|
18. Minimum process temperature test |
X |
X |
X |
X |
X (Q) | ||
|
19. Water quality |
4.9.2.3 a) 4.9.2.3 b) |
B |
B |
X |
X |
X (W) X (Q) | |
|
20. Chemical dos- ing test (single-dose container) |
X |
X |
X |
B |
O | ||
|
X – Recommended B – Not recommended O – Optional Q – Quarterly W – Weekly a Frequency of routine testing may be established based on risk assessment using trend analysis. | |||||||
Copyright International Org©anizIaStioOn fo2r S0ta1n8dar–dizAatiloln rights reserved
Provided by IHS Markit under license with ANSI
No reproduction or networking permitted without license from IHS
![]()
Order Number: 02223302 47
Sold to:CANTEL MEDICAL *DA [001612] - SMARTIN@MEDIVATORS.COM, Not for Resale,2018-12-18 15:39:13 UTC
Annex D
(normative)
Methods for microbiological evaluation of disinfection of liquid transport system
D.1 Principle
The following two methods are intended to simulate various incidents that might arise during normal
use of the WD, and that could give rise to contamination of the WD (see 4.9.2 and 6.12.5).
Method 1 (specified in D.3.6.1) tests the self-disinfection cycle after a simulated malfunction of the internal water treatment equipment that, although repaired quickly (24 h later), has caused contamination of the WD by the microorganisms present in the supply water.
Method 2 (specified in D.3.6.2) also simulates the case of WD contamination by microorganisms present in the supply water following a malfunction of the internal water treatment equipment. However, in this case, the self-disinfection cycle is only applied one week after a water equipment malfunction, and that during this week the WD has continued to be used (one endoscope washing/disinfection cycle per day). This allows evaluation of the efficiency of the self-disinfection cycle of a potentially contaminated WD after one week of use. Moreover, monitoring the internal level of contamination of the WD during the interval of time between the water treatment equipment failure and the execution of the self- disinfection cycle will allow evaluation of whether the WD's design is effective in limiting the growth of microorganisms and potential development of biofilm in the pipes of the WD.
D.2 Material
D.2.1 Microorganisms
Pseudomonas aeruginosa CIP4) A22 or ATCC5) 25619 (or equivalent) as microorganism. Bacterial suspension, with 1 × 109 CFU/ml to 1 × 1010 CFU/ml in sterile distilled water.
D.2.2 Culture medium
Soybean casein digest (SCD) agar or Tryptone soya agar (TSA) (see EN 12353 and EN 13727), as
maintenance and counting medium.
D.2.3 Washer-disinfector
The following cycles shall be available:
— endoscope WD cycle;
— self-disinfection cycle;
4) CIP refers to Collection of Institut Pasteur. The CIP numbers are the collection numbers of strains supplied by this reference culture collection. This information is given for the convenience of users of this document and does not constitute an endorsement by ISO of the product named.
5) ATCC refers to American Type Culture Collection, 10801 University Boulevard, Manassas, VA 20110-2209, USA, www.atcc.org. The ATCC numbers are the collection numbers of strains supplied by this reference culture collection. This information is given for the convenience of users of this document and does not constitute an endorsement by ISO of the product named.
Copyright In4ter8national Organization for Standardization
Order Number: 02223302
© ISO 2018 – All rights reserved
Provided by IHS Markit under license with ANSI
No reproduction or networking permitted without license from IHS
Sold to:CANTEL MEDICAL *DA [001612] - SMARTIN@MEDIVATORS.COM, Not for Resale,2018-12-18 15:39:13 UTC
ISO 15883-4:2018(E)
— sampling cycle;
— contamination cycle.
D.2.3.1 Sampling cycle
The sampling cycle shall correspond to a routine endoscope cleaning and disinfection cycle interrupted during the stage before disinfection, and for which the detergent shall be replaced by sterile distilled water. Once the cycle has been interrupted, a sample from the bottom of the tank containing water having circulated in the WD pipe work shall be taken.
NOTE This sampling programme only includes the cleaning and rinsing stage and circulates water throughout the WD's pipe work, without there being any addition of disinfectant or detergent product.
If the cycle cannot be interrupted immediately prior to the disinfection stage then a complete cycle substituting sterile purified (e.g. reverse osmosis) water for all process chemical solutions shall be used.
D.2.3.2 Contamination cycle
This special programme corresponds to a routine cleaning and disinfection cycle for which:
— the disinfectant solution heating system (if fitted) is deactivated;
— the detergent and disinfectant are replaced by sterile distilled water. During this contamination cycle, the WD is connected to the external tank containing the contamination
solution (see Figure D.1), so that during each phase of the contamination cycle, the WD is only fed with the contamination solution contained in the external tank.
D.2.4 Connection of the WD to the external tank
The connection of the WD to the external tank shall be as shown in Figure D.1.
Key
1 WD
2 water supply
3 drainage
4 external tank
NOTE As a function of manufacturer's recommendations, external peripherals can be inserted between the water supply network and the WD (water softener, etc.).
Figure D.1 — Connection of the WD to the external tank — Test configuration
Copyright International Org©anizIaStioOn fo2r S0ta1n8dar–dizAatiloln rights reserved
Provided by IHS Markit under license with ANSI
No reproduction or networking permitted without license from IHS
Order Number: 02223302 49
Sold to:CANTEL MEDICAL *DA [001612] - SMARTIN@MEDIVATORS.COM, Not for Resale,2018-12-18 15:39:13 UTC
ISO 15883-4:2018(E)
D.3 Procedure
D.3.1 External tank disinfection
Before each test, subject the external tank in which the contamination solution is prepared to a thermal disinfection cycle with an A0 of not less than 600.
D.3.2 Verification of absence of microbicidal residue in the external tank after disinfection
During the last rinsing stage of the external tank, collect 9 ml of the water circulating in the external tank and associated pipework.
Incorporate 1 ml of a bacterial suspension of Pseudomonas aeruginosa at 103 CFU/ml in the previously
sampled 9 ml of water.
After mixing thoroughly and 10 min of contact time, determine the number of viable bacteria present in the reaction mixture, CN, by serial dilution and counting on an SCD or TSA plate. After applying Formula (D.1), the rinsing is only considered to be valid if
CC
³ 0,8
(D.1)
where
CN is the number of viable bacteria present in the reaction mixture;
Cc is the exact concentration of bacteria in the bacterial suspension (control).
D.3.3 Preparation of the contamination solution
Fill the external tank with 30 l of tap water and 30 ml of a Pseudomonas aeruginosa suspension containing 109 CFU/ml. After thorough mixing, take a sample in order to determine, by serial dilution and counting on a SCD agar plate or TSA plate, the exact concentration of microorganisms in the contamination solution.
D.3.4 Contamination of the WD via the water supply network
After having prepared the contamination solution and deactivated the WD water treatment unit, connect the WD subjected to the tests to the external tank (Figure D.1). Then start the WD contamination cycle in order to ensure circulation of the contamination solution in all the internal piping of the WD.
D.3.5 Determination of the WD contamination level
During the different tests, determine the contamination level of the WD by running a sampling cycle and then establishing the concentration of microorganisms in the water having circulated in all the piping of the WD during this cycle. For this, during the sampling cycle collect 2 l of the water in the chamber of the WD. Filter 10 ml, 100 ml and 1 000 ml of the 2 l of water through 0,2 µm membranes. Then rinse the membranes with 3 × 50 ml of sterile distilled water, place on counting medium and incubate at 37 °C for 24 h.
After incubation, count and identify the number of colony forming units, and express the results as a number of colony forming units per litre.
