- Компании
- Takeda. О компании, буклеты, каталоги, контакты
- Olympus. О компании, буклеты, каталоги, контакты
- Boston Scientific. О компании, буклеты, каталоги, контакты
- Pentax. О компании, буклеты, каталоги, контакты
- Fujifilm & R-Farm. О компании, буклеты, каталоги, контакты
- Erbe. О компании, буклеты, каталоги, контакты
- Еще каталоги
- Мероприятия
- Информация
- Обучение
- Классификации
- Атлас
- Quiz
- Разделы
- Пациенту
QR-код этой страницы
Для продолжения изучения на мобильном устройстве ПРОСКАНИРУЙТЕ QR-код с помощью спец. программы или фотокамеры мобильного устройства
Статьи: Эндоскопическое лечение синдрома Линча и семейного риска колоректального рака: Руководство Европейского общества желудочно-кишечной эндоскопии (ESGE)
| Авторы: | ESGE 2019г. |
Анонс:
Данное руководство является официальным заявлением Европейского общества желудочно-кишечной эндоскопии (ESGE). В нем представлен обзор эндоскопического лечения лиц с синдромом Линча и лиц с семейным риском развития колоректального рака.
- ESGE рекомендует проводить наблюдение за пациентами с синдромом Линча в специализированных подразделениях, которые практикуют мониторинг соблюдения и эндоскопических показателей эффективности. Сильная рекомендация, низкое качество доказательств, уровень согласия 100%.
- ESGE рекомендует проводить эндоскопию раньше, чем запланированная процедура наблюдения, если пациент с ЛС имеет симптомы. Сильная рекомендация, низкое качество доказательств, уровень согласия 100%.
- ESGE рекомендует начать колоноскопическое наблюдение в возрасте 25 лет для носителей мутаций MLH1 и MSH2 и в возрасте 35 лет для носителей мутаций MSH6 и PMS2. Сильная рекомендация, умеренное качество доказательств, уровень согласия 100%.
- ESGE рекомендует проводить высококачественную эпиднадзорную колоноскопию каждые 2 года у лиц без симптомов с синдромом Линча. Сильная рекомендация, умеренное качество доказательств, уровень согласия 90%.
- ESGE рекомендует повторить полную колоноскопию в течение 3 месяцев в случае колоноскопии субоптимального качества (плохая подготовка кишечника или неполная процедура). Сильная рекомендация, умеренное качество доказательств, уровень согласия 90%.
- ESGE рекомендует регулярно использовать системы эндоскопии высокой четкости у лиц с синдромом Линча. Сильная рекомендация, высокое качество доказательств, уровень согласия 100%.
- ESGE предполагает, что использование хромоэндоскопии может быть полезным у людей с синдромом Линча, проходящих колоноскопию; однако рутинное использование должно быть сбалансировано с затратами, обучением и практическими соображениями. Слабая рекомендация, умеренное качество данных, уровень согласия 89%.
- ESGE не рекомендует регулярное наблюдение за желудком у лиц с синдромом Линча. Сильная рекомендация, низкое качество доказательств, уровень согласия 100%.
- ESGE предлагает (неинвазивное) тестирование на Helicobacter pylori у лиц с синдромом Линча. Слабая рекомендация, доказательства среднего качества, уровень согласия 90%.
- ESGE не рекомендует регулярное наблюдение за тонкой кишкой у лиц с синдромом Линча. Сильная рекомендация, умеренное качество доказательств, уровень согласия 100%
- ESGE рекомендует определять семейный риск развития колоректального рака как наличие по меньшей мере двух родственников первой степени с колоректальным раком или по меньшей мере одного родственника первой степени с колоректальным раком в возрасте до 50 лет. Сильная рекомендация, умеренное качество доказательств, уровень согласия 92%.
- ESGE рекомендует проводить колоноскопическое наблюдение у родственников первого уровня случаев КРР в семьях, которые соответствуют определению семейного риска развития колоректального рака. Сильная рекомендация, умеренное качество доказательств, уровень согласия 100%.
- ESGE рекомендует 5-летний интервал наблюдения для колоноскопии после нормального высококачественного базового обследования при семейном риске колоректального рака. Сильная рекомендация, низкое качество доказательств, уровень согласия 83%.
- ESGE рекомендует, чтобы последующее наблюдение после удаления полипов у лиц с семейным риском развития колоректального рака следовало руководящим принципам эпиднадзора для населения в целом. Сильная рекомендация, умеренное качество доказательств, уровень согласия 92%.
