- Компании
- Takeda. О компании, буклеты, каталоги, контакты
- Olympus. О компании, буклеты, каталоги, контакты
- Boston Scientific. О компании, буклеты, каталоги, контакты
- Pentax. О компании, буклеты, каталоги, контакты
- Fujifilm & R-Farm. О компании, буклеты, каталоги, контакты
- Erbe. О компании, буклеты, каталоги, контакты
- Еще каталоги
- Мероприятия
- Информация
- Обучение
- Классификации
- Атлас
- Quiz
- Разделы
- Пациенту
QR-код этой страницы
Для продолжения изучения на мобильном устройстве ПРОСКАНИРУЙТЕ QR-код с помощью спец. программы или фотокамеры мобильного устройства
Документы и приказы: Седация пациентов в отделениях анестезиологии, реанимации и интенсивной терапии
| Авторы: | Потиевская В.И., Заболотских И.Б., Гридчик И.Е., Грицан А.И., Еременко А.А., Козлов И.А., Левит А.Л., Мазурок В.А., Молчанов И.В. |
Полный текст статьи:
МИНИСТЕРСТВО
ЗДРАВООХРАНЕНИЯ
РОССИЙСКОЙ ФЕДЕРАЦИИ
Методические рекомендации
СЕДАЦИЯ ПАЦИЕНТОВ В ОТДЕЛЕНИЯХ
АНЕСТЕЗИОЛОГИИ, РЕАНИМАЦИИ И ИНТЕНСИВНОЙ
ТЕРАПИИ
Год утверждения (частота пересмотра): 2023 (пересмотр каждые 3 года)
Профессиональные ассоциации:
Общероссийская общественная организация «Федерация анестезиологов и реаниматологов»
Утверждены
Президиумом Общероссийской общественной организации «Федерация анестезиологов и реаниматологов» 21 июня 2023 года
ОГЛАВЛЕНИЕ
Ключевые слова 3
Список сокращений 4
Термины и определения 4
Краткая информация 5
Классификация 6
Подходы к проведению седации 7
Выбор седативных препаратов 18
Критерии оценки качества медицинской помощи 29
Список литературы 30
Приложение А1. Состав рабочей группы 48
Приложение А2. Методология разработки клинических рекомендаций 50
Приложение А3. Связанные документы 53
Приложение Б1. Алгоритм седации. Порядок проведения седации в ОАРИТ 54
Приложение Б2. Алгоритм седации. Стратегия седации в ОАРИТ 55
Приложение В. Информация для пациента 56
Приложение Г. Ричмондская шкала седации (RASS) 57
Ключевые слова
• седация
• искусственная вентиляция легких
• отделения анестезиологии, реанимации и интенсивной терапии
• седативные препараты
• постгипоксическая энцефалопатия.
Список сокращений
ИА — ингаляционные анестетики
ИВЛ — искусственная вентиляция легких
НИВЛ - неинвазивная искусственная вентиляция легких
НКИ - новая коронавирусная инфекция
ОАРИТ — отделение анестезиологии, реанимации и интенсивной терапии
ОРДС — острый респираторный дистресс-синдром
ЭЭГ — электроэнцефалография
RASS — Ричмондская шкала ажитации - седации
BIS — биспектральный индекс
Термины и определения
Ажитация — возбуждение, сопровождающееся моторным или речевым
возбуждением, страхом и тревогой.
Анальгезия - снижение или полное устранение чувствительности к боли.
Анксиолизис - минимальная седация, устранение тревоги.
Процедурная седация - техника введения седативных средств вместе с анальгетиками или без них, которая позволяет пациенту переносить неприятные процедуры, без нарушения функции систем дыхания и кровообращения.
Посттравматическое стрессовое расстройство — психическое расстройство, развивающееся вследствие мощного психотравмирующего воздействия угрожающего или катастрофического характера, сопровождающееся экстремальным стрессом.
Седация — контролируемый уровень медикаментозной депрессии сознания, при котором сохранены защитные рефлексы, обеспечивается адекватное дыхание и есть ответ на физические стимулы или вербальные команды [1]. Также седацию определяют, как комплекс медикаментозных и немедикаментозных средств, предназначенный обеспечить физический и психический комфорт пациента и облегчить уход за пациентом в отделении анестезиологии, реанимации и интенсивной терапии (ОАРИТ) [2].
Краткая информация
Многие пациенты в отделении реанимации и интенсивной терапии нуждаются в проведении адекватной седации в силу различных причин, среди которых необходимость выполнения инвазивных процедур, нарушение циркадных ритмов сна и бодрствования, тяжесть общего состояния, необходимость респираторной поддержки [3,4].
Основными причинами ажитации (возбуждения) являются боль, делирий, гипоксемия, гипогликемия, гипотензия, алкогольный или другой абстинентный синдром.
Возбуждение способствует асинхронии с аппаратом ИВЛ, повышенному потреблению кислорода, увеличению продукции углекислоты и лактата, респираторному и метаболическому ацидозу [4].
Седация также может быть причиной неблагоприятных клинических исходов, поэтому она должна использоваться только тогда, когда это действительно необходимо, быть настолько минимальной, насколько это возможно и ежедневно прерываться, если к этому нет противопоказаний [5].
Избыточная седация может привести к неоправданно пролонгированной ИВЛ и связанным с ней осложнениям, в том числе пневмонии. Длительная ИВЛ, в свою очередь, обусловливает увеличение времени пребывания в ОАРИТ, ухудшение прогноза, повышение риска летального исхода и возрастание затрат на лечение пациентов.
Принципы седации в ОАРИТ
- обеспечение легкой степени седации;
- ежедневные перерывы седации;
- использование протоколов и алгоритмов седации [6].
Глубокая седация может вызвать когнитивные нарушения, поэтому поддержание легкой степени седации является наиболее безопасным для пациента [7].
Задачи седативной терапии пациентов в ОАРИТ:
- уменьшение возбуждения и боли;
- снижение количества дней на ИВЛ и частоты трахеостомии;
- уменьшение времени пребывания в ОАРИТ;
- снижение частоты когнитивных расстройств;
- уменьшение потребления кислорода и стрессового ответа организма;
- предупреждение осложнений со стороны сердечно-сосудистой системы, легких, печени и почек;
- уменьшение десинхронизации с аппаратом ИВЛ и связанных с ИВЛ осложнений, в том числе развития вентилятор-ассоциированной пневмонии;
- уменьшение частоты развития депрессии и посттравматических стрессовых расстройств;
- уменьшение количества спонтанной экстубации;
- уменьшение частоты встречаемости делирия и/или более успешное лечение делирия [2, 8].
В настоящих рекомендациях изложены вопросы седации в ОАРИТ для взрослых пациентов. Диагностика и лечение делирия в данных рекомендациях не рассматриваются. Классификация
Седация различается по уровню (глубине) [9]:
- минимальная седация (анксиолизис), или легкая (поверхностная) седация: пациент находится в состоянии бодрствования, контактирует с врачом, но познавательная функция и координация могут быть нарушены;
- умеренная седация: депрессия сознания, при которой пациенты реагируют на словесный или легкий тактильный стимул, способны к сотрудничеству, адекватное спонтанное дыхание (не требуется поддержки проходимости дыхательных путей) и функция сердечно-сосудистой системы сохранены;
- глубокая седация: пациенты не могут быть легко пробуждены, но реагируют на повторный или болезненный стимул, может потребоваться поддержка проходимости дыхательных путей, спонтанное дыхание может быть нарушено, функция сердечно¬сосудистой системы сохранена.
В то же время разграничение уровня седации является условным и до сих пор нет точного определения легкой седации, которая по современным представлениям является оптимальной. Было принято считать легкой седацию с показателями по шкале RASS от -2 до +1 и при способности пациента открывать глаза не менее, чем на 10 с [10]. Однако этот уровень седации может превышать минимально необходимый. Оценка уровня седации при ее ежедневном прерывании также не может отражать объективную картину, так как снижение уровня седации происходит на определенном отрезке времени, а не в течение всего дня.
Седация также делится на фармакологическую, осуществляемую с помощью лекарственных препаратов, и нефармакологическую, при которой проводятся мероприятия и создаются условия более комфортного пребывания пациента.
Подходы к проведению седации
У пациентов в ОАРИТ, находящихся на ИВЛ, возможно возникновение тревоги, возбуждения, страха.
Предрасполагает к развитию возбуждения наличие в анамнезе алкогольной или наркотической зависимости, органических заболеваний головного мозга, артериальной гипертензии, особенно плохо контролируемой, общее тяжелое состояние пациента, а также пожилой возраст.
Большое значение имеют своевременная идентификация и устранение основных причин возбуждения, таких как боль, делирий, гипоксемия, гипогликемия, гипотензия, алкогольный или другой абстинентный синдром.
Результаты физикального обследования зависят от конкретного заболевания и тяжести состояния пациента. Необходимо обратить внимание на наличие признаков гипоксемии (цианоз) и нарушений периферического кровообращения, одышки, тахикардии, дыхательной и сердечной недостаточности, симптомов раздражения брюшины, олигурии и анурии, которые могут быть причинами возникновения возбуждения у пациентов в ОАРИТ.
Необходимо отметить, что в рекомендации Critical Care Society (2018) вошли такие разделы, как мобилизация (активизация) пациентов и сон, при этом малая подвижность и нарушения сна рассматриваются как отдельные расстройства, предрасполагающие к возникновению делирия. [11]
Стратегия оптимальной седации включает обезболивание (в первую очередь), легкую седацию, мультимодальную седацию и анальгезию, раннюю активизацию и профилактику делирия фармакологическими и нефармакологическими методами [12, 13].
Рекомендация 1. Пациентам ОАРИТ рекомендуется проводить в первую очередь анальгезию, а затем седацию [14, 15]. Уровень достоверности доказательств 1, уровень убедительности рекомендаций А.
Комментарий. Седацию возбужденного пациента в критическом состоянии можно начинать только после обеспечения адекватной анальгезии на фоне лечения обратимых физиологических причин (гипоксемии, гипогликемии, гипотензии, алкогольной или наркотической абстиненции). При этом предупреждение боли эффективнее, чем лечение уже имеющейся боли. Боль, страх и возбуждение могут иметь неблагоприятные психологические эффекты и вредные последствия [16]. Боль ухудшает функции дыхания и кровообращения, повышает частоту легочных осложнений и эндокринно-метаболических реакций. Страх может привести к отказу от ухода, прекращению сотрудничества с персоналом ОАРИТ, росту агрессивности. Анальгезия и седация приводят к уменьшению эндокринно-метаболической реакции на стресс, повышают соотношение «доставка- потребление кислорода», снижают частоту послеоперационных осложнений и летальность. Важно также исключить наличие обструкции верхних дыхательных путей, а у пациентов на ИВЛ — однолегочной вентиляции.
Недостаточное обезболивание может вызвать стресс, нарушения сна, когнитивную дисфункцию, возбуждение и даже приводить к развитию делирия. Добавление аналгоседации к протоколу седации способствует сокращению назначения седативных препаратов и снижает риск развития делирия [17, 18].
При этом положительные свойства были обнаружены у клонидина, который обладает и седативным, и анальгетическим эффектами [19].
Использование легкой седации совместно с анальгезией возможно даже при таких состояниях, как тяжелые ожоги, но применение менее глубокой седации не влияло на продолжительность ИВЛ у этой категории пациентов [20].
Рекомендации по лечению боли подробно изложены в клинических рекомендациях по послеоперационному обезболиванию ФАР [21].
Рекомендация 2. У всех пациентов ОАРИТ рекомендуется перед применением седативных средств предпринять попытки снижения беспокойства и возбуждения с помощью нефармакологической седации [16]. Уровень достоверности доказательств 2, уровень убедительности рекомендаций B.
Рекомендация 3. У всех пациентов ОАРИТ рекомендуется предотвращать нарушения сна, используя нефармакологические методы (ограничение шума, обследований в ночное время) [22-25]. Уровень достоверности доказательств 1, уровень убедительности рекомендаций A.
Комментарий. Нефармакологические методы включают следующие мероприятия:
- удаление ненужных инфузионных линий и трубок;
- прекращение или минимизацию фиксации пациента;
- обеспечение нормального цикла сна (обеспечить естественный сон ночью, соблюдать режим сна, не будить ранее чем через 90 мин от начала седации, проводить регулярные перерывы в уходе (60-90 мин), массаж спины 5-10 мин, создать спокойное окружение (в том числе посредством привлечения близких и родственников пациента), не включать свет, использовать естественные маркеры для сна — окно или регулировка свет/темнота);
- если пациент пользуется слуховым аппаратом и/или очками, целесообразно их применение в ОАРИТ для лучшего контакта персонала с пациентом.
Рекомендация 4. Пациентам ОАРИТ рекомендуется проводить минимально необходимую седацию только при наличии показаний и при недостаточной эффективности методов нефармакологической седации [26]. Уровень достоверности доказательств 2, уровень убедительности рекомендаций B.
Комментарий. Исследование NONSEDA не выявило различий 90-дневной летальности и количеству дней в ОРИТ без ИВЛ между группами пациентов с легкой седацией и без седации [27].
Рекомендация 5. Пациентам ОАРИТ рекомендуется проводить легкую седацию, если нет показаний к глубокой седации [28]. Уровень достоверности доказательств 1, уровень убедительности рекомендаций А.
Комментарий. Легкая седация связана с меньшей продолжительностью ИВЛ и пребывания в ОАРИТ и стационаре, снижением частоты трахеостомий, делирия, депрессии и самоэкстубации [29 - 31]. Напротив, глубокая седация приводит к худшим исходам для пациентов ОАРИТ, увеличивая 90-дневную летальность [32].
Рекомендация 6. Всем пациентам ОАРИТ рекомендуется регулярно оценивать уровень седации с помощью Ричмондской шкалы ажитации - седации - RASS [33]. Уровень достоверности доказательств 1, уровень убедительности рекомендаций А.
Комментарий. Оптимальной шкалой для оценки седации является RASS (Ричмондская шкала ажитации-седации) — наиболее информативная и надежная шкала для оценки качества и глубины седации у пациентов в ОАРИТ [34] - приложение Г, которая достаточно проста в использовании и отражает, как уровни седации, так и возбуждения пациентов в ОАРИТ [35, 36].
Шкала RASS валидирована для пациентов на ИВЛ и без ИВЛ, для хирургических и нехирургических, седированных и не седированных пациентов в ОАРИТ. Использование шкалы RASS позволяет уменьшить дозы седативных препаратов и продолжительность ИВЛ [35-38]
Рекомендация 7. У пациентов ОАРИТ рекомендуется проводить ежедневные прерывания седации [8, 39, 40]. Уровень достоверности доказательств 1, уровень убедительности рекомендаций A.
Комментарий. Постоянная седативная терапия ассоциирована с большей
длительностью ИВЛ, большей продолжительностью пребывания в ОАРИТ и стационаре.