Copyright In5ter0national Organization for Standardization
Order Number: 02223302
© ISO 2018 – All rights reserved
Provided by IHS Markit under license with ANSI
No reproduction or networking permitted without license from IHS
Sold to:CANTEL MEDICAL *DA [001612] - SMARTIN@MEDIVATORS.COM, Not for Resale,2018-12-18 15:39:13 UTC
ISO 15883-4:2018(E)
D.3.6 Establishment of the efficacy of the disinfection of the liquid transport system
Proceed as follows:
1) install the WD;
2) run a self-disinfection cycle;
3) run a sampling cycle;
4) determine the WD contamination level;
5) deactivate the water treatment system (i.e. remove filter, deactivate heating system);
6) disinfect the external tank;
7) prepare the contamination solution;
8) contaminate the WD via the water supply network;
9) leave the WD at room temperature (not less than 20 °C) to incubate for 24 h;
10) connect the WD normally;
11) re-activate the water treatment system;
12) run a self-disinfection cycle;
13) run a sampling cycle;
14) determine the contamination level of the WD in accordance with D.3.5;
15) if the analysis of the results shows a total viable count of 10 CFU/100 ml or more or presence of
Pseudomonas aeruginosa in the sample taken during step 14), repeat steps 12), 13) and 14).
NOTE It is not necessary to determine the contamination level before the disinfection cycle (see step 12) since the extent of contamination that can occur is specific to the design of the WD liquid transport system.
Proceed as follows:
1) install the WD;
2) run a self-disinfection cycle;
3) run a sampling cycle;
4) determine the WD contamination level;
5) deactivate the water treatment system (i.e. remove filter, deactivate heating system);
6) disinfect the external tank;
7) prepare the contamination solution;
8) contaminate the WD via the water supply network;
9) leave the WD at room temperature (not less than 20 °C) to incubate for 48 h;
10) connect the WD normally;
--`,,,,````,``,,``,,,``,-`-``,```,,,`---
Copyright International Org©anizIaStioOn fo2r S0ta1n8dar–dizAatiloln rights reserved
Provided by IHS Markit under license with ANSI
No reproduction or networking permitted without license from IHS
Order Number: 02223302 51
Sold to:CANTEL MEDICAL *DA [001612] - SMARTIN@MEDIVATORS.COM, Not for Resale,2018-12-18 15:39:13 UTC
ISO 15883-4:2018(E)
11) re-activate the water treatment system;
12) run a standard endoscope cleaning and disinfection cycle;
13) run a sampling cycle;
14) determine the contamination level of the WD in accordance with D.3.5;
15) leave the WD at room temperature (not less than 20 °C) to incubate for 24 h;
16) run a standard endoscope cleaning and disinfection cycle;
17) run a sampling cycle;
18) determine the contamination level of the WD in accordance with D.3.5;
19) leave the WD at room temperature (not less than 20 °C) to incubate for 24 h;
20) run a standard endoscope cleaning and disinfection cycle;
21) run a sampling cycle;
22) determine the contamination level of the WD in accordance with D.3.5;
23) leave the WD at room temperature (not less than 20 °C) to incubate for 24 h;
24) run a standard endoscope cleaning and disinfection cycle;
25) run a sampling cycle;
26) determine the contamination level of the WD in accordance with D.3.5;
27) leave the WD at room temperature (not less than 20 °C) to incubate for 24 h;
28) run a standard endoscope cleaning and disinfection cycle;
29) run a sampling cycle;
30) determine the contamination level of WD in accordance with D.3.5;
31) leave the WD at room temperature (not less than 20 °C) to incubate for 48 h;
32) run a self-disinfection cycle;
33) run a sampling cycle;
34) determine the contamination level of the WD in accordance with D.3.5;
35) if the analysis of the results shows a total viable count of 10 CFU/100 ml or more or presence of
Pseudomonas aeruginosa in the sample taken during step 33), repeat steps 32), 33) and 34).
D.4 Results/acceptance criteria
For both methods (Method 1 and Method 2), record the number of self-disinfection cycles needed to
reduce the contamination to less than 10 CFU/100 ml with absence of Pseudomonas aeruginosa.
Copyright In5ter2national Organization for Standardization
Order Number: 02223302
© ISO 2018 – All rights reserved
Provided by IHS Markit under license with ANSI
No reproduction or networking permitted without license from IHS
Sold to:CANTEL MEDICAL *DA [001612] - SMARTIN@MEDIVATORS.COM, Not for Resale,2018-12-18 15:39:13 UTC
Annex E
(normative)
Tests for microbial contamination of final rinse water
E.1 Principle
Samples of WD rinse water are inoculated onto appropriate microbiological growth media to evaluate the microbial quality of the water. The media facilitates the growth and counting of aerobic mesophilic bacteria, including Pseudomonas aeruginosa, and detection of environmental (atypical) Mycobacterium sp.
Sampling containers used for collection of final rinse water shall be 250 ml, or larger, and shall be
sterile.
E.3.1 Sampling technique
Take samples from draw-off points adjacent to the WD and from the point of discharge into the WD
chamber or load.
Swab the discharge surfaces of the sampling points thoroughly with 0,2 µm filtered 70 % alcohol and allow to dry by evaporation immediately before the sample is taken.
Collect a sample of not less than 200 ml, or as specified, from each sampling point for each test to be
carried out.
Test the samples within 4 h of collection or store at 2 °C to 5 °C and test within 48 h of collection.
E.3.2 Test for aerobic mesophilic bacteria
Test final rinse water for aerobic mesophilic bacteria in accordance with ISO 15883-1:2006+Amd 1:2014, 6.4.2.4, and Annex D of this document.
NOTE Specific microbiological media can be used for the detection of certain types of microorganisms (e.g.
for Pseudomonas aeruginosa).
E.3.3 Test for environmental (atypical) Mycobacterium sp.
Filter a 100 ml aliquot of the sample under vacuum through a 0,2 µm filter that is of appropriate size to
allow its transfer and incubation as described below (e.g. 47 mm diameter).
Transfer the filter aseptically to the surface of a Middlebrook6) 7H10 Agar plate and incubate at (30 ± 2) °C. The plates should be read regularly. Incubation should be continued for 28 d before it is concluded that no growth has occurred.
The agar plate should be sealed to prevent dehydration of the growth medium.
Carry out the test in duplicate. Examine the filters weekly and count and record the number of colonies
of bacterial growth.
6) Equivalent media can be used if they can be shown to lead to the same results.
Copyright International Org©anizIaStioOn fo2r S0ta1n8dar–dizAatiloln rights reserved
Provided by IHS Markit under license with ANSI
No reproduction or networking permitted without license from IHS
Order Number: 02223302 53
Sold to:CANTEL MEDICAL *DA [001612] - SMARTIN@MEDIVATORS.COM, Not for Resale,2018-12-18 15:39:13 UTC
ISO 15883-4:2018(E)
Record the mean number of colony forming units per sample.
NOTE If plates are overgrown by relatively faster growing contaminants within 48 h to 72 h, it might be necessary to resample and perform a validated preliminary partial decontamination of the sample with one or more chemicals to which mycobacterial species are more resistant than the other organisms.
If growth of (atypical) Mycobacterium sp. is observed consideration should be given to having the
cultures transferred to a specialist laboratory for identification of the mycobacterial strains isolated.
E.4 Results/Acceptance criteria
Record the number of aerobic mesophilic bacteria per 100 ml sample of final rinse water;
Report the number of Pseudomonas aeruginosa in 100 ml, and (atypical) Mycobacterium sp. in 100 ml.
There are fewer than 10 CFU/100 ml sample of final rinse water and the water is free from Pseudomonas aeruginosa in 100 ml, and (atypical) Mycobacterium sp. in 100 ml (see 6.3).