- ESGE рекомендует начинать колоноскопическое наблюдение в возрасте 40 лет, когда существует семейный риск развития колоректального рака. Сильная рекомендация, умеренное качество доказательств, уровень согласия 92%.

Полный текст статьи:
| Материалы по теме из раздела QuaCol |
| Обзор литературы: Синдром Линча
|
Авторы: Моник Э. ван Леердам 1,2, Викторина Х. Роос 3, Жанин Э. ван Хоофт 3, Франсеск Балагер 4,5, Эвелиен Деккер 3, Михал Ф.
Камински 6,7,8, Эндрю Латчфорд 9,10, Хельмут Нейман 11, Луиджи Ричардьелло 12, Мария Рупиньска 6,7, Жан-Кристоф
Саурин 13, Питер Дж. Танис 14, Аня Вагнер 15, Родриго Ховер 16, Мария Пеллисе 4.5
ОСНОВНЫЕ РЕКОМЕНДАЦИИ
ESGE рекомендует лицам с синдромом Линча
следует следовать в специализированных подразделениях, которые практикуют
мониторинг соответствия и эндоскопических показателей
меры.
Сильная рекомендация, доказательства низкого качества, уровень
соглашение 100%.
Приложения 1с, 2с
Интернет-контент для просмотра по адресу:
https://doi.org/10.1055/a-1016-4977
директива
Ван Леердам Моник Э. и соавт. Эндоскопическое лечение синдрома Линча и семейного риска колоректального рака ... Эндоскопия
1. Введение
Рак ободочной и прямой кишки (CRC) является четвертым наиболее распространенным раком и
вторая по значимости причина смертности от рака в Европе [1].
Хотя большинство CRC является спорадическим, исследования близнецов показали
что до 35% случаев CRC имеют семейный компонент [2].
В 2–5% случаев CRC выявлено генетическое происхождение
[3]. Наиболее распространенный наследственный синдром CRC вызван
конституционально-патогенный вариант в одном из несоответствий ДНК
ремонтные (MMR) гены (MLH1, MSH2, MSH6, PMS2) или 3'-конец
ген EpCAM; это также известно как синдром Линча (LS) и
ранее назывался наследственным не полипозным колоректальным
cer (HNPCC) [3]. Среди случаев CRC около 2% -4% вызваны
по LS [4]. Так же как увеличенный риск CRC, люди с LS
имеют более высокий риск развития эндометрия, желудка, малых
рак кишечника, желчных путей, яичников, мочевыводящих путей, мозга и кожи.
Из-за высокого риска рака очень важно, чтобы
клиницисты узнавали людей с ЛС, чтобы
Отдельные управленческие решения как для пациента, так и для его
рисковать членами семьи. Случаи CRC, связанные с синдромом полипоза
Дромы обсуждаются в отдельном руководстве [5].
Тем не менее, для большинства случаев CRC с семейным компонентом,
генетическое происхождение не обнаружено. Риск CRC в этом гетерогенном
группа лиц варьируется. Фактический риск CRC зависит от
количество пострадавших членов семьи и возраст на момент постановки диагноза, в соответствии с симптомами синдрома Линча,
любого пострадавшего члена семьи [6], и наблюдение должно быть
перечислил этим лицам на основе их предполагаемого риска CRC.
В этом руководстве представлен обзор эндоскопического
возраст людей с LS. Кроме того, мы стремились
определить семейный риск CRC для лиц с высоким риском
КПР, поэтому наблюдение должно быть предложено. поскольку
стратегии эндоскопического лечения ЛС и семейного риска
CRC широко варьируются, мы стремились достичь консенсуса среди европейских
эксперты с помощью процесса Delphi.
2 метода
ESGE заказал это Руководство (Руководящий комитет
председатель JvH) и назначил руководителя Руководства (MvL), который
перечислил авторов для участия в разработке проекта
Мент. Ключевые вопросы были подготовлены координирующим
ИСТОЧНИК И ОБЛАСТЬ ПРИМЕНЕНИЯ
Данное Руководство является официальным заявлением Европейского
Общество желудочно-кишечной эндоскопии (ESGE). Это обеспечивает
обзор эндоскопического управления
люди с синдромом Линча и люди с семейными
Риск колоректального рака. Оценка по рекомендациям
Оценка, развитие и оценка (GRADE)
система была принята, чтобы определить силу рекомендации
Даты и качество доказательств.