Кроме того, непрерывная седация затрудняет оценку когнитивных и психических функций пациента, нарушает активность головного мозга в течение длительного времени после ее прекращения и увеличивает смертность в течение последующих 6 месяцев. Впервые методика ежедневного кратковременного прерывания седации была предложена J.P.Kress et al. (2000). Было показано, что прерывистая седация сокращает время ИВЛ в среднем на 2 дня и время пребывания в ОАРИТ на 3,5 дня [41]. В последующем эти данные были подтверждены двумя рандомизированными исследованиями - Awakening and Breathing Controlled Trial (2008) («проснись и дыши») [40] и No Sedation in Intensive Care Unit Patients (2010) [8, 42, 43].
Ежедневные прерывания седации не ухудшают психологическое состояние, а, напротив, ассоциированы с уменьшением частоты развития посттравматического стрессового расстройства [44 - 46].
Рекомендация 8. Рекомендуется включать перерывы в седации в протокол по отлучению пациентов от ИВЛ [47 - 49]. Уровень достоверности доказательств 3, уровень убедительности рекомендаций B.
Комментарий. В одном исследовании прерывания седации были совмещены с попытками спонтанного дыхания [47], а в другом предлагалось проводить оценку неврологического статуса во время перерывов в инфузии седативных препаратов [48, 49].
У пациентов с НКИ COVID-19 ежедневные перерывы седации могут проводиться, только если есть уверенность, что состояние не ухудшится и при необходимости будет обеспечена защита пациента от негативных последствий [50].
Рекомендация 9. Не рекомендуется прерывать седацию пациентам с внутричерепной гипертензией [51, 52]. Уровень достоверности доказательств 2, уровень убедительности рекомендаций А.
Комментарий. В рекомендациях Celis-Rodriguez E, et al. [53] указано, что пациентам с внутричерепной гипертензией не показаны ежедневные прерывания седации [49]. Повышение внутричерепного давления и снижение церебрального перфузионного давления могут отрицательно повлиять на уровень кровоснабжения и оксигенации головного мозга и состояние пациента [51]. В проспективном обсервационном исследовании Helbok R. et al (2012) [52] показано, что ежедневные прерывания седации у пациентов с повреждением головного мозга в остром периоде сопровождаются повышением внутричерепного давления, возбуждением, десатурацией и неблагоприятными метаболическими изменениями
головного мозга.
Рекомендация 19. Пациентам с постгипоксической энцефалопатией в остром периоде не рекомендуется прерывание седации [54 - 56]. Уровень достоверности доказательств 2, уровень убедительности рекомендаций С.
Комментарий. В остром периоде постгипоксической энцефалопатии показана терапия, направленная на снижение энергетических потребностей мозга. Недостаточная аналгоседация у этих пациентов приводит к повышению внутричерепного давления, дисциркуляторным изменениям, гипоксии, нарушению текучих свойств крови, жировой эмболии, синдрому диссеминированного внутрисосудистого свертывания, отеку-набуханию мозга, истощению системы эндорфинов, диэнцефальным кризам. Терапия первых 3 ч постгипоксического периода для всех пациентов, перенесших терминальное состояние, идентична (дозы и схема лечения приводятся для взрослого со средней массой тела 70-80 кг) и включает введение препаратов, снижающих энергетические потребности мозга: производные бензодиазепинов или пропофол. Согласно американскому руководству по ведению пациентов с постгипоксической энцефалопатией вследствие травматического повреждения головного мозга, рекомендовано назначение центральных агонистов альфа-2 рецепторов (дексмедетомидин) под контролем артериального давления.
Рекомендация 7. У пациентов ОАРИТ не рекомендуется рутинное использование инструментальных методов оценки уровня седации (электроэнцефалография (ЭЭГ), биспектральный индекс (BIS) [57, 58]. Уровень достоверности доказательств 1, уровень убедительности рекомендаций В.
Комментарий. В настоящее время нет убедительных доказательств о преимуществах BIS -мониторинга в ОАРИТ. В то же время у пациентов с повреждением головного мозга может быть целесообразно использование инструментальных методов мониторинга, в том числе для оценки функционального состояния церебрального кровотока. Применение оценочных шкал в сочетании с таким мониторингом позволяет снизить дозы седативных препаратов [59].
Рекомендация 9. Пациентам ОАРИТ с тяжелой дыхательной недостаточностью, находящихся на ИВЛ в условиях миорелаксации, рекомендуется проводить глубокую седацию [60]. Уровень достоверности доказательств 2, уровень убедительности рекомендаций B.
Комментарий. При глубокой седации и нейромышечной блокаде инструментальные методы оценки имеют преимущества по сравнению со шкалами [61- 63]. При глубокой седации шкалы будут показывать максимальное угнетение сознания (-5 по шкале RASS и 1 по шкале SAS), а при нейромышечной блокаде невозможно оценить двигательные реакции пациента. В то же время не получено достоверных доказательств о преимуществах BIS- мониторинга и влиянии метода оценки седации на длительность ИВЛ и время пребывания в ОАРИТ, исходы заболевания или затраты на лечение [63].
Рекомендация 10. Глубокий уровень седации рекомендуется пациентам с постгипоксической энцефалопатией, рефрактерным эпилептическим статусом, пароксизмальной эпилептической активностью, гипотермии и рефрактерной внутричерепной гипертензии [59, 64-66]. Уровень достоверности доказательств 1, уровень убедительности рекомендаций B.
Комментарий. Агрессивное лечение с использованием анестетиков и глубокой седации рекомендуется пациентам с рефрактерным эпилептическим статусом вследствие необходимости подавить судорожную активность, которая может вызвать повреждение центральной нервной системы. При этом повышается активность Х-метил-! Хаспартат (NMDA) и рецепторов а-амино-3-гидрокси-5-метил-4-изоксазопропионовой кислоты (AMPA, что приводит к активации перекисного окисления липидов и повреждению фосфолипидного слоя клеточных мембран активными формами кислорода [67].
По данным другого исследования глубокая седация при эпилептическом статусе ассоциируется с плохим отдаленным прогнозом [68]. Это обусловлено побочными эффектами продленной глубокой седации, такими, как артериальная гипотензия, требующая применения вазопрессоров, иммуносупрессия, парез желудочно-кишечного тракта и дыхательная недостаточность [69].
В случае внутричерепной гипертензии целью является оптимизация перфузии и церебральной оксигенации, а также борьба с судорожным синдромом, нейровегетативными нарушениями и предупреждение новых эпизодов гипертензии.
Рекомендация 11. Пациентам с ОРДС рекомендуется проводить легкую седацию, или эпизодически умеренную седацию для преодоления асинхронии с аппаратом ИВЛ [42, 70]. Уровень достоверности доказательств 1, уровень убедительности рекомендаций B.
Комментарий. Современные подходы к седации пациентов с ОРДС включают использование легкой седации в первые 48 часов пребывания в ОАРИТ, адекватное обезболивание при минимальной седации или ее отсутствии, применение дексмедетомидина и атипичных антипсихотиков для снятия возбуждения после экстубации, комплексный подход к седации [71].
Для преодоления асинхронии с аппаратом ИВЛ или для обеспечения параметров протективной вентиляции может потребоваться глубокая седация [72].
Глубокая седация и нейромышечная блокада могут приводить к атрофии диафрагмы и неоправданно пролонгировать ИВЛ и пребывание в ОАРИТ [73].
Рекомендация 12. Рекомендуется проводить глубокую седацию пациентам на ИВЛ с новой коронавирусной инфекцией COVID-19 и тяжелым ОРДС, требующим применения миорелаксантов [74]. Уровень достоверности доказательств 3, уровень убедительности рекомендаций С.
Комментарий. Высокая распространенность ОРДС среди пациентов с тяжелым течением новой коронавирусной инфекций (НКИ) COVID-19 привела к необходимости использовать седацию у пациентов на ИВЛ. Седация облегчает синхронизацию с аппаратом ИВЛ, особенно у пациентов в прон-позиции, предупреждает эпизоды самоэкстубации и является необходимой при использовании миорелаксантов [75].
Есть сведения о том, что пациентам с НКИ COVID-19 требуются более высокие дозы седативных препаратов и анальгетиков по сравнению с пациентами с ОРДС другой этиологии, что повышает риск развития побочных эффектов седативной терапии [74]. Кроме того, часто требуется применение нескольких групп препаратов и продолжительность пребывания на ИВЛ увеличена по сравнению с другими больными в среднем c 7 до 12 дней. При этом особенно актуальным становится учет взаимодействий седативных препаратов с другими лекарственными средствами, используемыми для лечения новой коронавирусной инфекции (например, удлинение интервала QT на ЭКГ). Необходимо также принимать во внимание частое развитие острой почечной недостаточности у этой категории пациентов, что требует отказа от нефротоксичных комбинаций и коррекции доз препаратов [75].
Наиболее часто по данным литературы использовались мидазолам и пропофол, в том числе в сочетании с опиоидами, применяемыми для анальгезии [76].
Использование пропофола может быть ограничено при артериальной гипотензии или при необходимости длительного введения высоких доз препарата, что потенциально может привести к синдрому инфузии пропофола. Для седации пациентов с НКИ COVID-19 может также применяться дексмедетомидин. Ограничениями к его использованию являются брадикардия и необходимость более глубокой седации с введением миорелаксантов [53, 75].
Рекомендация 13. У пациентов на ИВЛ рекомендуется поддерживать легкую седацию с момента поступления пациента в ОАРИТ [77, 78]. Уровень достоверности доказательств 1, уровень убедительности рекомендаций A.
Комментарий. Глубокая седация в первые 48 часов увеличивает летальность и время пребывания в ОАРИТ [79].
Рекомендация 14. У всех пациентов в ОАРИТ рекомендуется регулярно проводить переоценку глубины и качества седации [80, 81]. Уровень достоверности доказательств 1, уровень убедительности рекомендаций А.
Комментарий. Раннее применение глубокой седации при отсутствии показаний может ухудшить исход заболевания у пациентов, находящихся на ИВЛ [82]. В то же время современные исследования доказывают, что поддержание минимальной седации у пациентов с тяжелыми нарушениями функции дыхания, в том числе с ОРДС, позволяют достичь более ранней активизации, отлучения от аппарата ИВЛ, снизить риск возникновения делирия и ускорить выздоровление [83]. Во всех перечисленных случаях состояние пациентов и показания к глубокой седации должны подвергаться периодической переоценке.
Рекомендация 15. Для улучшения проведения седации в ОАРИТ рекомендуется использовать протоколы и алгоритмы седации [83]. Уровень достоверности доказательств 1, уровень убедительности рекомендаций B. [12, 84].
Комментарий. Кохрейновский обзор 2018 г, включавший 3323 пациента, продемонстрировал, что использование протоколов седации позволяет сократить пребывание в стационаре более, чем на 3 суток. Однако не было получено убедительных данных о влиянии использования протоколов седации на длительность ИВЛ, длительность пребывания в ОАРИТ и летальность [84].
Для пациентов ОАРИТ используется стратегия ABCDEF: A - оценка, профилактика и лечение боли, B - тест со спонтанным пробуждением и тест со спонтанным дыханием, C - выбор анальгезии и седации, D - оценка, профилактика и лечение делирия, E - ранняя мобилизация и физические упражнения, F - привлечение родственников [32]. В протокол ведения пациентов с ОРДС к алгоритму ABCDEF добавляется R - respiratory drive, т. е. преодоление нарушений вентиляции [70].
Исследование, объединившее 15000 пациентов из США и Пуэрто-Рико, показало эффективность протокола ABCDEF [12]. У пациентов реже развивались кома, делирий, потребность в физической фиксации, было меньше повторных переводов в ОАРИТ, больные чаще выписывались домой. Однако полностью протокол соблюдался только у 8% пациентов.
Другая стратегия, подразумевающая пациент-ориентированное лечение и комфорт, называется eCASH (комфорт начиная с раннего пребывания в ОАРИТ с использованием анальгезии, минимальной седации и максимально гуманного лечения), включает обезболивание в первую очередь, минимальную седацию или отсутствие седации, коммуникацию, уменьшение шума для обеспечения полноценного сна, раннюю активизацию и привлечение членов семьи [13].
По данным ретроспективного анализа карт 2417 пациентов было обнаружено, что выполнение рекомендаций по седации пациентов приводило к сокращению времени ИВЛ и пребывания в стационаре [85].
Есть отдельные категории пациентов, для которых необходимы специальные подходы к седации. Например, неврологические пациенты в ОАРИТ имеют особенности ведения ИВЛ и отлучения от ИВЛ, ограничения ранней активизации, а также выбора антикоагулянтной терапии, которые должны быть учтены в протоколах седации [86]
В настоящее время нет единого протокола седации для пациентов в ОАРИТ, поэтому для их создания целесообразно привлекать мультидисциплинарную команду специалистов [79].
Рекомендация 16. У пациентов ОАРИТ во время прерывания седации рекомендуется оценивать необходимость физического стеснения [87]. Уровень достоверности доказательств 3, уровень убедительности рекомендаций С.
Комментарий. Нет убедительных доказательств преимуществ физического стеснения пациентов в ОАРИТ. Существуют описательные исследования низкого качества. По данным этих исследований парадоксальным образом при физическом стеснении пациентов увеличивается количество нежелательных эффектов, которые должны были быть с ее помощью предотвращены: незапланированная экстубация и частые реинтубация, непреднамеренное удаление линий и устройств, более длительное пребывание в ОРИТ, повышенное возбуждение, увеличение потребления бензодиазепинов, опиоидов и других седативных препаратов, повышенный риск делирия и дезориентации [88, 89].
В одном из исследований было показано, что около 72% пациентов в ОАРИТ были фиксированы профилактически. Доказывается необходимость минимизации физического стеснения и обсуждения каждого случая междисциплинарной командой [90].
Есть также рекомендации по использованию физического стеснения, созданные в Китае на основании дельфийского метода опроса экспертов. Сильной рекомендацией является создание обучающих программ для медицинского персонала с целью минимизации использования физического стеснения в условиях ОАРИТ [91].
Рекомендация 17. Рекомендуется ранняя активизация пациентов в ОАРИТ, находящихся на ИВЛ [92 - 101]. Уровень достоверности доказательств 2, уровень убедительности рекомендаций B.
Комментарий. В 6 РКИ показано, что ранняя активизация увеличивает мышечную силу пациентов к моменту перевода из ОАРИТ [1 - 3, 9, 10, 16]. В ряде РКИ было также выявлено уменьшение времени ИВЛ у пациентов, которым проводились реабилитационные мероприятия в ОАРИТ [1, 2, 4, 8, 14]. В то же время не было получено достоверных результатов по влиянию активизации и реабилитации пациентов на качество жизни, госпитальную летальность и показатели оценки физического состояния. По мнению экспертов все же преимущества ранней активизации и реабилитации преобладают над возможными отрицательными последствиями, поэтому рекомендуется проводить данные мероприятия [5].