Copyright In5ter4national Organization for Standardization
Order Number: 02223302
© ISO 2018 – All rights reserved
Provided by IHS Markit under license with ANSI
No reproduction or networking permitted without license from IHS
Sold to:CANTEL MEDICAL *DA [001612] - SMARTIN@MEDIVATORS.COM, Not for Resale,2018-12-18 15:39:13 UTC
Annex F
(informative)
Additional notes on microbiological testing of chemical disinfection processes
F.1 Difficulties with microbial testing
There are a number of difficulties associated with microbiological monitoring of the disinfection process in a WD. These include, but are not limited to, the following:
a) The end-point which is desired in practice (no survivors) does not allow quantitative interpretation of the results and does not provide assurance that the recovery method used would detect surviving organisms.
b) Artificial inoculation of surfaces to be disinfected might not adequately simulate the naturally occurring microflora because both the resistance of the organisms and the adhesion of the organisms to the surface can be changed by in vitro culture and preparative methods (harvesting, cleaning, inoculation etc.).
c) “Worst-case” conditions can be created by the use of high numbers of microorganisms that are also necessary to give quantifiable results. However, these might not be representative of naturally occurring populations due to clumping etc.
d) The addition of organic material (usually serum or blood) and/or inorganic material (usually the mineral salts causing hardness of water) can be used to simulate soiling but there are few data to support the correlation of these artificial soils with naturally occurring soiling.
e) The organisms that are normally of interest are pathogens (both obligate and facultative or opportunistic) but the use of non-pathogenic strains is necessary for test purposes. In many cases the evidence correlating the behaviour and resistance of the different species and strains is scant or absent.
f) The surfaces of particular interest are frequently the internal surfaces of devices with long narrow lumens. Their inaccessibility makes quantitative inoculation and recovery more difficult.
F.2 Verification of the disinfection process
During normal processing the cleaning and rinsing stages of a WD cycle are designed to remove surface
soiling and should therefore remove most of the contaminating microorganisms.
In carrying out tests to verify the efficacy of the chemical disinfection process it is therefore necessary either:
a) to evaluate the removal of microorganisms which occurs during the cleaning and rinsing stages and demonstrate that this removal efficacy is reproducible within acceptable limits (i.e. such that for a known initial contaminating population there will be a known residual population present at the start of the disinfection stage); or
b) to eliminate the cleaning and rinsing stages of the cycle during the test runs for evaluation of chemical disinfection efficacy.
In either case the exposure to disinfectant solution and then its removal with rinse water will also cause the physical removal of microorganisms and the extent to which this occurs should be evaluated as part of the validation of the test method.
Copyright International Org©anizIaStioOn fo2r S0ta1n8dar–dizAatiloln rights reserved
Provided by IHS Markit under license with ANSI
No reproduction or networking permitted without license from IHS
Order Number: 02223302 55
Sold to:CANTEL MEDICAL *DA [001612] - SMARTIN@MEDIVATORS.COM, Not for Resale,2018-12-18 15:39:13 UTC
ISO 15883-4:2018(E)
F.3 Validation of the test method
Validation of the test method should demonstrate:
a) the ability to produce a reproducible population of microorganisms (on the surface to be disinfected) by the chosen inoculation method; this should include determination of the loss of viable organisms as the inoculum dries on to the surface;
b) the extent to which these organisms are lost from the surface by the physical action of the disinfection and post-disinfection rinsing process; during evaluation of this effect it is necessary to ensure that any surfactants/detergents normally present in the disinfectant, or any similar effect of the disinfectant moiety, are evaluated.
NOTE 1 This can be undertaken by
1) preparing a solution of surfactant and estimating its antimicrobial activity against the test
organisms using an in vitro suspension test;
2) evaluating and comparing the extent of removal with water and with a surfactant solution (after correction for the “error” caused by the previously determined inactivation effect);
3) the ability to neutralize the disinfectant; the neutralizer solution will then be used instead of water for the post-disinfection rinse (the extent to which organisms are physically removed by the neutralizing rinse will also need to be evaluated);
4) the extent to which the remaining microorganisms are detected (or removed) by the recovery method.
NOTE 2 Methods in which
1) suspensions of microorganisms are flushed through the lumen of a device and are assumed
to adhere in large numbers;
2) the device(s) are then exposed to liquid disinfectants flushed through the lumen which it is assumed does not physically remove any of the deposited microorganisms;
3) evaluation for the lethal effect of the disinfectant is carried out by flushing the lumen with an eluate solution, which it is assumed removes close to 100 % of the surviving population, and then enumerating the viable microorganisms in the eluate; are unacceptable in the absence of systematic validation and justification for each of the assumptions made.
--`,,,,````,``,,``,,,``,-`-``,```,,,`---
Copyright International Organization for Standardization
Order Number: 02223302
© ISO 2018 – All rights reserved
|
56 |
Provided by IHS Markit under license with ANSI
No reproduction or networking permitted without license from IHS
|
56 |
Sold to:CANTEL MEDICAL *DA [001612] - SMARTIN@MEDIVATORS.COM, Not for Resale,2018-12-18 15:39:13 UTC
Annex G
(informative)
Typical specifications of trumpet valves and connection ports
G.1 Specification diagrams
The diagrams displayed in Figures G.1 to G.6 show typical specifications of trumpet valves and ports
for connection of endoscopes in WD.
Tolerances for all diagrams should be +0,1 mm for holes, 0
mm for shafts and ± 0,1 mm for others.
0
Key
1 elevator channel access port
2 suction valve cylinder
3 air/water valve cylinder
4 biopsy port
-0,1
Dimensions in millimetres
Figure G.1 — Overview of the control body — Position of valves and ports
Copyright International Org©anizIaStioOn fo2r S0ta1n8dar–dizAatiloln rights reserved
Provided by IHS Markit under license with ANSI
No reproduction or networking permitted without license from IHS
Order Number: 02223302 57
Sold to:CANTEL MEDICAL *DA [001612] - SMARTIN@MEDIVATORS.COM, Not for Resale,2018-12-18 15:39:13 UTC
ISO 15883-4:2018(E)
Dimensions in millimetres
a To distal end.
Figure G.2 — Example of an elevator channel access port
Copyright In5ter8national Organization for Standardization
Order Number: 02223302
© ISO 2018 – All rights reserved
Provided by IHS Markit under license with ANSI
No reproduction or networking permitted without license from IHS
Sold to:CANTEL MEDICAL *DA [001612] - SMARTIN@MEDIVATORS.COM, Not for Resale,2018-12-18 15:39:13 UTC
ISO 15883-4:2018(E)
Dimensions in millimetres
a To light/video connector.
b To biopsy port and distal end.
Figure G.3 — Example of a suction valve cylinder
Copyright International Org©anizIaStioOn fo2r S0ta1n8dar–dizAatiloln rights reserved
Provided by IHS Markit under license with ANSI
No reproduction or networking permitted without license from IHS
Order Number: 02223302 59
Sold to:CANTEL MEDICAL *DA [001612] - SMARTIN@MEDIVATORS.COM, Not for Resale,2018-12-18 15:39:13 UTC
ISO 15883-4:2018(E)
Dimensions in millimetres
a To light/video connector.
b To distal end.
Figure G.4 — Example of an air/water valve cylinder
Copyright In6ter0national Organization for Standardization
Order Number: 02223302
© ISO 2018 – All rights reserved
Provided by IHS Markit under license with ANSI
No reproduction or networking permitted without license from IHS
Sold to:CANTEL MEDICAL *DA [001612] - SMARTIN@MEDIVATORS.COM, Not for Resale,2018-12-18 15:39:13 UTC
ISO 15883-4:2018(E)
Dimensions in millimetres
a To suction valve.
b To distal end.