СОКРАЩЕНИЯ
Частота обнаружения аденомы
CE хромоэндоскопия
Доверительный интервал CI
CRC колоректальный рак
Компьютерная томография
ESGE Европейское общество желудочно-кишечной эндоскопии
Родственник первой степени
FIT фекальный иммунохимический тест
Оценка оценок рекомендаций,
Разработка и оценка
Коэффициент риска для персонала
HNPCC наследственный не полипозный колоректальный рак
Синдром Л.С. Линча
MMR несоответствие ремонт
МРТ магнитно-резонансная томография
ИЛИ отношение шансов
RR относительный риск
SIR стандартизированный коэффициент заболеваемости
Эндоскопия видео капсулы VCE
WLE эндоскопия белого света
ESGE рекомендует начать колоноскопическое наблюдение на
возраст 25 лет для носителей мутаций MLH1 и MSH2 и
возраст 35 лет для носителей мутаций MSH6 и PMS2.
Сильная рекомендация, доказательства среднего качества, уровень
соглашения 100%.
ESGE рекомендует рутинное использование высокой четкости
системы эндоскопии у лиц с синдромом Линча.
Сильная рекомендация, высокое качество доказательств, уровень
соглашение 100%.
ESGE предполагает, что использование хромоэндоскопии может быть полезным
Подходят людям с синдромом Линча, перенесшим
noscopy; Однако рутинное использование должно быть сбалансировано
затраты, обучение и практические соображения.
Слабая рекомендация, доказательства среднего качества, уровень
согласие 89%.
ESGE рекомендует определение семейного риска колоректального
рак как наличие как минимум двух родственников первой степени
с колоректальным раком или по крайней мере одним родственником первой степени
с колоректальным раком в возрасте до 50 лет.
Сильная рекомендация, доказательства среднего качества, уровень
соглашения 92%.
ESGE рекомендует колоноскопическое наблюдение в первой степени
родственники больных колоректальным раком в семьях, которые выполняют
определение семейного риска колоректального рака.
Сильная рекомендация, доказательства среднего качества, уровень
соглашения 100%.
Ван Леердам Моник Э. и соавт. Эндоскопическое лечение синдрома Линча и семейного риска колоректального рака ... Эндоскопия
команда (MvL и VR), а затем одобрен другой группой
члены. Координационная группа учредила целевую группу
группы, каждая со своим лидером и разделили ключевые темы
среди этих целевых групп (Приложение 1; см. только
материал).
Процесс разработки Руководства включал телефон
конференции, встречи, онлайн и личные встречи
среди членов с июля 2018 года по июль 2019 года.
были выполнены в MEDLINE, Embase и Cochrane
Библиотека. Статьи были выбраны через заголовок и реферат
скрининг с последующим полнотекстовым скринингом. Результаты
поиск был представлен всем членам группы и консенсус
заявления были созданы.
Уровни доказательств и сильные стороны рекомендаций были
с использованием оценки классификации рекомендаций,
Система развития и оценки (GRADE) [7]. Дальнейшие подробности
по методологии ESGE руководящих принципов
в другом месте [8].
Поскольку литература о семейном риске колоректального рака и LS
ограниченный, процесс Delphi, обычно состоящий из двух раундов, был
используется для получения консенсуса [9]. Все участники, кроме
Исследователи попросили завершить онлайн Delphi
вопросник изолированно, и ответы были анонимно
не позволять участникам влиять друг на друга [10]. В
каждый раунд участники должны были оценить все заявления
с их уровнем согласия, используя шкалу Лайкерта из семи пунктов:
«Совершенно согласен», «Совершенно согласен», «Согласен», «Ни то, ни другое
согласен, не согласен »,« Не согласен »,« Совершенно не согласен »или« Очень
категорически не согласен »[11]. Если заявление не было в пределах их
область знаний, участники могут отказаться. Во-вторых, особенно
штаны спросили, было ли утверждение ясно, и имел
возможность вносить предложения по улучшению. После
Дельфи раунд, все заявления были обсуждены и скорректированы, если
необходимо, во время личной встречи. Консенсус был
достигнуто, когда ≥80% членов группы проголосовали либо
«Совершенно согласен», «Совершенно согласен» или «Согласен» во время
Второй раунд Delphi. Третий и четвертый раунды Delphi были
ganized только для заявлений, касающихся передовых изображений.