Выбор седативных препаратов
Седативные препараты — это медикаментозные средства, которые успокаивают пациента, уменьшают возбуждение и обеспечивают сон [1] (таблица 1).
Отрицательные побочные эффекты седативных препаратов в ОАРИТ:
- развитие толерантности к препаратам;
- избыточный седативный эффект;
- нарушение перистальтики желудочно-кишечного тракта;
- появление симптомов отмены;
- когнитивный дефицит.
Выбор седативного препарата, глубина седации и факторы, связанные с особенностями конкретного пациента, играют ключевую роль в исходе заболевания [102].
Дексмедетомидин. Является селективным агонистом а2-адренорецепторов, но не обладает селективностью к А, В и С подтипам а2-адренорецепторов. Препарат обладает седативным, обезболивающим и симпатолитическим эффектами, но без противосудорожного действия, позволяет снизить потребность в опиоидах. Седация при назначении дексмедетомидина имеет определенные особенности [103]. Пациенты, получающие инфузию дексмедетомидина, легко просыпаются и способны к взаимодействию с персоналом, а признаки угнетения дыхания выражены минимально. а2-Агонисты вызывают активацию а2А- адренорецепторов в голубом пятне (locus coeruleus) и стволе мозга. Это, в свою очередь, приводит к ингибированию выброса норадреналина и гиперполяризации возбудимых нейронов, что вызывает седативный эффект [104]. Поэтому седация, вызванная дексмедетомидином, близка к естественному сну [105].
Дексмедетомидин легко проникает через гематоэнцефалический барьер и обладает анальгетическим эффектом, особенно в сочетании с низкими дозами опиоидов или местных анестетиков [106, 107].
Симпатолитический эффект дексмедетомидина связан с уменьшением высвобождения норадреналина из симпатических нервных окончаний [108], а седативный эффект опосредован снижением возбуждения в голубом пятне, основном центре норадренергической иннервации центральной нервной системы [109].
Дексмедетомидин потенцирует анальгетический эффект опиатов [110]. У взрослых на ИВЛ с факторами риска развития делирия использование для седации дексмедетомидина снижает выраженность делирия в сравнении с бензодиазепинами и пропофолом. В сравнении с пропофолом дексмедетомидин уменьшает частоту когнитивных расстройств в 1,6 раза [107, 111]. Кроме того, дексмедетомидин сокращает время пребывания на ИВЛ и продолжительность пребывания в ОАРИТ пациентов с делирием по сравнению с пациентами, для лечения которых применялся галоперидол [112]. Внутривенное введение дексмедетомидина обеспечивает эффективную седацию у пациентов на ИВЛ в ОАРИТ, седацию во время оперативных вмешательств и процедурную седацию [108, 113]. Обычно инфузия дексмедетомидина переносится хорошо и приводит к уменьшению потребности во внутривенном введении пропофола и мидазолама и снижает необходимость назначения опиатов.
Дексмедетомидин не вызывает депрессии дыхания. Препарат может применяться для седации самостоятельно дышащих неинтубированных пациентов и пациентов, которым проводят неинвазивную масочную вентиляцию легких. После прекращения введения дексмедетомидин не оказывает каких-либо остаточных влияний на систему дыхания
При использовании дексмедетомидина могут возникать гипотензия и брадикардия, но они проходят обычно самостоятельно, без дополнительного лечения. При седации дексмедетомидином возникает также побочный эффект в виде расслабления мышц ротоглотки.
Клиническая фармакология лекарственных средств
Таблица 1.
Препарат Время наступ-ления действи я Время полувы-ведения Активные метаболиты Нагрузочная доза, в/в Поддерживающ ая доза, в/в Побочные явления
Дексмеде-томидин 5-10
мин 1,8-3,1 ч Нет 1 мкг/кг в
течение 10 мин. Не назначают
при нестабильной гемодинамике 0,2-0,7 мкг/(кг*ч), при нормальной переносимости можно повысить до 1,5 мкг/(кг*ч) Брадикардия, гипотензия;
гипертензия при
нагрузочной дозе;
потеря рефлексов
дыхательных путей
Пропофол 1-2 мин Кратко-временное применение 3-12 ч,
длительное применение 50±18,6 ч Нет 5 мкг/(кг*мин) в течение 5 мин. Вводят только пациентам, у
которых маловероятная гипертензия 5-50 мкг/(кг*мин) Угнетение дыхания. Боль при инъекции в периферические вены, гипотензия, гипертриглицеридеми я, панкреатит,
аллергические реакции, инфузионный синдром, связанный с пропофолом; после
глубокой седации
пропофолом пробуждение гораздо более длительное, чем после легкой седации
Мидазолам 2-5 мин 3-11 ч Есть. Продлевают седацию, особенно у
пациентов с
почечной недостаточнос тью 0,01-0,05 мг/кг в течение
нескольких минут 0,02-0,1 мг/(кг*ч) Угнетение дыхания,
гипотензия
Ингаляционные анестетики Несколь ко минут 4-7 ч Нет Нет Нет Гипотензия, дозозависимое угнетение дыхания,
брадикардия, тахикардия
Изофлуран Трифторацета т 3 мл/ч 2-7 мл/ч
Севофлуран Гексафторизо пропанол 5 мл/ч 4-10 мл/ч
Препарат противопоказан при:
- гиперчувствительности к компонентам препарата;
- атриовентрикулярной блокаде П-Ш степени (при отсутствии искусственного водителя ритма);
- неконтролируемой артериальной гипотензии;
- острой цереброваскулярной патологии;
- у детей до 18 лет.
Пациенты на ИВЛ могут быть переведены на инфузию дексмедетомидина с начальной скоростью 0,7 мкг/(кг*ч) с последующей постепенной коррекцией дозы в пределах 0,2-1,4 мкг/(кгхч) с целью достижения необходимой глубины седации. Седация наступает в течение 5-10 мин, пик наблюдается через 1 ч после начала в/в инфузии дексмедетомидина, длительность действия препарата после окончания инфузии составляет 30 мин. После коррекции скорости введения препарата необходимая глубина седации может не достигаться в течение 1 ч. При этом не рекомендуется превышать максимальную дозу 1,4 мкг/(кгхч).
Для ослабленных пациентов начальная скорость инфузии дексмедетомидина может быть снижена до минимальных значений. У пожилых пациентов не требуется коррекции дозы.
Если нужно ускорить начало действия препарата, например, при выраженном возбуждении, рекомендовано проводить нагрузочную инфузию в дозе 0,5-1,0 мкг/кг массы тела в течение 20 мин, т.е. начальную инфузию 1,5-3 мкг/(кг*ч) в течение 20 мин. После нагрузочной дозы скорость введения препарата снижается до 0,4 мкг/(кг*ч), в дальнейшем скорость инфузии можно корригировать.
Пациенты, у которых адекватный седативный эффект не достигнут на максимальной дозе препарата, должны быть переведены на альтернативное седативное средство. Введение насыщающей дозы препарата не рекомендуется, так как при этом повышается частота побочных реакций. До наступления клинического эффекта дексмедетомидина допускается введение пропофола или мидазолама. Опыт применения дексмедетомидина в течение более 14 дней отсутствует, при применении препарата более 14 дней необходимо регулярно оценивать состояние пациента.
Успешное применение дексмедетомидина в условиях ОАРИТ в России [114, 115] позволяет рекомендовать препарат в качестве одного из основных седативных средств как для пациентов на пролонгированной ИВЛ, так и на самостоятельном дыхании.
К агонистам а2-адренорецепторов относится также клонидин, который обладает влиянием на ai-адренорецепторы, оказывает анальгетическое и седативное действие, при этом имеет значительно более низкую стоимость. Существует ряд исследований, описывающих успешное применение клонидина в ОАРИТ, в том числе при длительной седации и отлучении от аппарата ИВЛ [116 - 118]. Однако в российской инструкции к препарату клонидин в показаниях к применению седация отсутствует, в связи с чем клонидин не был включен в данные клинические рекомендации.
Пропофол. Короткодействующий гипнотик. Механизм действия обусловлен воздействием на различные рецепторы центральной нервной системы, в том числе рецепторы Y-аминомасляной кислоты, глицина, никотиновой кислоты и М1-мускариновые рецепторы. Препарат обладает седативным, снотворным, амнестическим, противорвотным и противосудорожным действием, но лишен обезболивающего эффекта [51]. Пропофол хорошо растворяется в липидах и проникает через гематоэнцефалический барьер, что обеспечивает быстрое наступление седативного эффекта. При этом печеночный и внепеченочный клиренс пропофола высок, что обусловливает быстрое прекращение действия препарата. В связи с этим применение пропофола может быть рекомендовано для пациентов, которым требуется частое пробуждение для неврологической оценки или при дневном прерывании седации [119]. При длительном применении пропофола может произойти насыщение периферических тканей, что приведет к более длительному действию и более медленному выходу из седации [120]. Так же, как и производные бензодиазепинов, пропофол вызывает угнетение дыхания и гипотензию, особенно у пациентов с уже имеющейся дыхательной недостаточностью или гемодинамической нестабильностью. Эти эффекты потенцируются одновременным назначением других седативных средств или опиоидов.
Доза введения пропофола в ОАРИТ составляет 0,3-4,0 мг/(кг*ч) и не должна превышать 4 мг/(кг*ч). Для пожилых пациентов скорость инфузии препарата должна быть снижена. Через 3 дня введения пропофола необходимо проверить уровень липидов крови. Длительность седации пропофолом не должна превышать 7 дней.
К побочным эффектам пропофола относятся гипертриглицеридемия, острый панкреатит и миоклонус [121 - 125]. Пропофол может также вызывать аллергические
реакции у пациентов с аллергией на яичный лецитин и соевое масло (так как растворен в 10% эмульсии липидов, содержащей эти вещества). В 1% случаев возможно возникновение синдрома инфузии пропофола. Степень тяжести синдрома может существенно различаться. Основными проявлениями являются метаболический ацидоз, гипертриглицеридемия, гипотензия, аритмии. В более тяжелых случаях развивается острая почечная недостаточность, гиперкалиемия, рабдомиолиз и печеночная недостаточность [120, 121, 126, 127]. Причиной развития инфузионного синдрома является нарушение метаболизма жирных кислот и углеводов и накопление промежуточных продуктов метаболизма пропофола. Как правило, синдром инфузии пропофола возникает при использовании высоких доз препарата, но описан и при инфузии низких доз [128 - 130]. Распознавание синдрома инфузии имеет важное значение, так как летальность при его развитии остается высокой (до 33%) [131]. Лечение пациентов с синдромом инфузии пропофола в основном симптоматическое.
Бензодиазепины. Механизм действия бензодиазепинов основан на взаимодействии с рецепторами Y—аминомасляной кислоты в головном мозге. Препараты обладают седативным, амнестическим, снотворным и противосудорожным эффектами, но не имеют обезболивающего действия. При этом мидазолам обладает более выраженным эффектом, чем диазепам. Отмечается повышенная чувствительность к бензодиазепинам у пожилых [132]. Бензодиазепины могут вызывать угнетение дыхания, а также артериальную гипотензию, особенно в сочетании с опиоидами [133]. При длительном применении развивается толерантность к препаратам данной фармакологической группы.
Все бензодиазепины метаболизируются в печени, поэтому их выведение замедлено у пациентов с печеночной недостаточностью, пожилых, а также при одновременном применении с препаратами, ингибирующими ферментную систему цитохрома P450 и конъюгацию глюкуронида в печени [134-136]. При почечной недостаточности могут накапливаться активные метаболиты мидазолама и диазепама [137].
При длительном применении бензодиазепинов возможно длительное восстановление сознания после окончания введения за счет насыщения периферических тканей, особенно при печеночной, почечной недостаточности и в пожилом возрасте. Особенно большой длительностью действия обладает диазепам [138]. При применении бензодиазепинов возможна повышенная частота развития делирия.
В настоящее время наиболее часто применяется мидазолам. Начальная доза препарата 2-2,5 мг, последующие дозы 1 мг, общая доза 3,5-7,5 мг. Для пожилых пациентов начальная доза должна быть снижена до 0,5-1 мг, последующие дозы: 0,5-1 мг, общая доза < 3,5 мг, так как период полувыведения увеличивается в 2 раза.
Рекомендация 18. Для седации пациентов в ОАРИТ рекомендуется использовать пропофол или дексмедетомидин вместо бензодиазепинов [139-141]. Уровень достоверности доказательств 1, уровень убедительности рекомендаций A.
Комментарий. По сравнению с бензодиазепинами дексмедетомидин приводил к более ранней экстубации пациентов на ИВЛ и уменьшению времени пребывания в ОАРИТ [139] и сокращению ранней смертности [140].
В рандомизированном исследовании, в которое было включено 422 пациента с сепсисом на ИВЛ, было показано, что нет достоверных различий между дексмедетомидином и пропофолом по количеству дней без комы и делирия, а также без ИВЛ и смертности в течение 90 дней, а также выраженности когнитивных нарушений через 6 месяцев [141].
Использование для седации пропофола и дексмедетомидина улучшает клинические исходы для пациентов на ИВЛ [142-148]. В то же время дексмедетомидин увеличивал частоту развития брадикардии у всех пациентов ОАРИТ [143]. Показано, что дексмедетомидин позволяет обеспечивать необходимый уровень седации от 0 до -3 по шкале RASS, но не обеспечивает более глубокую седацию пациентов [149].
Дексмедетомидин увеличивает коммуникативность, снижает частоту делирия и ускоряет его разрешение. Рекомендован к использованию для седации в ОАРИТ [25, 150¬152].
В некоторых гайдлайнах рекомендовано у пациентов ОАРИТ на ИВЛ использовать дексмедетомидин вместо других седативных средств, если основной целью является предупреждение делирия и менее значимы нежелательные эффекты препарата, включая усиление гипотензии и брадикардии [153].
Пропофол, также, как и бензодиазепины, нарушает физиологическую структуру сна, в частности угнетает его быструю фазу и ухудшает качество сна в целом, что приводит к увеличению риска делирия. В отличие от него дексмедетомидин вызывает сон, соответствующий физиологическому паттерну [154].
В двух исследованиях, сравнивающих эффекты пропофола и дексмедетомидина при септическом шоке, не было обнаружено различий по состоянию гемодинамики, поэтому авторы делают вывод о возможности использованию обоих препаратов [155, 156]. При необходимости седации при артериальной гипотензии необходима инотропная поддержка.
По данным многоцентрового обсервационного ретроспективного исследования у 179 неврологических пациентов не было обнаружено различий между дексмедетомидином и пропофолом по продолжительности седации, ИВЛ и времени пребывания в стационаре, а также частоте развития артериальной гипотензии и брадикардии, однако летальность была достоверно выше в группе пропофола [157].