Figure G.5 — Example of a biopsy port
Copyright International Org©anizIaStioOn fo2r S0ta1n8dar–dizAatiloln rights reserved
Provided by IHS Markit under license with ANSI
No reproduction or networking permitted without license from IHS
Order Number: 02223302 61
Sold to:CANTEL MEDICAL *DA [001612] - SMARTIN@MEDIVATORS.COM, Not for Resale,2018-12-18 15:39:13 UTC
ISO 15883-4:2018(E)
Dimensions in millimetres
a To distal end.
b To air/water valve.
c To air/water valve.
NOTE See Annex H for lengths and diameters of tubing.
Figure G.6 — Example of Y-junction between water and air channel
Copyright In6ter2national Organization for Standardization
Order Number: 02223302
© ISO 2018 – All rights reserved
Provided by IHS Markit under license with ANSI
No reproduction or networking permitted without license from IHS
Sold to:CANTEL MEDICAL *DA [001612] - SMARTIN@MEDIVATORS.COM, Not for Resale,2018-12-18 15:39:13 UTC
Annex H
(normative)
Establishing endoscope type test groups
H.1 General
This Annex is intended to be used by WD manufacturers to provide a rationale for their choice of endoscope type test groups.
The devices for which evidence exists that they can be processed satisfactorily in the WD shall be specified [see 8 a)]. This implies that a number of the type tests (see 6.6, 6.7, 6.8 and 6.11) shall be carried out for every flexible endoscope on the list. Considering the vast number of flexible endoscopes that are in use in the healthcare settings at any given moment (different brands, types, generations), this is impossible to do. The work load can be reduced by grouping the devices based on the similarities of design. The type tests can then be performed on a representative sample of each of these endoscope type test groups (see Table H.1).
H.2 Establishing endoscope type test groups
General as well as other critical design elements of flexible endoscopes shall be considered when clustering endoscopes in endoscope type test groups. The following critical design element shall be taken into consideration:
a) the same general channel design as specified in Table H.2, and
b) similarity of specific characteristics affecting the flow conditions in the endoscope, including:
— ports;
— connectors;
— channel separators;
— port closures;
— internal non-return valves;
— restrictions of channels;
— internal connection between channels;
— design of distal end ports (e.g. nozzle);
— supply connector;
— design of light guide connector ports (e.g. valves);
— design of trumpet valve cylinder;
— etc.
Copyright International Org©anizIaStioOn fo2r S0ta1n8dar–dizAatiloln rights reserved
Provided by IHS Markit under license with ANSI
No reproduction or networking permitted without license from IHS
Order Number: 02223302 63
Sold to:CANTEL MEDICAL *DA [001612] - SMARTIN@MEDIVATORS.COM, Not for Resale,2018-12-18 15:39:13 UTC
ISO 15883-4:2018(E)
The following procedure shall be followed:
a) Establish the specifications for the channels in the endoscope (see Table H.1). This shall include the length and diameter of each channel. This relevant information as specified in Table H.2 shall be obtained. If this information is not available, then this endoscope shall not be included in the list of compatible devices.
b) Assign all endoscopes for which the WD manufacturer intends to claim compatibility into a block or combination of blocks according to Table H.2.
NOTE The blocks under Table H.2 were established based upon the majority of currently marketed
endoscopes.
c) Special attention shall be paid to constructions such as endoscopes containing balloon channels.
d) Each block combination shall be further reviewed with respect to the other critical design elements as specified in H.2.1, and any other design characteristic affecting the flow and pressure conditions in the endoscope, are represented by the block combination.
e) Where one or more channels of the endoscope are not represented by any of the blocks in Table H.2, establish the specifications of the additional or modified block. Record the rationale for designing a new block or modifying an existing block.
f) An endoscope type test group shall consist of the same general block combination and be similar in its specific characteristics affecting the flow conditions in the endoscope.
NOTE Refer to Table H.1 for examples of establishing endoscope type test groups for WD type testing.
H.3 Choosing relevant endoscope type test groups for type testing
The procedure according to H.2 can result in a large variety of endoscope type test groups.
Based on a risk assessment, the most relevant endoscope type test groups shall be selected (see Table H.1) for inclusion in WD type testing, taking into consideration the specific characteristics and limitations of the specific WD.
The risk assessment should consider, and where necessary, include measurement of parameters that can influence the efficacy of the process (such as pressure, process fluid flow, etc.) in combination with the WD.
Copyright In6ter4national Organization for Standardization
Order Number: 02223302
© ISO 2018 – All rights reserved
Provided by IHS Markit under license with ANSI
No reproduction or networking permitted without license from IHS
Sold to:CANTEL MEDICAL *DA [001612] - SMARTIN@MEDIVATORS.COM, Not for Resale,2018-12-18 15:39:13 UTC
ISO 15883-4:2018(E)
Table H.1 — Example for establishing relevant endoscope type test groups for WD type testing
|
Endoscope |
Endoscope block |
Channel connector |
Separator (X)/ closure (Y) |
Endoscope type test group (TTG) |
Relevant for type test |
|
1 |
A1 |
1 |
X1 |
TTG1 |
No - based on risk assessment |
|
2 | |||||
|
B1 |
1 |
Y1 | |||
|
3 | |||||
|
2 |
A1 |
1 |
X2 |
TTG2 |
Yes - based on the risk assessment |
|
2 | |||||
|
B1 |
1 |
Y1 | |||
|
3 | |||||
|
3 |
A2 |
1 |
X1 |
TTG3 |
No - based on risk assessment |
H.4 Definition of relevant surrogate devices and endoscopes for type testing
Type testing shall be performed with the help of surrogate devices and/or representative endoscopes from every relevant type test group as specified in the test procedures described in this document. When a surrogate device is used it shall be verified to ensure that the critical design elements (as listed in H.2) are met and it has similar flow characteristics as the original device(s), using the following procedure:
a) Determine the specifications for the channels and the ports in the endoscope as in H.2.1.
b) From these specifications (see H.2.2), develop a channel irrigation plan. This plan shall ensure that all channels and all parts of the channels are effectively irrigated during the process.
c) Specify the necessary channel connectors to connect the endoscope channels to the WD. Where applicable, specify any channel separators and/or port closures. The connectors shall ensure that the channels will be irrigated according to the irrigation plan. The channel connectors shall also be used to connect the surrogate device to the WD.
d) During an operating cycle, measure and record the flow and pressure at each connection to the
endoscope.
e) From the blocks identified in H.2.1, build a surrogate device that represents the complete set of channels of the endoscope and its ports and define the necessary connectors.
f) During an operating cycle, with all connectors to the surrogate device in place, measure and record the flow and pressure at each connection to each channel of the surrogate device.
g) All channels shall be connected to ensure that the flow through any channel is realistically influenced by the other connected channels. The extent of the inter-channel influence can depend on the type of irrigation system of the particular WD.
h) Establish whether the flow and pressure values at each connection to the surrogate device representative of the relevant endoscope type test group (TTG) is equal to the flow and pressure values at each connection to the original endoscope(s). This is necessary in order to verify that the surrogate device correctly represents the original endoscope(s).
If it cannot be established that the surrogate device is a valid model for the endoscope(s), then repeat procedure from H.4 a), or abandon the procedure as the endoscope was not qualified for processing in the WD.
After establishing the relevant surrogate device(s) and endoscopes, perform the type test(s).
Copyright International Org©anizIaStioOn fo2r S0ta1n8dar–dizAatiloln rights reserved
Provided by IHS Markit under license with ANSI
No reproduction or networking permitted without license from IHS
Order Number: 02223302 65
Sold to:CANTEL MEDICAL *DA [001612] - SMARTIN@MEDIVATORS.COM, Not for Resale,2018-12-18 15:39:13 UTC
ISO 15883-4:2018(E)
After successful completion of WD type testing, the WD manufacturer may declare compatibility with all endoscopes that are included in the establishment of the endoscope type test groups according to H.2.