В июле 2019 года проект, подготовленный MvL и VR, был отправлен
все участники группы. После согласия всех членов группы
рукопись была рецензирована членом
Совета управляющих ESGE и внешнего рецензента, и был
отправлены для дальнейших комментариев в национальные общества ESGE и
отдельные участники. После этого он был передан на эндоскопию
для публикации. Это руководство было выпущено в 2019 году и будет
рассматривается для обновления в 2024 году. Любые промежуточные обновления будут
отметил на веб-сайте ESGE: http://www.esge.com/esge-guide-
lines.html.
3 синдром Линча
3.1 Справочная информация
Эта часть Руководства ориентирована на лиц с ЛС,
определяется как те, которые имеют конституциональный патогенный вариант в
один из генов восстановления несоответствия (MMR) MLH1, MSH2, MSH6,
PMS2 или делеции в 3'-области гена EpCAM. Ключ
для выявления LS среди случаев CRC проводится тестирование на MMR
дефицит опухолевой ткани, и это в настоящее время стратегия
выбора у всех лиц, диагностированных в возрасте до 70 лет
с CRC [12).
По оценкам, на уровне населения распространенность
LS составляет 1 из 279 (95% доверительный интервал [CI] 192–493) [13]. показываемое
люди с LS подвергаются риску раннего CRC и имеют высокую
совокупный риск жизни КРК в течение жизни от 15% до 70%
в возрасте 70 лет [14–18]. Последовательность аденома - карцинома кажется
чтобы быть ускоренным, с сообщенным временем задержки всего 35
месяцев по сравнению с 10–15 годами в спорадических CRC [17].
Предотвратить развитие CRC или обнаружить CRC на ранней стадии
На этапе колоноскопического надзора при ЛС необходимо. Обычный цвет
носкопическое наблюдение у лиц с ЛС значительно снижено
CRC заболеваемость и связанная с ней смертность более чем на 50% [18,
19]. Люди с ЛС также имеют более высокий риск других желудочно-кишечных
злокачественные новообразования яичек, для которых может быть проведено эндоскопическое наблюдение
опция.
3.2 Колоноскопическое наблюдение
3.2.1 Стандарты качества
Колоноскопия снижает частоту и смертность от КРР
[18–21] у лиц с LS.Post-колоноскопией CRC являются
оштрафован Всемирной организацией эндоскопии за раковые заболевания
после колоноскопии, при которой рак не диагностируется, и
охватывают как интервальный рак, так и не интервальный рак
[22]. Интервальные раки - это те, которые обнаружены до следующего
рекомендуется надзорное обследование. Неинтервальный рак
подразделяются на раковые заболевания, обнаруженные в (тип A) или после (тип
Б) рекомендуемый интервал наблюдения или когда нет последующего
интервал наблюдения рекомендован (тип С), до 10 лет
после колоноскопии.
Эпидемиологические исследования сообщили, что совокупный
Уровень CRC в 70 лет среди лиц с LS
Колоноскопический надзор может достигать 46% среди MLH1,
35% среди MSH2, 20% среди MSH6 и 10% среди PMS2
патогенные носители мутаций [15]. Некоторые авторы постулат
что некоторые постколоноскопические CRC в LS могут появиться из
MMR-дефицитные очаги крипты без полипоидной картины роста
и поэтому может быть трудно обнаружить с помощью колоноскопии [23].
Однако ретроспективные описательные исследования, оценивающие
колоноскопия CRC показала ассоциации с неполным
нация [24–28], недостаточная подготовка кишечника [24–27,29],
и возможна неполная резекция поражений [24,30]. Больше-
более, рекомендации по интервалу между колоноскопиями
не всегда соблюдаются, и несоблюдение
РЕКОМЕНДАЦИЯ
ESGE рекомендует лицам с синдромом Линча
следует следовать в специализированных подразделениях, которые практикуют
мониторинг соответствия и эндоскопических показателей
меры.
Сильная рекомендация, доказательства низкого качества, уровень
соглашение 100%.
Ван Леердам Моник Э. и соавт. Эндоскопическое лечение синдрома Линча и семейного риска колоректального рака ... Эндоскопия
директива
сообщается как еще один важный фактор в постколоноскопии CRC
[26–28,31–38].