Рекомендация 19. Для седации пациентов на ИВЛ после кардиохирургических операций рекомендуется использовать дексмедетомидин или пропофол вместо бензодиазепинов [79]. Уровень достоверности доказательств 2, уровень убедительности рекомендаций В.
Комментарий. У кардиохирургических пациентов при применении
дексмедетомидина реже развивался делирий, сокращались сроки госпитализации, однако отмечалась склонность к брадикардии [158]. По данным систематического обзора и метаанализа K. Heybati et al. (2022) дексмедетомидин уменьшал длительность ИВЛ и риск делирия у кардиохирургических пациентов, но не влиял на время пребывания в ОАРИТ [142].
При применении дексмедетомидина делирий развивается достоверно реже, чем при использовании для седации пропофола или мидазолама, что подтверждается данными метаанализа [159].
Дексмедетомидин сохраняет когнитивные функции, не вызывает значительной депрессии дыхания, действует в течение короткого времени и быстро выводится из организма, уменьшает частоту послеоперационных аритмий, уменьшает продолжительность ИВЛ, обладает нефропротективным эффектом в послеоперационном периоде. В то же время дексмедетомидин не подходит для глубокой седации, может вызывать брадикардию и дозозависимые колебания АД (как гипотензию, так и гипертензию), тошноту и сухость во рту [160].
Рекомендация 20. Для седации пациентов при возбуждении и высоком риске делирия рекомендуется использовать дексмедетомидин [161 - 164]. Уровень достоверности доказательств 2, уровень убедительности рекомендаций A.
Комментарий. Для пациентов, требующих глубокой седации, в том числе с миорелаксантами, применяется пропофол. При возбуждении, препятствующем экстубации, предпочтительно введение дексмедетомидина. Каждый из препаратов может быть использован для пациентов, находящихся на вазопрессорной поддержке [165].
Рекомендация 21. При неинвазивной вентиляции легких (НИВЛ) рекомендуется проводить седацию при возбуждении или риске непереносимости НИВЛ [166, 167]. Уровень достоверности доказательств 1, уровень убедительности рекомендаций B.
Комментарий. При НИВЛ предпочтительно использовать дексмедетомидин, так как он не угнетает дыхание и обеспечивает эффективную профилактику и лечение делирия. При НИВЛ важно проводить тщательный мониторинг уровня седации для предотвращения слишком глубокой седации. [168].
Ингаляционные анестетики. В настоящее время в анестезиологии все большую популярность завоевывают ингаляционные анестетики (ИА). Важными преимуществами ИА являются возможность эффективного мониторинга их концентрации в конце выдоха и, как следствие, хорошая управляемость анестезией. Начало и конец действия ИА наступают очень быстро, так как они выводятся через легкие и мало кумулируются печенью и почками. Современные ИА (севофлуран, десфлуран в концентрации менее 1 MAC) не оказывают отрицательного влияния на центральную гемодинамику, что имеет особое значение для пациентов ОАРИТ, находящихся в критическом состоянии. Кроме того, в ряде работ описан кардиопротективный эффект севофлурана [169, 171].
В ОАРИТ используется устройство для ингаляционной седации The Anaesthetic Conserving Device (ACD) [172], которое было зарегистрировано в России в 2013 г. ACD включает модифицированный бактериальный фильтр с отражателем анестетика и пористый испаритель. Концентрация ИА в конце выдоха контролируется с помощью газового анализатора. В качестве ИА рекомендовано использование изофлурана или севофлурана.
В инструкции по медицинскому применению лекарственного препарата, размещенной в Государственном реестре лекарственных средств Российской Федерации, у севофлурана отсутствуют показания к седации, однако в настоящее время эффективность и безопасность ACD подтверждена рядом исследований, в том числе рандомизированных [172- 175].
Использование ингаляционных анестетиков в ОАРИТ вошло в рекомендации по проведению седации в Германии [176].
ACD используется вместе с обычными аппаратами искусственной вентиляции легких и подключается между Y-образным коннектором и интубационной трубкой, так же как бактериальный/вирусный фильтр. Помимо этого, данная система требует использования шприцевой помпы, монитора наркозного газа и системы выведения наркозного газа (возможно использование систем с адсорберами).
Применение севофлурана для продленной седации пациентов на ИВЛ позволяет снизить дозы опиатов и полностью отменить седативные препараты, вводимые внутривенно. У ряда пациентов с нестабильной гемодинамикой, выраженной гиповолемией возможно развитие артериальной гипотензии.
Рекомендуемая концентрация севофлурана на выдохе колеблется от 0,5% (при этом скорость подачи севофлурана через шприцевую помпу составляет от 1,5 до 2,5 мл/ч) до 1% (скорость инфузии составляет 5-6 мл/ч). Для достижения уровня седации 2-3 балла по шкале RASS применяется скорость введения севофлурана 2,5-5,0 мл/ч, при этом концентрация
анестетика в конце выдоха составляет около 0,75%. Скорость введения изофлурана несколько меньше и не превышает 3 мл/ч.
Возможно использование седации с помощью ACD как в течение нескольких часов в послеоперационном периоде до экстубации пациента, так и для длительной седации [174, 176].
Седация ИА противопоказана в тех случаях, когда имеются противопоказания к соответствующему препарату для ингаляционного наркоза [177]. ИА используются только у интубированных пациентов, могут вызвать глубокую седацию, угнетают дыхание и ограничивают подвижность [175].
Рекомендация 22. У пациентов на ИВЛ рекомендуется использование ингаляционных анестетиков (изофлурана и севофлурана) в качестве альтернативного метода седации [178, 179]. Уровень достоверности доказательств 2, уровень убедительности рекомендаций B.
Комментарий. Противопоказаниями к использованию галогенсодержащих ИА являются подтвержденная или подозреваемая генетическая предрасположенность к развитию злокачественной гипертермии, а также повышенная чувствительность к севофлурану или другим галогенизированным препаратам. ИА с осторожностью применяют при нарушении функции почек, нейрохирургических вмешательствах, если у пациента имеется угроза повышения внутричерепного давления. Повышение концентрации ИА вызывает дозозависимое снижение артериального давления; в таких случаях его можно повысить путем уменьшения концентрации подаваемого анестетика.
По данным систематического обзора, основанным на 13 РКИ, показано, что использование ингаляционных анестетиков в ОАРИТ уменьшает длительность ИВЛ и времени вне бодрствования. В то же время не отмечено влияния на летальность и время пребывания в ОАРИ Т [36].
Использование ингаляционных анестетиков в ОАРИТ способствует также уменьшению нежелательных пробуждений и спонтанных экстубаций [180].
В проспективном исследовании показано, что ингаляционные анестетики являются безопасной альтернативой внутривенной седации пропофолом и даже снижают потребление опиодиов в послеоперационном периоде [181].
Во время пандемии новой COVID-19 повысился интерес к ИА для седации в ОАРИТ. ИА имеют хороший профиль седации, быстро выводятся из организма и уменьшают воспалительный процесс в легких. Во Франции был проведен опрос, по результатам 25
которого 79% ОРИТ признали седацию ИА достойной альтернативой внутривенным препаратам, особенно для пациентов с COVID -19 [179].
Оказалось, что пациентам с COVID-19, в том числе с ОРДС, требуется большее количество седативных средств, и ИА являются хорошим дополнением к седации интубированных пациентов, при этом обладают бронходилатирующим и противовоспалительным эффектом, что является преимуществом в данном случае. Требуются дальнейшие исследования с привлечением различных специалистов для определения места ИА в лечении тяжелых форм новой коронавирусной инфекции [182].
В качестве перспективного средства аналгоседации может обсуждаться инертный газ ксенон. Согласно инструкции, ксенон рекомендован в качестве препарата для анестезии и анальгезии. В ряде научных работ доказано, что ксенон обладает анальгетическим, гипнотическим, нейро-, кардио-и ренопротективными эффектами, а также антигипоксическим, антиоксидантным и антистрессовым действием [183 - 186]. В
настоящее время отсутствуют РКИ по седации ксеноном в ОАРИТ, существуют единичные пилотные исследования, посвященные применению ксенона для седации в интенсивной терапии [186].
Рекомендация 23. У пациентов ОАРИТ рекомендуется проведение профилактики возникновения возбуждения [13]. Уровень достоверности доказательств 2, уровень убедительности рекомендаций С.
Комментарий. Профилактика возникновения возбуждения у пациентов в ОАРИТ включает следующие мероприятия:
• адекватное обезболивание;
• своевременное проведение седативной терапии;
• предпочтение легкой седации при отсутствии показаний к глубокой седации;
• регулярная оценка уровня седации или возбуждения с помощью оценочных шкал;
• частое общение медицинского персонала с пациентами, объяснение проводимых процедур лечения и ухода, привлечение родственников;
• ориентировка пациентов во времени и пространстве;
• физическая активность, ранняя мобилизация пациентов;
• избегание ненужной фиксации пациентов;
• уменьшение шума;
• обеспечение ночного сна.
Соблюдение основных принципов проведения седации в ОАРИТ, в первую очередь обеспечения адекватной анальгезии, а также разработка надежных алгоритмов и шкал оценки седации непосредственно у постели пациента позволяют улучшить качество лечения. Современные методы оценки психоэмоционального статуса пациентов в ОАРИТ дают возможность контролировать исходы, связанные с нефармакологическими и фармакологическими методами аналгоседации, осуществлять мониторинг и управление уровнем седации. У большинства пациентов ОАРИТ обеспечение легкой степени седации связано с лучшими клиническими исходами.
Члены рабочей группы при обновлении методических рекомендаций использовали результаты дельфийской экспертизы предыдущей версии, выполненной независимыми специалистами [187].
Критерии оценки качества медицинской помощи
№ Критерии качества* Уровень достоверности доказательств Уровень убедительности рекомендаций
1 Проведение адекватного обезболивания в случае наличия боли перед началом седации 1 A
2 Оценка возбуждения и уровня седации по шкале RASS 1 А
3 Поддержание легкой степени седации при отсутствии специальных показаний к глубокой седации 1 B
4 Проведение регулярной переоценки
седативной терапии 1 В
5 Наличие протокола седации 2 B
6 Использование небензодиазепиновых
препаратов для седации (пропофол, дексмедетомидин) при отсутствии
специальных показаний к назначению производных бензодиазепинов 2 B
Приложение А1. Состав рабочей группы
Потиевская Вера Исааковна - доктор медицинских наук, главный научный сотрудник ФГБУ «Национальный медицинский исследовательский радиологический центр» Минздрава России, член Общероссийской общественной организации «Федерация анестезиологов и реаниматологов», член Российского кардиологического общества, Москва, отв. редактор.
Заболотских Игорь Борисович - доктор медицинских наук, профессор, заведующий кафедрой анестезиологии, реаниматологии и трансфузиологии ФПК и ППС ФГБОУ ВО «Кубанский государственный медицинский университет» Минздрава России, главный научный сотрудник ФГБНУ «ФНКЦ реаниматологии и реабилитологии» Минобрнауки России, руководитель анестезиолого-реанимационной службы ГБУЗ «Краевая клиническая больница №2» МЗ КК, Первый Вице-Президент Общероссийской общественной организации «Федерация анестезиологов и реаниматологов», Краснодар, отв. редактор.
Гридчик Ирина Евгеньевна - доктор медицинских наук, профессор, профессор кафедры анестезиологии и реаниматологии ФГБОУ ДПО «Российская медицинская академия непрерывного последипломного образования» Минздрава России, член Общероссийской общественной организации «Федерация анестезиологов и реаниматологов», Москва.
Грицан Алексей Иванович - доктор медицинских наук, профессор, заведующий кафедрой анестезиологии и реаниматологии ИПО ФГБОУ ВО «Красноярский государственный медицинский университет имени. профессора В.Ф. Войно-Ясенецкого» Минздрава России, главный внештатный анестезиолог-реаниматолог министерства здравоохранения Красноярского края и Сибирского Федерального округа,, Представитель России в Совете Европейского общества интенсивной терапии (ESICM), вице-президент Общероссийской общественной организации «Федерация анестезиологов и реаниматологов», Красноярск.
Еременко Александр Анатольевич - доктор медицинских наук, профессор, член- корр. РАН, руководитель отделения кардиореанимации и интенсивной терапии ФГБНУ «Российский научный центр хирургии имени академика Б.В. Петровского», заслуженный деятель науки РФ, заслуженный врач РФ, член Общероссийской общественной организации «Федерация анестезиологов и реаниматологов», Москва.
Козлов Игорь Александрович - доктор медицинских наук, профессор, профессор кафедры анестезиологии и реаниматологии ГБУЗ МО «МОНИКИ им. М. Ф.
Владимирского», член Общероссийской общественной организации «Федерация анестезиологов и реаниматологов», Москва.
Левит Александр Львович - доктор медицинских наук, профессор, заслуженный врач РФ, главный анестезиолог-реаниматолог Минздрава Свердловской области, член Общероссийской общественной организации «Федерация анестезиологов и
реаниматологов», Екатеринбург.
Мазурок Вадим Альбертович - доктор медицинских наук, профессор, заведующий кафедрой анестезиологии и реаниматологии Института медицинского образования ФГБУ «Северо-Западный федеральный медицинский исследовательский центр им. В.А. Алмазова» Минздрава России, член Общероссийской общественной организации «Федерация анестезиологов и реаниматологов», Санкт-Петербург
Молчанов Игорь Владимирович - доктор медицинских наук, профессор, профессор кафедры анестезиологии и реаниматологии ФГБОУ ДПО «Российская медицинская академия непрерывного последипломного образования» Минздрава России, главный внештатный специалист анестезиолог-реаниматолог Министерства здравоохранения Российской Федерации, Почетный член Общероссийской общественной организации «Федерация анестезиологов и реаниматологов», Москва.
Авторы заявляют об отсутствии конфликта интересов.
Приложение А2. Методология разработки клинических рекомендаций
Целевая аудитория данных методических рекомендаций:
Врачи-анестезиологи-реаниматологи
Таблица А2.1. Шкала оценки УДД для диагностических вмешательств.
УДД Иерархия дизайнов клинических исследований по убыванию уровня достоверности доказательств от 1 до 5
1 систематические обзоры исследований с контролем референсным методом
2 Отдельные исследования с контролем референсным методом
3 Исследования без последовательного контроля референсным методом или исследования с референсным методом, не являющимся независимым от исследуемого метода
4 Несравнительные исследования, описание клинического случая
5 Имеется лишь обоснование механизма действия или мнение экспертов
Таблица А2.2. Шкала определения УУР для диагностических вмешательств УУР.
УУР Расшифровка
А Однозначная (сильная) рекомендация (все исследования имеют высокое или удовлетворительное методологическое качеств, их выводы по интересующим исходам являются согласованными)
В Неоднозначная (условная) рекомендация (не все исследования имеют высокое или удовлетворительное методологическое качество и/или их выводы по интересующим исходам не являются согласованными)
С Низкая (слабая) рекомендация - отсутствие доказательств надлежащего качества (все исследования имеют низкое методологическое качество и их выводы по интересующим исходам не являются согласованными)
Таблица А2.3. Шкала определения УДД для лечебных, реабилитационных, профилактических вмешательств.