H.5 Procedure for new endoscopes
The following procedure shall be followed:
a) Assess the new endoscope for compatibility and assign it to a block or combination of blocks according to it specific characteristics and Table H.2.
b) Check whether the new endoscope consists of the same general block combination and is similar with regard to specific characteristics affecting the flow conditions in the endoscope,
e.g. connectors, channel separators, port closures, return valves, etc. with one of the previously established endoscope type test groups.
c) In case of doubt, verify that the flow through the channels of the new endoscope is similar, when
measured as described in H.4 d).
d) If all of these conditions are satisfied, then the endoscope is a member of the endoscope type test group and may be added to the list of compatible endoscopes without the necessity of further testing. The results of this assessment shall be documented.
e) If the new endoscope does not belong to any previously established endoscope type test group, then it becomes the first member of a new endoscope type test group. Based on an additional risk assessment for this new endoscope type test group, it shall be stated whether the type testing already covers the new endoscope type test group or if further type testing is required.
H.6 List of endoscope blocks
Examples of specified endoscope blocks are provided in Table H.2. Deviations to the length and internal
diameter specifications in the table can be acceptable, if justified.
Copyright In6ter6national Organization for Standardization
Order Number: 02223302
© ISO 2018 – All rights reserved
Provided by IHS Markit under license with ANSI
No reproduction or networking permitted without license from IHS
Sold to:CANTEL MEDICAL *DA [001612] - SMARTIN@MEDIVATORS.COM, Not for Resale,2018-12-18 15:39:13 UTC
ISO 15883-4:2018(E)
Table H.2 — Examples of specified endoscope blocks
|
Endoscope Block A, air/water channels |
Specification | |
|
A1 |
|
Single air channel and water channel: |
|
|
|
— not combined |
|
|
|
— Ø 0,7 mm ≤ d ≤ Ø 1,7 mm |
|
|
Key L1: valve to distal end |
Channel lengths: — 600 mm < L1 < 2 600 mm |
|
|
L2: valve to connector |
— 800 mm < L2 < 2 000 mm |
|
A2 |
|
Single air channel and water channel: |
|
|
|
— combined |
|
|
|
— Ø 0,8 mm ≤ d ≤ Ø 2,4 mm |
|
|
|
Channel lengths: |
|
|
Key |
— 900 mm < L1 < 2 900 mm |
|
|
L1: valve to distal end |
— 1 400 mm < L2 < 2 000 mm |
|
|
L2: valve to connector |
|
|
A3 |
|
Single air channel and water channel: |
|
|
|
— combined |
|
|
|
— Ø 0,7 mm ≤ d ≤ Ø 1,7 mm |
|
|
Key L1: valve to distal end |
Channel lengths: — 600 mm < L1 < 2 600 mm |
|
|
L2: valve to connector |
— 800 mm < L2 < 2 000 mm |
|
A4 |
|
Single air channel and water channel: |
|
|
|
— combined |
|
|
|
— Ø 0,7 mm ≤ d ≤ Ø 1,7 mm |
|
|
Key L1: valve to distal end |
Channel lengths: — 600 mm < L1 < 2 600 mm |
|
|
L2: valve to connector |
— 800 mm < L2 < 2 000 mm |
Copyright International Org©anizIaStioOn fo2r S0ta1n8dar–dizAatiloln rights reserved
Order Number: 02223302
--`,,,,````,``,,``,,,``,-`-``,```,,,`---
67
Provided by IHS Markit under license with ANSI
No reproduction or networking permitted without license from IHS
Sold to:CANTEL MEDICAL *DA [001612] - SMARTIN@MEDIVATORS.COM, Not for Resale,2018-12-18 15:39:13 UTC
ISO 15883-4:2018(E)
![]()
Table H.2 (continued)
|
A5 |
|
Single air channel and water channel: |
|
|
|
— Combined with balloon fill channel |
|
|
|
Air channel and water channel: |
|
|
|
— Ø 0,8 mm ≤ d ≤ Ø 1,2 mm |
|
|
Key |
Balloon channel: |
|
|
1: balloon fill channel |
— Ø 0,8 mm ≤ d ≤ Ø 1,2 mm |
|
|
L1: valve to distal end L2: valve to connector |
Channel lengths: |
|
|
|
— 1 200 mm < L1 < 2 200 mm |
|
|
|
— 1 600 mm < L2 < 2 000 mm |
Copyright In6ter8national Organization for Standardization
Order Number: 02223302
© ISO 2018 – All rights reserved
Provided by IHS Markit under license with ANSI
No reproduction or networking permitted without license from IHS
Sold to:CANTEL MEDICAL *DA [001612] - SMARTIN@MEDIVATORS.COM, Not for Resale,2018-12-18 15:39:13 UTC
ISO 15883-4:2018(E)
Table H.2 (continued)
|
Endoscope Block B, Biopsy suction channels |
Specification | |
|
B1 |
|
Biopsy/suction channel: |
|
|
|
— Ø 1,2 mm ≤ d ≤ Ø 2,5 mm |
|
|
|
Channel lengths: |
|
|
Key |
— 600 mm < L1 < 2 800 mm |
|
|
L1: biopsy port to distal end |
— 1 400 mm < L2 < 2 000 mm |
|
|
L2: valve to connector |
— L3 < 300 mm |
|
|
L3: suction channel to valve |
|
|
B2 |
|
Biopsy/suction channel: |
|
|
|
— Ø 2,5 mm ≤ d ≤ Ø 4,5 mm |
|
|
|
Channel lengths: |
|
|
Key |
— 1 200 mm < L1 < 2 200 mm |
|
|
L1: biopsy port to distal end |
— 1 400 mm < L2 < 2 000 mm |
|
|
L2: valve to connector |
— L3 < 200 mm |
|
|
L3: suction channel to valve |
|
|
B3 |
|
Biopsy/suction channel: |
|
|
|
— Ø 4,5 mm ≤ d ≤ Ø 6,5 mm |
|
|
|
Channel lengths: |
|
|
Key |
— 600 mm < L1 < 1 200 mm |
|
|
L1: biopsy port to distal end |
— 1 400 mm < L2 < 2 000 mm |
|
|
L2: valve to connector |
— L3 < 200 mm |
|
|
L3: suction channel to valve |
|
|
B4 |
|
Double biopsy/suction channel: |
|
|
|
— Valve |
|
|
|
— Ø 2,5 mm ≤ d ≤ Ø 4,5 mm |
|
|
Key |
Channel lengths: |
|
|
L1: biopsy port to distal end |
— 1 100 mm < L1 < 2 200 mm |
|
|
L2: valve to connector |
— 1 400 mm < L2 < 2 000 mm |
|
|
L3: suction channel to valve |
— L3 < 200 mm |
|
B5 |
|
Double biopsy/suction channel: |
|
|
|
— Ø 2,5 mm ≤ d ≤ Ø 4,5 mm |
|
|
|
Channel lengths: |
|
|
Key |
— 1 100 mm < L1 < 2 200 mm |
|
|
L1: biopsy port to distal end |
— 1 400 mm < L2 < 2 000 mm |
|
|
L2: valve to connector |
— L3 < 300 mm |
|
|
L3: suction channel to valve |
|
Copyright International Org©anizIaStioOn fo2r S0ta1n8dar–dizAatiloln rights reserved
Provided by IHS Markit under license with ANSI
No reproduction or networking permitted without license from IHS
![]()
Order Number: 02223302 69
Sold to:CANTEL MEDICAL *DA [001612] - SMARTIN@MEDIVATORS.COM, Not for Resale,2018-12-18 15:39:13 UTC
ISO 15883-4:2018(E)
Table H.2 (continued)
|
B6 |
Key 1: balloon drain channel L1: biopsy port to distal end L2: valve to connector L3: suction channel to valve |
Biopsy/suction channel: — Ø 1,2 mm ≤ d ≤ Ø 2,5 mm Balloon drain channel: — Ø 0,8 mm ≤ d ≤ Ø 1,2 mm Channel lengths: — 1 200 mm < L1 < 2 200 mm — 1 400 mm < L2 < 2 000 mm — L3 < 200 mm |
|
B7 |
|
Biopsy/suction channel: |
|
|
|
— Ø 1,2 mm ≤ d ≤ Ø 2,5 mm |