Кроме того, высокий процент случаев колоректальной неоплазии (12% -
74%) были зарегистрированы в нескольких спинах колоноскопии
исследования [39–46]. Таким образом, можно сделать вывод, что высокое качество
Стандарты колоноскопии не всегда соблюдаются у отдельных лиц.
с общ. Тем не менее, данные, касающиеся ключевых показателей эффективности
Число пациентов для колоноскопии у лиц с ЛС ограничено [24–30].
Соблюдение рекомендуемых интервалов наблюдения
важный. Некоторые исследования показали, что предоставление
генетическое тестирование [37] и внедрение стандартизированных
программы наблюдения [38,47] улучшают соблюдение. Национальное
gistries, связанные с программами наблюдения, предлагающими регулярные
эндоскопическое наблюдение с использованием напоминаний шоу
высокие показатели соответствия [26–28,31–36,38].
По этим причинам лицам с ЛС следует следовать в
специализированные подразделения (национальные реестры, центры генетического консультирования,
или онкологические центры высокого риска), где эндоскопическое наблюдение
рекомендации отслеживаются с целью улучшения
и для проверки качества программы наблюдения. Это
Следует подчеркнуть, что эпиднадзор за колоноскопией в
люди с LS должны соответствовать критериям качества ESGE для
носкопия [48,49].
3.2.2 Симптоматические индивидуумы LS
В данном Руководстве обсуждаются интервалы наблюдения для асимпто-
индивидуумы с ЛС. Однако лица, имеющие специфические
жалобы, такие как анемия, ректальная кровопотеря или брюшной полости
боль должна быть осмотрена гастроэнтерологом и эндоскопом
может быть указано в более ранний момент времени.
3.2.3 Колоноскопическое наблюдение: возраст начала
Соответствующий возраст, чтобы начать наблюдение, чтобы достичь
оптимальная эффективность не была установлена в клинических испытаниях. Таким образом,
начальный возраст оценивается на основе индивидуального риска
развития прогрессирующих аденом и CRC в определенном возрасте. Это
Было продемонстрировано, что как риск развития
CRC начала, а также общий риск CRC зависят от MMR
участие гена [14,16,28,50–53]. В недавнем международном
Спективное когортное исследование, включающее более 3000 незатронутых мутаций
носителей, совокупная частота CRC составила 46%, 43%, 15% и
0% для носителей патогенных MLH1, MSH2, MSH6 и PMS2
варианты, соответственно, после среднего периода наблюдения 7,8 лет
[16]. Следует отметить, что носители патогенных вариантов MSH6 и
Ген PMS2 не имел CRC до 40 лет. Другие исследования
подтвердили, что возраст появления CRC у носителей патогенный
варианты генов MSH6 и PMS2 откладывались на 10 лет
по сравнению с носителями патогенных вариантов MLH1 и MSH2
[52,53], с очень низким риском CRC в возрасте до 30 лет [51,
52]. Точно так же был крайне низкий риск развития
венозная аденома (среднее число опухолевых поражений в возрасте
20–29 лет, 1,3 ± 0,5) или CRC (1% за 5 лет) до достижения возраста
30 для носителей патогенных вариантов MLH1 и MSH2
гены [52,53], с очень большими числами, необходимыми для скрининга
предотвратить одну смерть CRC [54]. Важно принять во внимание
Кроме того, во избежание предвзятости, индексные случаи не
включены в ретроспективные и проспективные когортные исследования.
В основном среди индексных случаев носители с патогенным MMR варьируют
Iant может представлять с CRC в более молодом возрасте, чем предложено
стартовый возраст для наблюдения. Тем не менее, с учетом рака
риски и очень большие цифры, необходимые для выявления
одно поражение при колоноскопии [17,54] кажется оправданным отложить
начало колоноскопического наблюдения до возраста не менее 25 лет
лет для носителей патогенных вариантов MLH1 и MSH2
ген и 35 лет для носителей патогенных вариантов
Гены MSH6 и PMS2. Резюме доказательств предоставляется
в таблицах 1 (Приложение 2, только дополнительный онлайн-материал).
Нет никаких доказательств того, что колоноскопия до возраста
самый молодой диагноз CRC в семье является полезным; Однако это
может быть рекомендовано в индивидуальном порядке после полного консультирования
человек о рисках и преимуществах процедуры.