УДД Иерархия дизайнов клинических исследований по убыванию уровня достоверности доказательств от 1 до 5
1 Систематический обзор РКИ с применением мета-анализа
2 Отдельные РКИ и систематические обзоры исследований любого дизайна (помимо РКИ) с применением мета-анализа
3 Нерандомизированные сравнительные исследования, в т.ч. когортные
исследования
4 Несравнительные исследования, описание клинического случая или серии случаев, исследования «случай-контроль»
5 Имеется лишь обоснование механизма действия вмешательства (доклинические исследования) или мнение экспертов
Таблица А2.4. Шкала определения УУР для лечебных, реабилитационных, профилактических, вмешательств.
УУР Расшифровка
А Однозначная (сильная) рекомендация (все исследования имеют высокое или
удовлетворительное методологическое качеств, их выводы по интересующим исходам являются согласованными)
В Неоднозначная (условная) рекомендация (не все исследования имеют высокое или удовлетворительное методологическое качество и/или их выводы по интересующим исходам не являются согласованными)
С Низкая (слабая) рекомендация - отсутствие доказательств надлежащего качества (все исследования имеют низкое методологическое качество и их выводы по интересующим исходам не являются согласованными)
Приложение А3. Связанные документы
Данные методические рекомендации разработаны с учётом следующих нормативно¬правовых документов:
1) Порядок оказания медицинской помощи по Приказ Минздрава России от 15.11.2012 N 919н «Об утверждении Порядка оказания медицинской помощи взрослому населению по профилю «анестезиология и реаниматология»
2) Приказ Минздрава РФ от 10.05.2017 N 203н - Об утверждении критериев оценки
качества медицинской помощи - Действующая первая редакция - Зарегистрировано в Минюсте РФ 17.05.2017 N46740 - Начало действия документа 01.07.2017.
Приложение Б1. Алгоритм седации. Порядок проведения седации в ОАРИТ.
Приложение Б2. Алгоритм седации. Стратегия седации в ОАРИТ.
Приложение В. Информация для пациента
Во время пребывания в отделении реанимации будет гореть свет, в том числе и в ночное время, будет шум, звуки мониторов и аппаратов, будут поступать другие пациенты, посещения родственников обычно
кратковременны. В отделении реанимации и интенсивной терапии могут проводиться инвазивные процедуры, которые требуют обезболивания и назначения седативных препаратов. Седативные препараты могут быть назначены в случае необходимости искусственной вентиляции легких при дыхательной недостаточности, а также для снятия тревоги и нормализации сна.
Приложение Г. Ричмондская шкала возбуждения-седации (RASS)
Название на русском языке: Ричмондская шкала возбуждения-седации
Оригинальное название: Richmond Agitation-Sedation Scale
Источник (официальный сайт разработчиков, публикация с
валидацией): Ely EW, Truman B, Shintani A, Thomason JWW, Wheeler AP, Gordon S et al. Monitoring sedation status over time in ICU patients: the reliability and validity of the Richmond Agitation Sedation Scale (RASS). JAMA 2003; 289:2983-2991
Тип (подчеркнуть):
- шкала оценки
- индекс
- вопросник
другое (уточнить):
Назначение: оценка уровня седации
Оценочный инструмент, содержание:
Баллы Термин Описание
+4 Агрессивный Настроен враждебно или агрессивно, представляет
непосредственную опасность для персонала
+3 Очень сильно возбуждён Тянет или удаляет трубки, катетеры и т.д., или агрессивен по отношению к персоналу
+2 Возбуждён Частые бессмысленные движения или десинхронизация пациента с ИВЛ
+1 Беспокоен Взволнован, но движения не носят агрессивный или энергичный характер
0 Тревога и
спокойствие
-1 Сонливый Не в полном сознании, но без пробуждения (более 10 секунд), зрительный контакт в ответ на голос
-2 Легкая седация Пробуждается на короткий период времени (менее 10 секунд), зрительный контакт в ответ на голос
-3 Умеренная седация Движение в ответ на голос, без зрительного контакта
-4 Глубокая седация Никакой реакции в ответ на голос, движение в ответ на физическую стимуляцию
-5 Отсутствие пробуждения Никакой реакции на голос или физическую стимуляцию
Ключ (интерпретация):
- RASS от -3 баллов и менее - слишком глубокая седации
- RASS 2 и более баллов - недостаточная седация, возбуждение
- RASS от -2 до 0 баллов - оптимальный уровень седации
Пояснения (при необходимости) Следует избегать чрезмерного углубления седации (меньше -2 баллов по RASS), если для этого нет показаний
.
Список литературы:
2. The San Diego Patient Safety Council. ICU Sedation Guidelines of Care. — 2009.
3. Венсан Ж.-Л., Абрахам Э., Мур Ф. - Руководство по критической медицине. Том 1. 7-е издание.
4. DeBiasi Е.М. Akgün K. M., Pisani M. Trends in the Evaluation and Management of Agitation in the ICU. Semin Respir Crit Care Med 2015;36:899–913.
5. Devlin JW, Skrobik Y, Gelinas C, Needham DM, Slooter AJC, Pandharipande PP, Watson PL, Weinhouse GL, Nunnally ME, Rochwerg B et al (2018) Clinical practice guidelines for the prevention and management of pain, agitation/sedation, delirium, immobility, and sleep disruption in adult patients in the ICU. Crit Care Med 46(9):e825–e873
6. Pearson SD, Patel BK. Evolving targets for sedation during mechanical ventilation. Curr Opin Crit Care. 2020 Feb;26(1):47-52. doi: 10.1097/MCC.0000000000000687. PMID: 31764193; PMCID: PMC8086012.
7. Porhomayon J, A Joude P, Adlparvar G, et al. The impact of high versus low sedation dosing strategy on cognitive dysfunction in survivors of intensive care units: a systematic review and meta-analysis. J Cardiovasc Thorac Res. 2015;7(2):43. doi:10.15171/jcvtr.2015.10
8. Sharma S, Hashmi MF, Valentino III DJ. Sedation Vacation in the ICU. 2022 Nov 6. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan–. PMID: 30020699.
9. Козлов И.А. Современные подходы к седации в отделениях реанимации и интенсивной терапии // Медицинский алфавит. Неотложная медицина. — 2013. — №1. — С. 22–31.
10. Kress JP, Pohlman AS, O’Connor MF, et al. Daily interruption of sedative infusions in critically ill patients undergoing mechanical ventilation. N Engl J Med 2000; 342:14711477.
11. Timothy D Girard, Jennifer L Thompson, Pratik P Pandharipande, Nathan E Brummel, James C Jackson, Mayur B Patel, Christopher G Hughes, Rameela Chandrasekhar, Brenda T Pun, Leanne M Boehm, Mark R Elstad, Richard B Goodman, Gordon R Bernard, Robert S Dittus, E W Ely, Clinical phenotypes of delirium during critical illness and severity of subsequent long-term cognitive impairment: a prospective cohort study, The Lancet Respiratory Medicine, Volume 6, Issue 3, 2018, Pages 213-222, ISSN 2213-2600, https://doi.org/10.1016/S2213- 2600(18)30062-6. (https://www.sciencedirect.com/science/article/pii/S2213260018300626).
12. Pun BT, Balas MC, Barnes-Daly MA, Thompson JL, Aldrich JM, Barr J, et al. Caring for critically ill patients with the ABCDEF bundle: results of the ICU liberation collaborative in over 15,000 adults. Crit Care Med. 2019;47(1):3–14. https://doi.org/10.1097/
13. . Vincent J, Shehabi Y, Walsh TS, Pandharipande P, Ball JA, Spronk P, et al. Comfort and patient-centred care without excessive sedation: the eCASH concept. Intensive Care Med 2016;42:962–71.
14. Walsh TS, Kydonaki K, Antonelli J, et al.; Development and Evaluation of Strategies to Improve Sedation Practice in Intensive Care (DESIST) Study Investigators: Staff education, regular sedation and analgesia quality feedback, and a sedation monitoring technology for improving sedation and analgesia quality for critically ill, mechanically ventilated patients: A cluster randomised trial. Lancet Respir Med 2016; 4:807817.
15. Kiesewetter I, Bartels U, Bauer A, Schneider G, Pilge S. The German version of the Critical-Care Pain Observation Tool for critically ill adults : A prospective validation study. Anaesthesist. 2019 Dec;68(12):836-842. English. doi: 10.1007/s00101-019-00694-5. Epub 2019 Nov 20. PMID: 3174883.
16. Rivosecchi RM, Kane-Gill SL, Svec S, et al. The implementation of a nonpharmacologic protocol to prevent intensive care delirium. J Crit Care 2016; 31:206211
17. Wøien H. Movements and trends in intensive care pain treatment and sedation: What matters to the patient? J Clin Nurs. 2020 Apr;29(7-8):1129-1140. doi: 10.1111/jocn.15179. Epub 2020 Jan 21. PMID: 31904888.]
18. B. Hutton, L.D. Burry, S. Kanji, S. Mehta, M. Guenette, C.M. Martin, et al., Comparison of sedation strategies for critically ill patients: a protocol for a systematic review incorporating network meta-analyses, Syst. Rev. 5 (1) (2016) 1–7
19. G. Park, D. Coursin, E.W. Ely, M. England, G.L. Fraser, J. Mantz, et al., Commentary. Balancing sedation and analgesia in the critically ill, Crit. Care Clin. 17 (4) (2001) 1015–1027].
20. Cinotti R, Besnard N, Desmedt L, Floch RL, Perrot P, Bekara F, Klouche K, Larcher R, Mahé PJ, Frasca D, Asehnoune K, Jung B, Roquilly A. Feasibility and impact of the implementation of a clinical scale-based sedation-analgesia protocol in severe burn patients undergoing mechanical ventilation. A before-after bi-center study. Burns. 2020 Sep;46(6):1310- 1317. doi: 10.1016/j.burns.2020.02.009. Epub 2020 Mar 8. PMID: 32156477].
21. Овечкин А.М., Баялиева А.Ж., Ежевская А.А., Еременко А.А., Заболотский Д.В., Заболотских И.Б., Карелов А.Е., Корячкин В.А., Спасова А.П. Хороненко В.Э., Уваров
Д.Н., Ульрих Г.Э., Шадрин Р.В. Послеоперационное обезболивание. Клинические рекомендации. Вестник интенсивной терапии им. А.И. Салтанова. 2019;4:9–33.
22. Van Rompaey B, Elseviers MM, Van Drom W, Fromont V, Jorens PG. The effect of earplugs during the night on the onset of delirium and sleep perception: a randomized controlled trial in intensive care patients. Crit Care 2012;16:R73.
23. Patel J, Baldwin J, Bunting P, Laha S. The effect of a multicomponent multidisciplinary bundle of interventions on sleep and delirium in medical and surgical intensive care patients. Anaesthesia 2014;69:540-9.
24. Alexopoulou C, Kondili E, Diamantaki E, Psarologakis C, Kokkini S, Bolaki M, et al. Effects of dexmedetomidine on sleep quality in critically ill patients: a pilot study. Anesthesiology 2014;121:801-7].
25. Seo Y, Lee HJ, Ha EJ, Ha TS. 2021 KSCCM clinical practice guidelines for pain, agitation, delirium, immobility, and sleep disturbance in the intensive care unit. Acute Crit Care. 2022 Feb;37(1):1-25. doi: 10.4266/acc.2022.00094. Epub 2022 Feb 28. PMID: 35279975; PMCID: PMC8918705
26. Shehabi Y, Bellomo R, Reade MC, Bailey M, Bass F, Howe B, McArthur C, Seppelt IM, Webb S, Weisbrodt L et al (2012) Early intensive care sedation predicts long-term mortality in ventilated critically ill patients. Am J Respir Crit Care Med 186(8):724–731
27. Olsen HT, Nedergaard HK, Strom T, Oxlund J, Wian KA, Ytrebo LM, Kroken BA, Chew M, Korkmaz S, Lauridsen JT et al (2020) Nonsedation or light sedation in critically ill, mechanically ventilated patients. N Engl J Med 382(12):1103–1111].
28. Treggiari M: Randomized trial of light versus deep sedation on mental health after critical illness. Crit Care Med 2010, 38(1):349-350
29. Shehabi Y, Bellomo R, Reade MC, et al; Sedation Practice in Intensive Care Evaluation Study Investigators; Australian and New Zealand Intensive Care Society Clinical Trials Group: Early goal-directed sedation versus standard sedation in mechanically ventilated critically ill patients: A pilot study. Crit Care Med 2013; 41:1983–1991
30. Tanaka LM, Azevedo LC, Park M, et al; ERICC Study Investigators: Early sedation and clinical outcomes of mechanically ventilated patients: A prospective multicenter cohort study. Crit Care 2014; 18:R156.
31. Aragón RE, Proaño A, Mongilardi N, de Ferrari A, Herrera P, Roldan R, Paz E, Jaymez AA, Chirinos E, Portugal J, Quispe R, Brower RG, Checkley W. Sedation practices and clinical
outcomes in mechanically ventilated patients in a prospective multicenter cohort. Crit Care. 2019 Apr 17;23(1):130. doi: 10.1186/s13054-019-2394-9. PMID: 30995940; PMCID: PMC6472077.
32. Stollings J. L, Balas M. C., Chanques G. Evolution of sedation management in the intensive care unit (ICU). Intensive Care Med (2022) 48:1625–1628 https://doi.org/10.1007/s00134- 022-06806-
33. Sessler CN, Gosnell MS, Grap MJ, et al. The Richmond Agitation-Sedation Scale: Validity and reliability in adult intensive care unit patients. Am J Respir Crit Care Med 2002; 166:13381344
34. Papazian L, Forel JM, Gacouin A, et al. Neuromuscular blockers in early acute respiratory distress syndrome. N Engl J Med 2010;363:1107-16.
35. Katherine Rowe, Simon Fletcher, Sedation in the intensive care unit, Continuing Education in Anaesthesia Critical Care & Pain, Volume 8, Issue 2, 2008, Pages 50-55, ISSN 1743- 1816, https://doi.org/10.1093/bjaceaccp/mkn005].
36. Temesgen N, Chekol B, Tamirie T, Eshetie D, Simeneh N, Feleke A. Adult sedation and analgesia in a resource limited intensive care unit - A Systematic Review and evidence based guideline. Ann Med Surg (Lond). 2021 Apr 30;66:102356. doi: 10.1016/j.amsu.2021.102356. PMID: 34035907; PMCID: PMC8138481
37. Talsi O, Kiiski Berggren R, Johansson G, Winsö O. A national survey on routines regarding sedation in Swedish intensive care units. Ups J Med Sci. 2019 Aug;124(3):199-202. doi: 10.1080/03009734.2019.1616339. Epub 2019 May 23. PMID: 31119971; PMCID: PMC6758647.