|
|
|
Balloon drain channel with valve: |
|
|
Key |
— Ø 0,8 mm ≤ d ≤ Ø 1,2 mm |
|
|
1: balloon drain channel |
Channel lengths: |
|
|
L1: biopsy port to distal end |
— 1 200 mm < L1 < 2 200 mm |
|
|
L2: valve to connector L3: suction channel to valve |
— 1 400 mm < L2 < 2 000 mm — L3 < 200 mm |
Copyright In7ter0national Organization for Standardization
|
|
| ||
|
|
| ||
|
|
| ||
Order Number: 02223302
© ISO 2018 – All rights reserved
Provided by IHS Markit under license with ANSI
No reproduction or networking permitted without license from IHS
Sold to:CANTEL MEDICAL *DA [001612] - SMARTIN@MEDIVATORS.COM, Not for Resale,2018-12-18 15:39:13 UTC
ISO 15883-4:2018(E)
Table H.2 (continued)
|
Endoscope Block C, water jet channel/air balloon chan- nel double balloon system |
Specification | |
|
C1 |
Key L: water jet or balloon connector to distal end |
Water jet channel: — Ø 0,7 mm ≤ d ≤ Ø 1,6 mm — L = L1 of Block A — L = L1 of Block A + L2 of Block A |
|
C2 |
Key L: balloon connector to distal end |
Balloon channel: — Ø 0,6 mm ≤ d ≤ Ø 1,5 mm Channel lengths: — L = L1 of block A — L = L1 of block A +L2 of block A |
Copyright International Org©anizIaStioOn fo2r S0ta1n8dar–dizAatiloln rights reserved
Provided by IHS Markit under license with ANSI
No reproduction or networking permitted without license from IHS
--`,,,,````,``,,``,,,``,-`-``,```,,,`---
|
71 |
Order Number: 02223302
Sold to:CANTEL MEDICAL *DA [001612] - SMARTIN@MEDIVATORS.COM, Not for Resale,2018-12-18 15:39:13 UTC
ISO 15883-4:2018(E)
Table H.2 (continued)
|
Endoscope Block D, elevator channel |
Specification | |
|
D |
|
Elevator channel: |
|
|
Key |
— Wire: Ø 0,3 mm ≤ d ≤ Ø 0,8 mm |
|
|
L: control body to distal end |
— Channel: Ø 0,8 mm ≤ d ≤ Ø 1,2 mm |
|
|
|
— Delta 0,1 mm ≤ d ≤ 0,4 mm |
|
|
|
Channel lengths: |
|
|
|
— 1 000 mm < L < 1 700 mm |
Copyright In7ter2national Organization for Standardization
Order Number: 02223302
© ISO 2018 – All rights reserved
Provided by IHS Markit under license with ANSI
No reproduction or networking permitted without license from IHS
Sold to:CANTEL MEDICAL *DA [001612] - SMARTIN@MEDIVATORS.COM, Not for Resale,2018-12-18 15:39:13 UTC
ISO 15883-4:2018(E)
![]()
Table H.2 (continued)
|
Endoscope Block E, small diameter endoscopes (e.g. cystoscopes, bronchoscopes) |
Specification | |
|
E1 |
Key L: biopsy port to distal end |
Biopsy/suction channel: — Ø 0,5 mm ≤ d ≤ Ø 3,4 mm Channel lengths: — 300 mm < L < 1 000 mm |
|
E2 |
Key L1: biopsy port to distal end L2: suction channel to valve |
Biopsy/suction channel: — Ø 0,5 mm ≤ d ≤ Ø 3,4 mm Channel lengths: — 300 mm < L1 < 1 000 mm — L2 < 300 mm |
Copyright International Org©anizIaStioOn fo2r S0ta1n8dar–dizAatiloln rights reserved
Provided by IHS Markit under license with ANSI
No reproduction or networking permitted without license from IHS
Order Number: 02223302 73
Sold to:CANTEL MEDICAL *DA [001612] - SMARTIN@MEDIVATORS.COM, Not for Resale,2018-12-18 15:39:13 UTC
ISO 15883-4:2018(E)
Examples of endoscopes that cannot be divided into endoscope blocks due to interconnections between water/air and the biopsy/suction channels or combinations with balloon channels are described in Table H.3. Deviations to the length and internal diameter specifications in the table can be acceptable, if justified.
![]()
Table H.3 — Examples of endoscopes that cannot be divided into endoscope blocks due to interconnections
|
Diagrams of endoscopes that cannot be divided into endoscope blocks due to interconnections between water/air and biopsy/suction channels or combinations with balloon channels |
Specification |
|
|
Ultrasound endoscope |
|
|
Air channel and water channel: |
|
|
— Ø 0,8 mm ≤ d ≤ Ø 2,4 mm |
|
|
Biopsy/suction channel: |
|
|
— Ø 1,2 mm ≤ d ≤ Ø 3,7 mm |
|
Key |
Balloon channel: |
|
1: balloon channel |
— Ø 0,8 mm ≤ d ≤ Ø 1,4 mm |
|
2: biopsy/suction channel |
Channel lengths: |
|
L1: air/water channel to distal end L2: valve to connector L3: suction channel to valve |
— 1 200 mm < L1 < 2 200 mm — 1 400 mm < L2 < 2 000 mm |
|
|
— L3 < 300 mm |
|
|
Ultrasound endoscope |
|
|
Air channel and water channel: |
|
|
— Ø 0,8 mm ≤ d ≤ Ø 1,2 mm |
|
|
Biopsy/suction channel: |
|
|
— Ø 1,2 mm ≤ d ≤ Ø 2,5 mm |
|
Key 1: balloon channel 2: biopsy/suction channel |
Balloon channel: — Ø 0,8 mm ≤ d ≤ Ø 1,2 mm |
|
L1: air/water channel to distal end |
Channel lengths: |
|
L2: valve to connector |
— 1 200 mm < L1 < 2 200 mm |
|
L3: suction channel to valve |
— 1 400 mm < L2 < 2 000 mm |
|
|
— L3 < 200 mm |
Copyright In7ter4national Organization for Standardization
Order Number: 02223302
© ISO 2018 – All rights reserved
Provided by IHS Markit under license with ANSI
No reproduction or networking permitted without license from IHS
Sold to:CANTEL MEDICAL *DA [001612] - SMARTIN@MEDIVATORS.COM, Not for Resale,2018-12-18 15:39:13 UTC
ISO 15883-4:2018(E)
![]()
Table H.3 (continued)
|
Diagrams of endoscopes that cannot be divided into endoscope blocks due to interconnections between water/air and biopsy/suction channels or combinations with balloon channels |
Specification |
|
|
Ultrasound endoscope |
|
|
Air channel and water channel: |
|
|
— Ø 0,8 mm ≤ d ≤ Ø 1,2 mm |
|
|
Biopsy/suction channel: |
|
Key 1: balloon channel |
— Ø 1,2 mm ≤ d ≤ Ø 2,5 mm Balloon channel: |
|
2: biopsy/suction channel |
— Ø 0,8 mm ≤ d ≤ Ø 1,2 mm |
|
L1: air/water channel to distal end |
Channel lengths: |
|
L2: valve to connector |
— 1 200 mm < L1 < 2 200 mm |
|
L3: suction channel to valve |
— 1 400 mm < L2 < 2 000 mm |
|
|
— L3 < 200 mm |
|
|
Paediatric GI endoscope |
|
|
Air channel, water channel, biopsy, suction: |
|
|
— Ø 1,2 mm ≤ d ≤ Ø 2,5 mm |
|
|
Channel lengths: |
|
|
— 1 200 mm < L1 < 2 200 mm |
|
Key |
— 1 400 mm < L2 < 2 000 mm |
|
L1: biopsy port to distal end |
— L3 < 200 mm |
|
L2: valve to connector |
|
|
L3: suction channel to valve |
|
Copyright International Org©anizIaStioOn fo2r S0ta1n8dar–dizAatiloln rights reserved
Provided by IHS Markit under license with ANSI
No reproduction or networking permitted without license from IHS
Order Number: 02223302 75
Sold to:CANTEL MEDICAL *DA [001612] - SMARTIN@MEDIVATORS.COM, Not for Resale,2018-12-18 15:39:13 UTC
Annex I
(informative)
Establishing endoscope product families
I.1 General
This Annex provides guidance for performance of Performance Qualification (PQ) at the user’s facility
(see Table C.2).