3.2.4 Интервал колоноскопического наблюдения
Рандомизированные контролируемые испытания для наблюдения в мутации LS
перевозчики недоступны; поэтому мы должны полагаться на
наблюдательные исследования, которые косвенно
РЕКОМЕНДАЦИЯ
ESGE рекомендует высококачественный эпиднадзор за колоноскопией
Пы каждые 2 года у бессимптомных лиц с Линчем
синдром.
Сильная рекомендация, доказательства среднего качества,
уровень согласия 90%.
РЕКОМЕНДАЦИЯ
ESGE рекомендует повторить полную колоноскопию
в течение 3 месяцев в случае колоноскопии
оптимальное качество (плохая подготовка кишечника или неполное
процедура).
Сильная рекомендация, доказательства среднего качества,
уровень согласия 90%.
РЕКОМЕНДАЦИЯ
ESGE рекомендует выполнить эндоскопию раньше
чем запланированная процедура наблюдения, если человек
с LS это симптоматично.
Сильная рекомендация, доказательства низкого качества, уровень
соглашение 100%.
РЕКОМЕНДАЦИЯ
ESGE рекомендует начать колоноскопический надзор в
возраст 25 лет для носителей мутаций MLH1 и MSH2
и в возрасте 35 лет для мутации MSH6 и PMS2
носители.
Сильная рекомендация, доказательства среднего качества,
уровень согласия 100%.
Ван Леердам Моник Э. и соавт. Эндоскопическое лечение синдрома Линча и семейного риска колоректального рака ... Эндоскопия
сравнить показатели после колоноскопии CRC и их стадии распределения
с разными интервалами наблюдения. Краткое изложение этих
исследования предоставляются в таблице 2s. CRCs после колоноскопии были
служил независимо от 1-, 2- или 3-летнего колоноскопического обследования-
интервал копий, используемый в каждом из опубликованных исследований [14–17,28,
50-55]. В недавнем большом международном исследовании с участием 2747
носители патогенных вариантов MLH1, MSH2 или MSH6
гены, сообщающие о более чем 16 000 колоноскопий, без различий
в постколоноскопии частота CRC или распределение стадии CRC были
наблюдается среди трех различных политик наблюдения, в
Реестры LS из Германии (с интервалом в 1 год), Нидерландов
(Интервал 1–2 года) и Финляндия (интервал 2–3 года) [35]. Мех-
более того, в нескольких исследованиях среднее время от даты
колоноскопии с диагнозом CRC был между 24 и 36
месяцев, которые могут поддерживать интервалы, превышающие 1 год [31,
32,56]. Следует отметить, что общая выживаемость у пациентов с диагнозом
с постколоноскопией CRC в рамках программ наблюдения были
отлично и превысил 90% [24,27,32,36,56,57].
Как данные о качестве колоноскопии в исследованиях, сравнивающих
различные интервалы наблюдения были ограничены, как и данные о
соблюдение установленных интервалов наблюдения и доказательств
для стратифицированного подхода к различным конституционным пато
генные варианты в генах MMR, кажется оправданным предложить
равномерный 2-летний интервал независимо от патогенного варианта.
Доказательства повышенного риска метахронного CRC в
лица с LS после удаления полипа или резекции CRC не
однозначный [31,32,35,58]. В кабинете из Нидерландов
ни наличие аденомы, ни ее характеристики
были связаны с повышенным риском для CRC [32]. Тем не мение,
Энгель и соавт. показали, что распространенная аденома при индексе
копия была на самом деле связана с более высоким совокупным показателем CRC
денс [35]. Кроме того, предполагалось, что неполное удаление
аденомы может быть значительным фактором риска
CRC после колоноскопии [24]. В других исследованиях риск развития
метахронная аденома или CRC после операции по поводу CRC
(сегментальная или субтотальная колэктомия) была относительно низкой, обеспечивая
это наблюдение проводилось в течение 2 лет [27,58]. Ждите-
дальнейшие доказательства сокращают интервалы наблюдения
чем 2 года следует рассматривать только в особых ситуациях.
В настоящее время ограниченные данные поддерживают более длительный интервал наблюдения
для носителей патогенного варианта MSH6 и PMS2, которые делают
нести более низкий совокупный уровень CRC. Это было предложено
что PMS2-ассоциированные CRC действительно имеют отличную биологию опухолей,
который может поддерживать более длительный интервал наблюдения для носителей PMS2
Если данные подтвердятся [59].