38. Neme D, Aweke Z, Micho H, Mola S, Jemal B, Regasa T. Evidence-Based Guideline for Adult Sedation, Pain Assessment, and Analgesia in a Low Resource Setting Intensive Care Unit: Review Article. Int J Gen Med. 2020 Dec 8;13:1445-1452. doi: 10.2147/IJGM.S276878. PMID: 33335417; PMCID: PMC7737551.
39. Nassar Jr AP, Park M. Daily sedative interruption versus intermittent sedation in mechanically ventilated critically ill patients: a randomized trial. Ann Intensive Care 2014;4:14. 20.
40. Girard TD, Kress JP, Fuchs BD, Thomason JWW, Schweickert WD, Pun BT, et al. Efficacy and safety of a paired sedation and ventilator weaning protocol for mechanically ventilated patients in intensive care (Awakening and Breathing [Controlled Trial): a randomised controlled trial. Lancet 2008; 371:126–34
41. Kress JP, Pohlman AS, O’Connor MF, Hall J. Daily interruption of sedative infusions in critically ill patients undergoing mechanical ventilation. N Engl J Med 2000; 42: 1471-1477. doi: 10.1056/NEJM 200005183422002
42. Strøm T, Martinussen T, Toft P. A protocol of no sedation for critically ill patients receiving mechanical ventilation: a randomized trial. Lancet 2010; 375: 475-480. doi: 10.1016/S0140- 6736(09)62072-9.
43. Vagionas D, Vasileiadis I, Rovina N, Alevrakis E, Koutsoukou A, Koulouris N. Daily sedation interruption and mechanical ventilation weaning: a literature review. Anaesthesiol Intensive Ther. 2019;51(5):380-389. doi: 10.5114/ait.2019.90921. PMID: 31893604
44. Jackson JC, Girard TD, Gordon SM, et al. Long-term cognitive and psychological outcomes in the awakening and breathing controlled trial. Am J Respir Crit Care Med 2010; 182:183– 191. [PubMed: 20299535].
45. Kress JP, Gehlbach B, Lacy M, et al. The long-term psychological effects of daily sedative interruption on critically ill patients. Am J Respir Crit Care Med 2003; 168:1457–1461. [PubMed: 14525802].
46. Strøm T, Stylsvig M, Toft P. Long-term psychological effects of a no-sedation protocol in critically ill patients. Crit Care 2011; 15:R293. [PubMed: 22166673
47. Baron R. et al. Evidence and consensus based guideline for the management of delirium, analgesia, and sedation in intensive care medicine. Revision 2015 (DAS-Guideline 2015)– short version //GMS German Medical Science. – 2015. – Т. 13
48. Institute for Healthcare Improvement. How-to guide: prevent ventilatorassociated pneumonia [Internet]. Cambridge, MA: Institute for Healthcare Improvement; 2012. Available from, www.ihi.org.
49. Graham ND, Graham ID, Vanderspank-Wright B, Varin MD, Nadalin Penno L, Fergusson DA, Squires JE. A systematic review and critical appraisal of guidelines and their recommendations for sedation interruptions in adult mechanically ventilated patients. Aust
Crit Care. 2022 Dec 13:S1036-7314(22)00224-7. doi: 10.1016/j.aucc.2022.10.011. Epub
ahead of print. PMID: 36522246
50. Donato M, Carini FC, Meschini MJ, Saubidet IL, Goldberg A, Sarubio MG, Olmos D, Reina
R. Consensus for the management of analgesia, sedation and delirium in adults with COVID- 19-associated acute respiratory distress syndrome. Rev Bras Ter Intensiva. 2021 Jan- Mar;33(1):48-67. doi: 10.5935/0103-507X.20210005. PMID: 33886853; PMCID: PMC8075332
51. Skoglund K, Enblad P, Marklund N (2009) Effects of the neurological wake-up test on intracranial pressure and cerebral perfusion pressure in brain-injured patients. Neurocrit Care 11:135–142
52. Helbok R, Kurtz P, Schmidt MJ, Fernandez L, Connolly SE, Lee K, Schmutzhard E, Mayer SA, Claassen J, Badjatia N (2012) Effects of the neurological wake-up test on clinical examination, intracranial pressure, brain metabolism and brain tissue oxygenation in severely brain-injured patients. Crit Care 16:R226
53. Celis-Rodriguez E, Diaz Cortes JC, Cardenas Bolivar YR, Carrizosa Gonzalez JA, Pinilla D- I, Ferrer Zaccaro LE, et al. Evidence-based clinical practice guidelines for the management of sedoanalgesia and delirium in critically ill adult patients. Med Intensiva 2020;44(3):171e84
54. Алексеева Г.В., Гурвич А.М., Семченко В.В. Постреанимационная энцефалопатия (патогенез, клиника, профилактика и лечение). — 2-е изд., доп. и перераб. — Омск: Омская областная типография, 2002. — 152 с.
55. Алексеева Г.В., Молчанов И.В., Семченко В.В. Клиническая неврология и интенсивная терапия постреанимационного поражения нервной системы (острый период). Пособие для врачей (утв. Ученым Советом МЗ и СРРФ (2006), 26 с.
56. University of Virginia Health System. Level I. Trauma Center. Trauma Handbook, 2012. — 141 p.
57. Yang KS, Habib AS, Lu M, et al. A prospective evaluation of the incidence of adverse events in nurse-administered moderate sedation guided by sedation scores or bispectral index. Anesth Analg 2014; 119:4348.
58. Shetty RM, Bellini A, Wijayatilake DS, Hamilton MA, Jain R, Karanth S, et al. BIS monitoring versus clinical assessment for sedation in mechanically ventilated adults in the intensive care unit and its impact on clinical outcomes and resource utilization. Cochrane Database Syst Rev. 2018;2(2):CD011240. https://doi. org/10.1002/14651858.CD011240.pub2]
59. Poignant S, Vigué B, Balram P, Biais M, Carillon R, Cottenceau V, Dahyot-Fizelier C, Degos V, Geeraerts T, Jeanjean P, Vega E, Lasocki S, Espitalier F, Laffon M; ANARLF and AtlanRea Network for the SEDABIP ICU Study. A One-Day Prospective National Observational Study on Sedation-Analgesia of Patients with Brain Injury in French Intensive Care Units: The SEDA-BIP-ICU (Sedation-Analgesia in Brain Injury Patient in ICU) Study. Neurocrit Care. 2022 Feb;36(1):266-278. doi: 10.1007/s12028-021-01298-x. Epub 2021 Jul 30. PMID: 34331208
60. Shehabi Y, Bellomo R, Reade MC, et al.; Sedation Practice in Intensive Care Evaluation (SPICE) Study Investigators; ANZICS Clinical Trials Group: Early intensive care sedation predicts long-term mortality in ventilated critically ill patients. Am J Respir Crit Care Med 2012; 186:724731.
61. Mahmood S, Parchani A, El-Menyar A, et al: Utility of bispectral index in the management of multiple trauma patients. Surg Neurol Int 2014; 5:141
62. Wang ZH, Chen H, Yang YL, et al. Bispectral index can reliably detect deep sedation in mechanically ventilated patients: A prospective multicenter validation study. Anesth Analg 2017; 125:176183.
63. Oddo M., Crippa I.A., Mehta S., Menon D., Payen J.-F., Taccone F.S., Citerio G. Optimizing sedation in patients with acute brain injury. Critical Care (2016) 20:128/DOI 10.1186/s13054-016-1294-5/
64. Opdenakker O, Vanstraelen A, De Sloovere V, Meyfroidt G. Sedatives in neurocritical care: an update on pharmacological agents and modes of sedation. Curr Opin Crit Care. 2019 Apr;25(2):97-104.
65. Hawryluk GWJ, Aguilera S, Buki A, Bulger E, Citerio G, Cooper DJ, Arrastia RD, Diringer M, Figaji A, Gao G, Geocadin R, Ghajar J, Harris O, Hoffer A, Hutchinson P, Joseph M, Kitagawa R, Manley G, Mayer S, Menon DK, Meyfroidt G, Michael DB, Oddo M, Okonkwo D, Patel M, Robertson C, Rosenfeld JV, Rubiano AM, Sahuquillo J, Servadei F, Shutter L, Stein D, Stocchetti N, Taccone FS, Timmons S, Tsai E, Ullman JS, Vespa P, Videtta W, Wright DW, Zammit C, Chesnut RM. A management algorithm for patients with intracranial pressure monitoring: the Seattle International Severe Traumatic Brain Injury Consensus Conference
(SIBICC). Intensive Care Med. 2019 Dec;45(12):1783-1794. doi: 10.1007/s00134-019-05805-9. Epub 2019 Oct 28. PMID: 31659383; PMCID: PMC6863785
66. Prabhakar H, Tripathy S, Gupta N, Singhal V, Mahajan C, Kapoor I, Wanchoo J, Kalaivani M. Consensus Statement on Analgo-sedation in Neurocritical Care and Review of Literature. Indian J Crit Care Med. 2021 Feb;25(2):126-133. doi: 10.5005/jp-journals-10071-23712. PMID: 33707888; PMCID: PMC7922463.
67. Rai S, Drislane FW. Treatment of Refractory and Super-refractory Status Epilepticus. Neurotherapeutics. 2018 Jul;15(3):697-712. doi: 10.1007/s13311-018-0640-5. PMID: 29922905; PMCID: PMC6095773.].
68. Caronna E, Vilaseca A, Maria Gràcia Gozalo R, Sanchez Corral A, Santafé M, Sueiras M, Guzmán L, Quintana M, Toledo-Argany M, Santamarina E. Long-term prognosis related to deep sedation in refractory status Epilepticus. Acta Neurol Scand. 2020 Dec;142(6):555- 562. doi: 10.1111/ane.13302. Epub 2020 Jul 29. PMID: 32614067
69. Holtkamp M. The anaesthetic and intensive care of status epilepticus. Current Opinion in Neurology, 2007? 20(2), 188–193. doi:10.1097/wco.0b013e328042bacb
70. Chanques G, Kress JP, Pohlman A, Patel S, Poston J, Jaber S, Hall JB (2013) Impact of ventilator adjustment and sedation-analgesia practices on severe asynchrony in patients ventilated in assist-control mode. Crit Care Med 41:2177–2187
71. Wong IMJ, Thangavelautham S, Loh SCH, Ng SY, Murfin B, Shehabi Y. Sedation and Delirium in the Intensive Care Unit-A Practice-Based Approach. Ann Acad Med Singap. 2020 Apr;49(4):215-225. PMID: 32419006
72. Chanques G, Conseil M, Roger C, Constantin JM, Prades A, Carr J, Muller L, Jung B, Belafa F, Cisse M, Delay JM, de Jong A, Lefrant JY, Futier E, Mercier G, Molinari N, Jaber S (2017) Immediate interruption of sedation compared with usual sedation care in critically ill postoperative patients (SOS-Ventilation): a randomised, parallel-group clinical trial. Lancet RespirMed 5:795–805
73. Pearson SD, Patel BK. Evolving targets for sedation during mechanical ventilation. Curr Opin Crit Care. 2020 Feb;26(1):47-52. doi: 10.1097/MCC.0000000000000687. PMID: 31764193; PMCID: PMC8086012]..
74. Kapp CM, Zaeh S, Niedermeyer S, Punjabi NM, Siddharthan T, Damarla M. The use of analgesia and sedation in mechanically ventilated patients with COVID-19 ARDS. Anesth Analg. 2020
75. Karamchandani K, Dalal R, Patel J, Modgil P, Quintili A. Challenges in Sedation Management in Critically Ill Patients with COVID-19: a Brief Review.Curr Anesthesiol Rep. 2021;11(2):107-115. doi: 10.1007/s40140-021-00440-x. Epub 2021 Feb 26.PMID: 33654458].PMID: 33654458
76. Luz M, Brandão Barreto B, de Castro REV, Salluh J, Dal-Pizzol F, Araujo C, De Jong A, Chanques G, Myatra SN, Tobar E, Gimenez-Esparza Vich C, Carini F, Ely EW, Stollings JL, Drumright K, Kress J, Povoa P, Shehabi Y, Mphandi W, Gusmao-Flores D. Practices in sedation, analgesia, mobilization, delirium, and sleep deprivation in adult intensive care units (SAMDS-ICU): an international survey before and during the COVID-19 pandemic. Ann Intensive Care. 2022 Feb 4;12(1):9. doi: 10.1186/s13613-022-00985-y. PMID: 35122204; PMCID: PMC8815719.
77. Shehabi Y, Bellomo R, Kadiman S, Ti LK, Howe B, Reade MC, et al. Sedation intensity in the first 48 hours of mechanical ventilation and 180-day mortality: a multinational prospective longitudinal cohort study. Crit Care Med 2018;46:850–9
78. Stephens, Robert J. BS1; Dettmer, Matthew R. MD2; Roberts, Brian W. MD3; Ablordeppey, Enyo MD, MPH4,5; Fowler, Susan A. MLIS6; Kollef, Marin H. MD7; Fuller, Brian
M. MD, MSCI4,5. Practice Patterns and Outcomes Associated With Early Sedation Depth in Mechanically Ventilated Patients: A Systematic Review and Meta-Analysis. Critical Care Medicine 46(3): p 471-479, March 2018. | DOI: 10.1097/CCM.0000000000002885
79. Noel C, Mallemat H. Sedation and Analgesia for Mechanically Ventilated Patients in the Emergency Department. Emerg Med Clin North Am. 2019 Aug;37(3):545-556. doi: 10.1016/j.emc.2019.04.004. Epub 2019 May 16. PMID: 31262420.
80. Brattebо G, Hofoss D, Flaatten H, et al. Effect of a scoring system and protocol for sedation on duration of patients’ need for ventilator support in a surgical intensive care unit. BMJ 2002; 324:13861389.
81. Tanaka et al.: Early sedation and clinical outcomes of mechanically ventilated patients: a prospective multicenter cohort study. Critical Care 2014 18:R156.
82. Shah F. A., Girard T. D., Yende S. Limiting sedation for patients with acute respiratory distress syndrome – time to wake up. Curr Opin Crit Care 2017, 23:45–51.