It is the responsibility of the health care facility to ensure that the choice of WD, process chemicals, operating cycles and quality of service is appropriate for the particular load used in the respective endoscopy unit.
For performance qualification the process is verified by sampling endoscopes and determining their hygienic status (see 6.11 and 6.12.6.3). Clustering endoscopes into endoscope product families can reduce the number of endoscopes required to be sampled for performance qualification, but still allow for coverage of the range of endoscopes used in the respective healthcare facility.
Three endoscope product families have been identified and defined based on the relevant characteristics of endoscopes (see I.2). For endoscopes that do not belong to one of these three endoscope product families, or for a different brand endoscope, or for endoscopes that have a different connector set, further tests need to be performed.
I.2 Classification of endoscope product families
I.2.1 Endoscope product family 1
Endoscope product family 1 includes endoscopes
— with air/water channels,
— with biopsy/suction channel,
— with/without additional instrument channel,
— with/without water jet channel.
Endoscopes belonging to this product family are typically intended for use in the gastrointestinal (GI) tract. Gastroscopes and colonoscopies are the main representatives of this endoscope product family, and duodenoscopes with an encapsulated elevator wire, also belong to this group (see Figure I.1).
Copyright In7ter6national Organization for Standardization
Order Number: 02223302
© ISO 2018 – All rights reserved
Provided by IHS Markit under license with ANSI
No reproduction or networking permitted without license from IHS
Sold to:CANTEL MEDICAL *DA [001612] - SMARTIN@MEDIVATORS.COM, Not for Resale,2018-12-18 15:39:13 UTC
ISO 15883-4:2018(E)
Key
1 biopsy/suction channel
2 air channel
3 water channel
4 water jet channel
Figure I.1 — Endoscope product family 1
I.2.2 Endoscope product family 2
Endoscope product family 2 includes endoscopes
— with air/water channels,
— with biopsy/suction channel,
— with/without additional instrument channel,
![]()
— with/without elevator wire channel,
— with up to two control channels for balloon functions.
Endoscopes belonging to this product family include models which can be used in the gastrointestinal tract. They are equipped with a so-called elevator wire channel and/or control channels, the latter designed to fill and deflate balloons as components of the endoscope. Examples for this product family are duodenoscopes with open elevator channel, endoscopes for endoscopic ultrasound, and enteroscopes (see Figure I.2).
Copyright International Org©anizIaStioOn fo2r S0ta1n8dar–dizAatiloln rights reserved
Provided by IHS Markit under license with ANSI
No reproduction or networking permitted without license from IHS
Order Number: 02223302 77
Sold to:CANTEL MEDICAL *DA [001612] - SMARTIN@MEDIVATORS.COM, Not for Resale,2018-12-18 15:39:13 UTC
ISO 15883-4:2018(E)
Key
1 biopsy /suction channel
2 air channel
3 water channel
4 elevator channel
5 balloon channel
Figure I.2 — Endoscope product family 2
I.2.3 Endoscope product family 3
Endoscope product family 3 includes endoscopes
— with up to two instrument channels, but without channel system in the umbilical cord, or
— without any channels within the entire endoscope.
Endoscopes belonging to this product family comprise models with only one channel system for biopsy, irrigation and suction, or models without any channel. They are used in bronchoscopy, ear-nose-throat applications, gynaecology and urology (see Figure I.3).
NOTE During the verification procedures consideration can be given to the clinical use of the endoscope.
Copyright In7ter8national Organization for Standardization
Order Number: 02223302
© ISO 2018 – All rights reserved
Provided by IHS Markit under license with ANSI
No reproduction or networking permitted without license from IHS
Sold to:CANTEL MEDICAL *DA [001612] - SMARTIN@MEDIVATORS.COM, Not for Resale,2018-12-18 15:39:13 UTC
ISO 15883-4:2018(E)
Key
1 biopsy/suction channel
Figure I.3 — Endoscope product family 3
Copyright International Org©anizIaStioOn fo2r S0ta1n8dar–dizAatiloln rights reserved
Provided by IHS Markit under license with ANSI
No reproduction or networking permitted without license from IHS
Order Number: 02223302 79
Sold to:CANTEL MEDICAL *DA [001612] - SMARTIN@MEDIVATORS.COM, Not for Resale,2018-12-18 15:39:13 UTC
Bibliography
[1] ISO 384, Laboratory glass and plastics ware — Principles of design and construction of volumetric instruments
[2] ISO 11138-1, Sterilization of health care products — Biological indicators — Part 1: General requirements
[3] ISO 11737-1, Sterilization of health care products — Microbiological methods — Part 1:
Determination of a population of microorganisms on products
[4] EN 1822-1, High efficiency air filters (EPA, HEPA and ULPA) — Part 1: Classification, performance testing, marking
[5] EN 13624, Chemical disinfectants and antiseptics — Quantitative suspension test for the evaluation of fungicidal or yeasticidal activity in the medical area — Test method and requirements (phase 2, step 1)
[6] EN 14347, Chemical disinfectants and antiseptics — Basic sporicidal activity — Test method and requirements (phase 1, step 1)
[7] EN 14348, Chemical disinfectants and antiseptics — Quantitative suspension test for the evaluation of mycobactericidal activity of chemical disinfectants in the medical area including instrument disinfectants — Test methods and requirements (phase 2, step 1)
[8] EN 14476+A1, Chemical disinfectants and antiseptics — Quantitative suspension test for the evaluation of virucidal activity in the medical area — Test method and requirements (phase 2, step 1)
[9] EN 14561, Chemical disinfectants and antiseptics — Quantitative carrier test for the evaluation of bactericidal activity for instruments used in the medical area — Test method and requirements (phase 2, step 2)
[10] EN 14562, Chemical disinfectants and antiseptics — Quantitative carrier test for the evaluation of fungicidal or yeasticidal activity for instruments used in the medical area — Test method and requirements (phase 2, step 2)
[11] EN 14563, Chemical disinfectants and antiseptics — Quantitative carrier test for the evaluation of mycobactericidal or tuberculocidal activity of chemical disinfectants used for instruments in the medical area — Test method and requirements (phase 2, step 2
[12] EN 14885, Chemical disinfectants and antiseptics — Application of European standards for chemical disinfectants and antiseptics
[13] ASTM E1052-11, Standard Test Method for Efficacy of Antimicrobial Agents Against Viruses in Suspension
[14] ASTM E1053-11, Standard Test Method to Assess Virucidal Activity of Chemicals Intended for Disinfection of Inanimate, Nonporous Environmental Surfaces
[15] ASTM E2111-05, Standard Quantitative Carrier Test Method to Evaluate the Bactericidal,
Fungicidal, Mycobactericidal and Sporicidal Potencies of Liquid Chemical Microbicides
[16] ASTM E2197-11, Standard Quantitative Disk Carrier Test Method for Determining the Bactericidal,
Virucidal, Fungicidal, Mycobactericidal and Sporicidal Activities of Liquid Chemical Germicides
[17] ASTM E2314-03, Standard Test Method for Determination of Effectiveness of Cleaning Processes for Reusable Medical Instruments Using a Microbiologic Method (Simulated Use Test)
[18] AOAC sporicidal test, Sporicidal Activity Test: Official Methods of Analysis, 15th Ed., Association of Official Analytical Chemists, Arlington VA, Method 966.04, 2002
Copyright In8ter0national Organization for Standardization
Order Number: 02223302
© ISO 2018 – All rights reserved
Provided by IHS Markit under license with ANSI
No reproduction or networking permitted without license from IHS
Sold to:CANTEL MEDICAL *DA [001612] - SMARTIN@MEDIVATORS.COM, Not for Resale,2018-12-18 15:39:13 UTC
ISO 15883-4:2018(E)
[19] AOAC International. Official Methods of Analysis of AOAC INTERNATIONAL. Chapter 6,
Nineteenth Edition, 2012
[20] DVV. Quantitative test for the evaluation of virucidal activity of chemical disinfectants on non-porous surfaces. Guideline of “Deutsche Vereinigung zur Bekämpfung der Viruskrankheiten e.V.” (DVV;
German Association for the Control of Virus Diseases). Bundesgesundheitsbl. 2015, 58, 493–504
[21] OECD Environment, Health and Safety Publications, Series on Testing and Assessment No. 187 and Series on Biocides No. 6, ENV/JM/MONO (2013)11, Guidance document on quantitative methods for evaluating the activity of microbicides used on hard non-porous surfaces.