83. Girard TD, Kress JP, Fuchs BD, et al. Efficacy and safety of a paired sedation and ventilator weaning protocol for mechanically ventilated patients in intensive care (Awakening and Breathing Controlled trial): A randomised controlled trial. Lancet 2008; 371:126134
84. Aitken LM, Bucknall T, Kent B, Mitchell M, Burmeister E, Keogh SJ. Protocol- directed sedation versus non-protocol-directed sedation in mechanically ventilated intensive care adults and children. Cochrane Database Syst Rev. 2018;11(11): 009771. https://doi. org/10.1002/14651858.CD009771.pub3
85. Heim M, Draheim R, Krupp A, Breihan P, O'Rourke A, Wells J, Fish J. Evaluation of a Multidisciplinary Pain, Agitation, and Delirium Guideline in Mechanically Ventilated Critically Ill Adults. Hosp Pharm. 2019 Apr;54(2):119-124. doi: 10.1177/0018578718769570. Epub 2018 Apr 18. PMID: 30923405; PMCID: PMC6431725
86. Billington ME, Seethala RR, Hou PC, Takhar SS, Askari R, Aisiku IP; USIITG- CIOS investigators. Differences in prevalence of ICU protocols between neurologic and non- neurologic patient populations. J Crit Care. 2019 Aug;52:63-67. doi: 10.1016/j.jcrc.2019.03.002. Epub 2019 Mar 27. PMID: 30981927
87. Ismaeil MF, El-Shahat HM, El-Gammal MS, et al: Unplanned versus planned extubation in respiratory intensive care unit, predictors of outcome. Egypt J Chest Dis Tuberc 2014; 63:219–231
88. Rose L, Burry L, Mallick R, et al: Prevalence, risk factors, and outcomes associated with physical restraint use in mechanically ventilated adults. J Crit Care 2016; 31:31–35].
89. Chang LY, Wang KW, Chao YF: Influence of physical restraint on unplanned extubation of adult intensive care patients: A case-control study. Am J Crit Care 2008; 17:408–415; quiz 416
90. Alostaz Z, Rose L, Mehta S, Johnston L, Dale C. Physical restraint practices in an adult intensive care unit: A prospective observational study. J Clin Nurs. 2023 Apr;32(7-8):1163- 1172. doi: 10.1111/jocn.16264. Epub 2022 Feb 22. PMID: 35194883.
91. Cui N, Yang R, Zhang H, Chen D, Wu J, Zhang Y, Ma Y, Jin J. Using the evidence to decision frameworks to formulate the direction and strength of recommendations for adapted guidelines of physical restraints in critical care: A Delphi study. Intensive Crit Care Nurs. 2023 Jun;76:103382. doi: 10.1016/j.iccn.2022.103382. Epub 2023 Jan 11. PMID: 36638685.]
92. Schweickert WD, Pohlman MC, Pohlman AS, et al: Early physical and occupational therapy in mechanically ventilated, critically ill patients: A randomised controlled trial. Lancet 2009; 373:1874–1882
93. Routsi C, Gerovasili V, Vasileiadis I, et al: Electrical muscle stimulation prevents critical illness polyneuromyopathy: A randomized parallel intervention trial. Crit Care 2010; 14:R74
94. Dantas CM, Silva PF, Siqueira FH, et al: Influence of early mobilization on respiratory and peripheral muscle strength in critically ill patients. Rev Bras Ter Intensiva 2012; 24:173–178
95. Denehy L, Skinner EH, Edbrooke L, et al: Exercise rehabilitation for patients with critical illness: A randomized controlled trial with 12 months of follow-up. Crit Care 2013; 17:R156
96. Ali MS, Talwar D, Jain SK: The effect of a short-term pulmonary rehabilitation on exercise capacity and quality of life in patients hospitalised with acute exacerbation of chronic obstructive pulmonary disease. Indian J Chest Dis Allied Sci 2014; 56:13–19 413.
97. Dong ZH, Yu BX, Sun YB, et al: Effects of early rehabilitation therapy on patients with mechanical ventilation. World J Emerg Med 2014; 5:48–52
98. Kayambu G, Boots R, Paratz J: Early physical rehabilitation in intensive care patients with sepsis syndromes: A pilot randomised controlled trial. Intensive Care Med 2015; 41:865–874
99. Kho ME, Truong AD, Zanni JM, et al: Neuromuscular electrical stimulation in mechanically ventilated patients: A randomized, shamcontrolled pilot trial with blinded outcome assessment. J Crit Care 2015; 30:32–39
100. Moss M, Nordon-Craft A, Malone D, et al: A randomized trial of an intensive physical therapy program for patients with acute respiratory failure. Am J Respir Crit Care Med 2016; 193:1101–1110
101. Hodgson CL, Bailey M, Bellomo R, et al; Trial of Early Activity and Mobilization Study Investigators: A binational multicenter pilot feasibility randomized controlled trial of early goal-directed mobilization in the ICU. Crit Care Med 2016; 44:1145–1152.
102. Wang T, Zhou D, Zhang Z and Ma P (2021) Tools Are Needed to Promote Sedation Practices for Mechanically Ventilated Patients. Front. Med. 8:744297. doi:10.3389/fmed.2021.744297
103. Jakob S.M., Ruokonen E., Grounds R.M. et al. Dexmedetomidin vs midozalam or propofol for sedation during prolonged mechanical ventilation // JAMA. — 2012. — Vol. 307. — N 11. — P. 1151–1160.
104. Keating G.M., Sheritan M.H., Williamson K.A. Dexmedetomidin: a guide to its use for sedation in the US // Clin. Drug. Investig. — 2012. — Vol. 32. — N 8. — P. 561–567.
105. Yuan X., Wu J., Wmoang Q., Xu M. The antinociceptive effect of systemic ad- ministration of a combination of low-dose tramadol and dexmedetomidine in a rat model of bone cancer pain // Eur. J. Anaesthesiol. — 2014. — Vol. 31. — P. 30–34.
106. Brumett C.M., Hong E.K., Janda A.M. et al. Perineural dexmedetomidine added to roopivacaine for sciatic nerve block in rats prolongs the duration of an- algesia by blocking the
hyperpolarization-activated cation current // Anesthesiol- ogy. — 2011. — Vol. 115. — P. 836– 843.
107. Ugur F., Gilcu N., Boyaci A. Intrathecal infusion therapy with dexmedetomidine- supplemented morphine in cancer pain // Acta. Anaeshesiol. Scand. — 2007. — Vol. 51. — P. 388.
108. Dexdor: public assessment report. London: European Medicines Agency, 2011. Oct.4.
109. Hoy S.M., Keating J.M. Dexmedetomidine: a review of its use for sedation in mechanically ventilated patients in an intensive care setting and for procedural sedation // Drugs. — 2011. — Vol. 71. — N 11. — P. 1481–1501.
110. Li B., Wang H., Wu H., Gao C. Neurocognitive Dysfunction Risk Alleviation With the Use of Dexmedetomidine in Perioperative Conditions or as ICU Sedation Medicine. Volume 94, Number 14, April 2015: 1 – 9.
111. Reede M.S., O’Sullivan K., Bates S. et al. Dexmedetomidin versus galoperidol in delirious, agitated, intubated patients: a randomized open-label trial // Crit. Care. — 2009. — Vol. 13. — N 3. — P. 75–84.
112. Козлов И.А., Кричевский Л.А. Дексмедетомидин для седации кардиохирургических больных // Патология кровообращения и кардиохирургия. 2014. № 3. С. 67-75.
113. Никода В.Б., Бондаренко А.В., Дубов В.А. Клиническое применение дек- смедетомидина у больных после торакоабдоминальных хирургических вмешательств // Анестезиология и реаниматология. — 2014. — №5. — C. 16–21.
114. Никода В.В., Грицан А.И., Еременко А.А. и др. Эффективность и безопасность применения дексмедетомидина для седации больных при проведении продленной ИВЛ в отделениях реанимации и интенсивной терапии // Анестезиология и реаниматология. — 2015. — №5. — C. 47–55.
115. Jörg M., Axel P., Franck M. et al. Practice of sedation and analgesia in German intensive care units: results of a national survey // Critical Care. — 2005. — Vol. 9. — N 2. — P. 117–123.
116. Cormack J.R., Orme R.M., Costello T.G. The role of α2-agonists in neurosurgery // J. Clin. Sci. — 2005. — Vol. 12. — Issue 4. — P. 375–378.
117. Jing Wang, Belley-Coté E., Burry L., Duffett M. et al. Clonidine for sedation in the critically ill: a systematic review and meta-analysis (protocol). Systematic Reviews (2015) 4:154.
118. Mirski M.A., Hemstreet M.K. Critical care sedation for neuroscience patients // J. Neurosurg. Sci. — 2007. — Vol. 261. — P. 16–34.
119. McKeage K., Perry C.M. Propofol: A review of its use in intensive care sedation of adults // CNS Drugs. — 2003. — Vol 17. — P. 235–272.
120. Carson S.S., Kress J.P., Rodgers J.E. et al. A randomized trial of intermittent lorazepam versus propofol with daily interruption in mechanically ventilated patients // Crit. Care Med. — 2006. — Vol. 34. — P. 1326–1332.
121. Barr J., Egan T.D., Sandoval N.F. et al: Propofol dosing regimens for ICU sedation based upon an integrated pharmacokinetic-pharmacodynamic model // Anesthesiology. — 2001. — Vol. 95. — P. 324–333.
122. Riker R.R., Fraser G.L. Adverse events associated with sedatives, analgesics, and other drugs that provide patient comfort in the intensive care unit // Pharmacotherapy, 2005. — Vol. 25 (5 Pt 2). — P. 8S–18S.
123. Walder B., Tramèr M.R., Seeck M. Seizure-like phenomena and propofol: a systematic review // Neurology, 2002. — Vol. 58. — P. 1327–1332.
124. Iyer V.N., Hoel R., Rabinstein A.A. Propofol infusion syndrome in patients with refractory status epilepticus: An 11-year clinical experience // Crit Care Med. — 2009. — Vol. 37.
— P. 3024–3030.
125. Parviainen I., Uusaro A., Kälviäinen R. et al: Propofol in the treatment of refractory status epilepticus // Intensive Care Med. — 2006. — Vol. 32. — P. 1075–1079.
126. Voss L.J., Sleigh J.W., Barnard J.P. et al. The howling cortex: Seizures and general anesthetic drugs // Anesth. Analg. — 2008. — Vol. 107. — P. 1689–1703.
127. Fong J. J., Sylvia I., Barnard J.P. et al. Predictors of mortality in patients with suspected propofol infusion syndrome // Crit Care Med. — 2008. — Vol. 36. — P. 2281–2287.
128. Didrich D.A., Brown D.R. Analytic revewes: Propofol infusion syndrome in ICU //
J. Intensive Care Med. — 2011. — Vol. 26. — P. 59–72.
129. Merz T.M., Regli B., Roten H.U. et al. Propofol infusion syndrome: a fatal case at a low infusion rate // Anesth. Analg. — 2006. —Vol. 103. — P. 1050.
130. Chukwuemeka A., Ko R., Ralf-Edwards A. Short-term low-dose propofol anaesthesia associated with severe metabolic acidosis // Anaesth. Intensive Care. — 2006. —Vol. 34. — P. 651–655.
131. Roberts R.J., Barletta J.F., Fong J.J. et al: Incidence of propofol-related infu- sion syndrome in critically ill adults: A prospective, multicenter study // Crit. Care, 2009. —Vol. 13. — P. 169.
132. Barr J., Zomorodi K., Bertaccini E.J. et al: A double-blind, randomized comparison of i.v.lorazepam versus midazolam for sedation of ICU patients via a pharmacologic model // Anesthesiology, 2001. — Vol. 95. — P. 286–298.
133. Shafer A. Complications of sedation with midazolam in the intensive care unit and a comparison with other sedative regimens // Crit. Care Med. — 1998. — Vol. 26. — P. 947–956.
134. Swart E.L., Zuideveld K.P., de Jongh J. et al: Population pharmacodynamics modelling of lorazepam- and midazolam-induced sedation upon long-term continuous infusion in critically ill patients // Eur. J. Clin. Pharmacol. — 2006. — Vol. 62. — P. 185–194.
135. Swart E.L., de Jongh J., Zuideveld K.P. et al: Population pharmacokinetics of lorazepam and midazolam and their metabolites in intensive care patients on continuous veno- venous hemofiltration // Am. J. Kidney Dis. — 2005. —Vol. 45. — P. 360–371.
136. Swart E.L., Zuideveld K.P., de Jongh J. et al: Comparative population pharmacokinetics of lorazepam and midazolam during long-term continuous infusion in critically ill patients // Br. J. Clin. Pharmacol. — 2004. —Vol. 57. — P. 135–145.
137. Ariano R.E.,Kassum D.A., Aronson K.J. Comparison of sedative recovery time after midazolam versus diazepam administration // Crit. Care Med. — 1994. — Vol. 22. — P. 1492– 1496.
138. Garcia R, Salluh JIF, Andrade TR, Farah D, da Silva PSL, Bastos DF, Fonseca MCM. A systematic review and meta-analysis of propofol versus midazolam sedation in adult intensive care (ICU) patients. J Crit Care. 2021 Aug;64:91-99. doi: 10.1016/j.jcrc.2021.04.001. Epub 2021 Apr 6. PMID: 33838522.
139. Buckley MS, Smithburger PL, Wong A, Fraser GL, Reade MC, Klein-Fedyshin M, et al. Dexmedetomidine for facilitating mechanical ventilation extubation in difficult-to-wean ICU patients: systematic review and meta-analysis of clinical trials. J Intensive Care Med. Jul. 2020;6:885066620937673. https://doi.org/10.1177/0885066620937673
140. Chen P, Jiang J, Zhang Y, Li G, Qiu Z, Levy MM, et al. Effect of dexmedetomidine on duration of mechanical ventilation in septic patients: a systematic review and meta-analysis. BMC Pulm Med. 2020;20(1):42. https://doi.org/10.1186/s12890-020-1065-6.
141. Hughes CG, Mailloux PT, Devlin JW, Swan JT, Sanders RD, Anzueto A, Jackson JC, Hoskins AS, Pun BT, Orun OM, Raman R, Stollings JL, Kiehl AL, Duprey MS, Bui LN,
O'Neal HR Jr, Snyder A, Gropper MA, Guntupalli KK, Stashenko GJ, Patel MB, Brummel NE, Girard TD, Dittus RS, Bernard GR, Ely EW, Pandharipande PP; MENDS2 Study Investigators. Dexmedetomidine or Propofol for Sedation in Mechanically Ventilated Adults with Sepsis. N Engl J Med. 2021 Apr 15;384(15):1424-1436. doi: 10.1056/NEJMoa2024922. Epub 2021 Feb 2. PMID: 33528922; PMCID: PMC8162695
142. Heybati K, Zhou F, Ali S, Deng J, Mohananey D, Villablanca P, Ramakrishna H. Outcomes of dexmedetomidine versus propofol sedation in critically ill adults requiring mechanical ventilation: a systematic review and meta-analysis of randomised controlled trials. Br J Anaesth. 2022 Oct;129(4):515-526. doi: 10.1016/j.bja.2022.06.020. Epub 2022 Aug 10.
143. Shruti B. Patel and John P. Kress. Sedation and Analgesia in the Mechanically Ventilated Patient. // Am. J. Resp. and Crit. Care Med. — 2012. — Vol. 185. — N 5. — P. 486– 497.
144. Zhou Y, Jin X, Kang Y, et al. Midazolam and propofol used alone or sequentially for long-term sedation in critically ill, mechanically ventilated patients: A prospective, randomized study. Crit Care 2014; 18:R122.
145. Casault C, Soo A, Lee CH, et al. Sedation strategy and ICU delirium: a multicentre, population-based propensity score-matched cohort study. BMJ Open 2021;11:e045087. doi:10.1136/ bmjopen-2020-045087.
146. Huey-Ling L, Chun-Che S, Jen-Jen T, et al: Comparison of the effect of protocol- directed sedation with propofol vs. Midazolam by nurses in intensive care: Efficacy, haemodynamic stability and patient satisfaction. J Clin Nurs 2008; 17:1510–1517.
147. . Mesnil M, Capdevila X, Bringuier S, et al: Long-term sedation in intensive care unit: A randomized comparison between inhaled sevoflurane and intravenous propofol or midazolam. Intensive Care Med 2011; 37:933–941.
148. Jakob SM, Ruokonen E, Grounds RM, et al; Dexmedetomidine forLong-Term Sedation Investigators: Dexmedetomidine vs midazolam or propofol for sedation during prolonged mechanical ventilation: Two randomized controlled trials. JAMA 2012; 307:1151–1160
149. Srivastava VK, Agrawal S, Kumar S, et al. Comparison of dexmedetomidine, propofol and midazolam for short-term sedation in postoperatively mechanically ventilated neurosurgical patients. J Clin Diagn Res 2014; 8:GC04GC07.
150. Kawazoe Y, Miyamoto K, Morimoto T, Yamamoto T, Fuke A, Hashimoto A, et al. Effect of dexmedetomidine on mortality and ventilator-free days in patients requiring mechanical ventilation with sepsis a randomized clinical trial. JAMA 2017;317:1321–8. 27.
151.. Reade MC, Eastwood GM, Bellomo R, Bailey M, Bersten A, Cheung B, et al. Effect of dexmedetomidine added to standard care on ventilator-free time in patients with agitated delirium: a randomized clinical trial. JAMA 2016;315:1460–8].
152. Farina N, Alaniz C. Reconsidering Dexmedetomidine for Sedation in the Critically Ill: Implications of the SPICE III Trial. Ann Pharmacother. 2020 May;54(5):504-508. doi: 10.1177/1060028019890672. Epub 2019 Nov 19. PMID: 31744312.
153. Møller MH, Alhazzani W, Lewis K, Belley-Cote E, Granholm A, Centofanti J, McIntyre WB, Spence J, Al Duhailib Z, Needham DM, Evans L, Reintam Blaser A, Pisani MA, D'Aragon F, Shankar-Hari M, Alshahrani M, Citerio G, Arora RC, Mehta S, Girard TD, Ranzani OT, Hammond N, Devlin JW, Shehabi Y, Pandharipande P, Ostermann M. Use of dexmedetomidine for sedation in mechanically ventilated adult ICU patients: a rapid practice guideline. Intensive Care Med. 2022 Jul;48(7):801-810. doi: 10.1007/s00134-022-06660-x. Epub 2022 May 19. PMID: 35587274.]
154. Mulkey MA, Everhart DE. Sedation selection to reduce delirium risk: Why dexmedetomidine may be a better choice. J Am Assoc Nurse Pract. 2020 Jan 16;33(4):266- 270. doi: 10.1097/JXX.0000000000000364. PMID: 31972787].
155. Nelson KM, Patel GP, Hammond DA. Effects from continuous infusions of dexmedetomidine and propofol on hemodynamic stability in critically ill adult patients with septic shock. J Intensive Care Med 2018. https://doi.org/10.1177/ 0885066618802269. 45. Chang Y-F, Chao A, Shih P-Y, et al. Comparison of dexmedetomidine versus propofol on hemodynamics in surgical critically ill patients. J Surg Res 2018;228: 194–200].
156.. Chang Y-F, Chao A, Shih P-Y, et al. Comparison of dexmedetomidine versus propofol on hemodynamics in surgical critically ill patients. J Surg Res 2018;228: 194–200
157. Owusu KA, Kurczewski L, Armahizer MJ, Zichichi A, Maciel CB, Heavner MS. DEXmedetomidine compared to PROpofol in NEurocritical Care [DEXPRONE]: A multicenter retrospective evaluation of clinical utility and safety. J Crit Care. 2020 Dec;60:79-83. doi: 10.1016/j.jcrc.2020.07.021. Epub 2020 Jul 24. PMID: 32769007
158. Wang G, Niu J, Li Z, Lv H, Cai H. The efficacy and safety of dexmedetomidine in cardiac surgery patients: a systematic review and meta-analysis. PLoS One. 2018;13(9):e0202620. https://doi. org/10.1371/journal.pone.0202620.
159. Lin Y, He B, Chen J, Wang Z. Can dexmedetomidine be a safe and efficacious sedative agent in post-cardiac surgery patients? A meta-analysis. Crit Care. 2012; 16(5):R169
160. Brock L. Dexmedetomidine in Adult Patients in Cardiac Surgery Critical Care: An Evidence-Based Review. AACN Adv Crit Care. 2019 Fall;30(3):259-268. doi: 10.4037/aacnacc2019888. PMID: 31462522.
161. Maldonado JR, Wysong A, van der Starre PJ, et al. Dexmedetomidine and the reduction of postoperative delirium after cardiac surgery. Psychosomatics. 2009;50(3):206-217.
162. Djaiani G, Silverton N, Fedorko L, et al. Dexmedetomidine versus propofol sedation reduces delirium after cardiac surgery: a randomized controlled trial. Anesthesiology. 2016; 124(2):362-368.
163. Jakob SM, Ruokonen E, Grounds RM, et al. Dexmedetomidine vs midazolam or propofol for sedation during prolonged mechanical ventilation: two randomized controlled trials. JAMA. 2012; 307(11):1151-1160
164. Reade MC, Eastwood GM, Bellomo R, et al. Effect of dexmedetomidine added to standard care on ventilator-free time in patients with agitated delirium: a randomized clinical trial. JAMA. 2016; 315(14):1460-1468.
165. Smithburger PL, Patel MK. Pharmacologic Considerations Surrounding Sedation, Delirium, and Sleep in Critically Ill Adults: A Narrative Review. J Pharm Pract. 2019 Jun;32(3):271- 291. doi: 10.1177/0897190019840120. Epub 2019 Apr 7. PMID: 30955461
166. Allam MG. Dexmedetomidine versus midazolam for sedation of critically ill patients on noninvasive mechanical ventilation. Ain-Shams J Anaesthesiol 2016;9(2):178–185. DOI: 10.4103/1687- 7934.179910.
167. Huang Z, Chen YS, Yang ZL, Liu JY. Dexmedetomidine versus midazolam for the sedation of patients with noninvasive ventilation failure. Intern Med 2012;51(17):2299–2305. DOI: 10.2169/ internalmedicine.51.7810
168. Karim HM, Šarc I, Calandra C, Spadaro S, Mina B, Ciobanu LD, Gonçalves G, Caldeira V, Cabrita B, Perren A, Fiorentino G, Utku T, Piervincenzi E, El-Khatib M, Alpay N, Ferrari R, Abdelrahim ME, Saeed H, Madney YM, Harb HS, Vargas N, Demirkiran H, Bhakta P, Papadakos P, Gómez-Ríos MÁ, Abad A, Alqahtani JS, Hadda V, Singha SK, Esquinas AM. Role of Sedation and Analgesia during Noninvasive Ventilation: Systematic Review of Recent Evidence and Recommendations. Indian J Crit Care Med. 2022 Aug;26(8):938-948. doi: 10.5005/jp-journals- 10071-23950. PMID: 36042773; PMCID: PMC9363803
169. De Hert S.G., van der Linden P.J., Cromheecke S. et al.Cardioprotective properties of sevoflurane in patients undergoing coronary surgery with cardiopulmonary bypass are related to the modalities of its administration // Anesthesiology. — 2004. — Vol. 101. — P. 299–310.
170. Hellstrom J., Owall A., V. Sackey P.V. Cardiac outcome after sevoflurane versus propofol sedation following coronary bypass surgery: a pilot study // ActaAnaesthesiol. Scand. — 2011. —Vol. 55. — P. 460–467.
171. Soro M., Gallego L., Silva V. et al. Sevoflurane and propofol during anaesthesia and the postoperative period in coronary bypass graft surgery: a double- blind randomised study // Eur.
J. Anaesthesiol. — 2012. —Vol. 29. — P. 1–9.
172. Bellgardt M., Bomberg H., Herzog-Niescery J. et al. Survival after long-term isoflurane sedation as opposed to intravenous sedation in critically ill surgical patients // Eur. J. Anaesthesiol. — 2015. — Vol. 32. — P. 1–8.
173. Mesnil M., Capdevila X., Bringuier S. et al. Long-term sedation in intensive care unit: a randomized comparison between ihaled sevoflurane and intravenous propofol or midazolam
// Intensive Care Med. — 2011. —Vol. 37. — P. 933–941.
174. Soro M., Belda F.J., Badenes R., AlcantaraM.J. Use of the AnaConDa (Anestesia Conserving Device) with sevoflurane in critical care patients // Eur. J. Anaesthesiol. — 2004. — Vol. 21 (suppl 32). — Р. 708a .
175. Jerath A, Beattie SW, Chandy T, Karski J, Djaiani G, Rao V, Yau T, Wasowicz M. Volatile-based short-term sedation in cardiac surgical patients: a prospective randomized controlled trial. Crit Care Med 2015;43: 1062-9.
176. Martin J., Heymann A., Basell K. et al. Evidence and consensus-based German guidelines for the management of analgesia, sedation and delirium in intensive care– short version // Ger. Med. Sci. — 2010. — Vol. 8. Doc02.
177. Ha Yeon Kim, Ja Eun Lee, Ha Yan Kim, Jeongmin Kim Volatile sedation in the intensive care unit:A systematic review and meta-analysis Medicine (Baltimore)2017 Dec; 96(49)
178. Meiser A, Volk T, Wallenborn J, Guenther U, Becher T, Bracht H, Schwarzkopf K, Knafelj R, Faltlhauser A, Thal SC et al (2021) Inhaled isofurane via the anaesthetic conserving device versus propofol for sedation of invasively ventilated patients in intensive care units in Germany and Slovenia: an open-label, phase 3, randomised controlled, non-inferiority trial. Lancet Respir Med 9(11):1231–1240.
179. Blondonnet R, Balde A, Zhai R, Pereira B, Futier E, Bazin J-E, et al. (2022) Use of volatile anesthetics for sedation in the ICU during the COVID-19 pandemic: A national survey in France (VOL’ICU 2 study). PLoS ONE 17(12): e0278090. https://doi.org/10.1371/journal.pone.0278090
180. G.L. Fraser, J.W. Devlin, C.P. Worby, W. Alhazzani, J. Barr, J.F. Dasta, et al., Benzodiazepine versus nonbenzodiazepine-based sedation for mechanically ventilated, critically ill adults: a systematic review and meta-analysis of randomized trials, Read. Online: Critical Care Medicine| Society of Critical Care Medicine 41 (9) (2013) S30–S38
181. Jung S, Na S, Kim HB, Joo HJ, Kim J. Inhalation sedation for postoperative patients in the intensive care unit: initial sevoflurane concentration and comparison of opioid use with propofol sedation. Acute Crit Care. 2020 Aug;35(3):197-204. doi: 10.4266/acc.2020.00213. Epub 2020 Aug 10. PMID: 32772035; PMCID: PMC7483012.]
182. Jerath A, Slessarev M. The impact of the coronavirus pandemic on sedation in critical care: volatile anesthetics in the ICU. Curr Opin Crit Care. 2023 Feb 1;29(1):14-18. doi: 10.1097/MCC.0000000000001011. Epub 2022 Dec 9.
183. Буров Н.Е. Представления о механизме анестезиологических и лечебных свойств ксенона // Анестезиология и реаниматология. — 2011. — Vol. 2. — C. 58–62.
184. Стряпко Н.В., Сазонтова Т.Г., Потиевская В.И. и др., Молчанов И.В. Адаптационный эффект многократного применения ксенона // Общая реаниматология. — 2014. — Т. 10. — №2. — Vol. 10 . — С. 50–56.
185. Liu W., Liu Y., Chen H. et al. Xenon preconditioning: molecular mechanis ms and biological effects // Medical. Gas. Research. — 2013. — Vol. 3. — P. 1–5.
186. Молчанов И.В., Потиевская В.И., Пулина Н.Н., Шебзухова Е.Х. Лечение больных с острым коронарным синдромом ингаляциями ксенона // Доктор. Ру. — 2012. — Т. 10. — №78. — С. 35–40.
187. Лахин Р.Е., Андреенко А.А., Власенко А.В., Мартынов Д.В., Лазарев В.В., Овезов А.М., Горбачев В.И., Лейдерман И.Н., Белкин А.А., Фишер В.В., Ломиворотов В.В., Кузьков В.В., Шифман Е.М., Григорьев Е.В., Попов А.С., Магомедов М.А., Ярошецкий А.И. Модифицированный дельфийский анализ положений и критериев качества методических рекомендаций «Седация пациентов в отделениях анестезиологии, реанимации и интенсивной терапии». Вестник интенсивной терапии имени А.И. Салтанова. 2023;(2):45–54. doi:10.21320/1818-474X-2023-2-45-54.
Рекомендуемые статьи
При эндоскопическом исследовании в случае бронхоэктазов в стадии ремиссии выявляется
частично диффузный бронхит I степени воспаления
Активируйте PUSH уведомления в браузер
Отключите PUSH уведомления в браузер
Содержание
Интернет магазин
Популярное
- О нас
- Правовые вопросы
- Политика
обработки персональных
данных EndoExpert.ru - Связаться с нами
- Стать партнером
© 2016-2022 EndoExpert.ru

Вы находитесь в разделе предназначенном только для специалистов (раздел для пациентов по ссылке). Пожалуйста, внимательно прочитайте полные условия использования и подтвердите, что Вы являетесь медицинским или фармацевтическим работником или студентом медицинского образовательного учреждения и подтверждаете своё понимание и согласие с тем, что применение рецептурных препаратов, обращение за той или иной медицинской услугой, равно как и ее выполнение, использование медицинских изделий, выбор метода профилактики, диагностики, лечения, медицинской реабилитации, равно как и их применение, возможны только после предварительной консультации со специалистом. Мы используем файлы cookie, чтобы предложить Вам лучший опыт взаимодействия. Файлы cookie позволяют адаптировать веб-сайты к вашим интересам и предпочтениям.
Я прочитал и настоящим принимаю вышеизложенное, хочу продолжить ознакомление с размещенной на данном сайте информацией для специалистов.









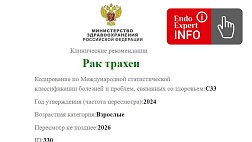

.jpg)


.png)












Комментарии