[22] DGKH (German Society of Hospital Hygiene). Testing and evaluating the cleaning and disinfection efficacy of endoscope washer-disinfectors and disinfecting automats. Hyg Med. 1995, 20, 40-47 and correction Hyg Med. 2001, 26, 524
[23] Pineau L., Roques C., Lue J., Michel G. Automatic WD for flexible endoscopes — A new evaluation process, Endoscopy. 1997, 29, 372–377
[24] Orzechowski T.J.H., de Bruijn A.C.P., Wassenaar C. Validation of a cleaning test for flexible endoscopes. Central Service. 2003, 11 (3), 165–178
[25] Schrader G., Görisch G. The Limitations of Instrument Cleaning Based on Data Collected on vCJD-
Risks Posed by Medical Instrument. Hyg Med. 2003, 28, 306–309
[26] Edmunds L.M., Rawlinson A. The effect of cleaning on blood contamination in the dental surgery following periodontal procedures. Aust Dent J. 1998, 43 (5), 349–353
[27] Michels W. Evaluation of a quick test for examining cleaning efficiency of processed surgical and minimally invasive instruments. Hyg Med. 1997, 22, 173–184
[28] Michels W. Proof of drying within the channels of flexible endoscopes. Central Service. 2015,
23, 94–97
[29] Koller W., Lessky E. Evaluierung eines automatischen Verfahrens zur Reinigung und chemothermischen Desinfektion flexibler Endoskope. Hyg Med. 1989, 14, 24–30
[30] Health Technical Memorandum 01-01: Management and decontamination of surgical instruments (medical devices) used in acute care, Part D – Washer-disinfectors. Crown copyright 2016
[31] Hygienic and microbiological inspection of flexible endoscopes after reprocessing. Central Service.
2010, 18, 113–117
[32] Luu Duc D., Shum-Cheong-Sing J., Soule H., Fauconnier J., Marchetti B., Mallaret M.R., Lerroux N., Ducel G. and Calop J. Validation of a sampling method for the channels of a flexible endoscope which is experimentally contaminated. Pathol Biol (Paris). 1998 Jan, 46 (1), 34-38
[33] Chu N.S., McAllister D., Antonoplos P.A. Natural bioburden levels detected on flexible gastrointestinal endoscopes after clinical use and manual cleaning. Gastrointest Endosc. 1998. 48 (2), 137–142
[34] Vesley D., Melson J., Stanley P. Microbial bioburden in endoscope reprocessing and an in-use evaluation of the high-level disinfection capabilities of Cidex OPA. Gastroenterol Nurs. 1999. 22 (2), 63–68
[35] Alfa M.J., Michelle J.A., Degagné, P., Olson N. Worst-case soiling levels for patient-used flexible endoscopes before and after cleaning. Am J Infect Control. October 1999. 27 (5), 392-401
[36] Wehrl M., Kircheis U. Method for testing the cleaning efficacy of washer-disinfectors for flexible endoscopes. Central Service. 2011. 19, 357-361
Copyright International Org©anizIaStioOn fo2r S0ta1n8dar–dizAatiloln rights reserved
Provided by IHS Markit under license with ANSI
No reproduction or networking permitted without license from IHS
Order Number: 02223302 81
Sold to:CANTEL MEDICAL *DA [001612] - SMARTIN@MEDIVATORS.COM, Not for Resale,2018-12-18 15:39:13 UTC
ISO 15883-4:2018(E)
ICS 11.080.10
Price based on 81 pages
Copyright In©ternIaStioOnal2O0rg1an8iza–tionAfolrlSrtaingdhardtiszartioenserved Provided by IHS Markit under license with ANSI
No reproduction or networking permitted without license from IHS
Order Number: 02223302
Sold to:CANTEL MEDICAL *DA [001612] - SMARTIN@MEDIVATORS.COM, Not for Resale,2018-12-18 15:39:13 UTC
Список литературы:
INTERNATIONAL STANDARD ISO 15883-4
Рекомендуемые статьи
При эндоскопическом исследовании в случае бронхоэктазов в стадии ремиссии выявляется
частично диффузный бронхит I степени воспаления
Активируйте PUSH уведомления в браузер
Отключите PUSH уведомления в браузер
Содержание
Интернет магазин
Популярное
- О нас
- Правовые вопросы
- Политика
обработки персональных
данных EndoExpert.ru - Связаться с нами
- Стать партнером
© 2016-2022 EndoExpert.ru

Вы находитесь в разделе предназначенном только для специалистов (раздел для пациентов по ссылке). Пожалуйста, внимательно прочитайте полные условия использования и подтвердите, что Вы являетесь медицинским или фармацевтическим работником или студентом медицинского образовательного учреждения и подтверждаете своё понимание и согласие с тем, что применение рецептурных препаратов, обращение за той или иной медицинской услугой, равно как и ее выполнение, использование медицинских изделий, выбор метода профилактики, диагностики, лечения, медицинской реабилитации, равно как и их применение, возможны только после предварительной консультации со специалистом. Мы используем файлы cookie, чтобы предложить Вам лучший опыт взаимодействия. Файлы cookie позволяют адаптировать веб-сайты к вашим интересам и предпочтениям.
Я прочитал и настоящим принимаю вышеизложенное, хочу продолжить ознакомление с размещенной на данном сайте информацией для специалистов.











.jpg)
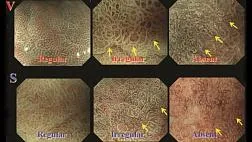


.png)















Комментарии