Высокое качество экспертизы считается одним из ключевых
факторы оптимальной эффективности эпиднадзора за колоноскопией,
и, следовательно, колоноскопии наблюдения у лиц с LS
должны соответствовать критериям качества ESGE для колоноскопии [24,48,
49] (см. Также выше). Perrod et al. оценили
грамм, который назначил интервалы наблюдения на основе качества
предыдущей колоноскопии (чистота, полнота и
использование хромоэндоскопии) и продемонстрировали улучшение
по качеству, снижение пост-колоноскопии CRC и увеличение
выявление плоской дисплазии [60]. Так что когда субоптимальный кишечник
подготовка (Бостонская шкала подготовки кишечника <2 в одном из
сегменты толстой кишки) или процедура не завершена,
Носка должна быть повторена в течение 3 месяцев до ввода
2-летний период наблюдения.
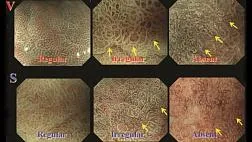
3.2.5 Колоноскопическое наблюдение: расширенная визуализация
методы
В литературе семь исследований сравнивали индигокармин
хромоэндоскопия с эндоскопией белого света (WLE) у
проб с LS (Table3As) [39–41,44,45].
Три небольших одноцентровых исследования с параллельным дизайном
и эндоскопы стандартной четкости показали, что
Мендоскопия превосходила WLE, сообщая об аденоме WLE
частота промахов составляет от 61% до 74% [39,40,45]. Совсем недавно
другое многоцентровое исследование, в котором второе
проход был выполнен другим гастроэнтерологом, снова
продемонстрировал превосходство хромоэндос
скопировать поверх стандартного разрешения WLE, сообщив об отсутствии аденомы
показатель 52% [41]. Тем не менее, все эти исследования являются методологическими
ошибочно, так как спина к спине влечет за собой то, что второй
проход всегда делается с помощью хромоэндоскопии, которая может иметь
привело к переоценке эффекта хромоэндоскопии
о WLE.
Доступны три параллельных испытания с контрольной рукой [44,61,
62]. Небольшое параллельное исследование с двумя руками, а именно WLE
снижается путем интенсивного осмотра более 20 минут или WLE-
хромоэндоскопия, не показала значительных различий в адено-
мисс скорость между двумя стратегиями [44]. Недавно два
largemulticenterrandomizedparalleltrialsdidnotdemonstrate
польза для хромоэндоскопии по сравнению с WLE [61,62].
Голландское исследование у 246 человек с конституциональным патогенным
варианты в одном из генов MMR не показали различий в нео
Уровень обнаружения плазмы между хромоэндоскопией и WLE, оба
при базовой колоноскопии (27% против 30% соответственно, P =
0,56), а также через 2 года колоноскопии (26% против
28% соответственно, P = 0,81) [61]. Многоцентровая неполноценность
Испанское исследование на 256 носителях с конституциональным патогенным
вариант в одном из генов MMR показал столь же высокую
скорости обнаружения по номе (ADR), для WLE и хроматографии высокого разрешения
Мендоскопия (ADR 28,1%, 95% CI 21,1% -36,4% против 34,4%,
95% ДИ 26,4% -43,3% соответственно; P = 0,28) [62]. Тем не мение,
РЕКОМЕНДАЦИЯ
ESGE рекомендует рутинное использование высокой четкости
системы эндоскопии у лиц с синдромом Линча.
Сильная рекомендация, высокое качество доказательств, уровень
соглашение 100%.
РЕКОМЕНДАЦИЯ
ESGE предполагает, что использование хромоэндоскопии может иметь
польза в людях с проходящим синдромом Линча
колоноскопии; Однако рутинное использование должно быть сбалансировано
против затрат, обучения и практических соображений.
Слабая рекомендация, умеренное качество доказательств, уровень
соглашения 89%.
Ван Леердам Моник Э. и соавт. Эндоскопическое лечение синдрома Линча и семейного риска колоректального рака ... Эндоскопия
директива
наблюдалась нестатистически значимая тенденция в отношении
скорость плоских аденом в пользу панколонийного хромо-
Доскопия (24,2%, 95% ДИ 17,1% - 32,6%) по сравнению с WLE
(14,8%, 95% ДИ от 9,2% до 22,2%) (р = 0,06). Примечательно, что только на высоком уровне
Детекторы-эндоскописты участвовали как в исследованиях, так и в
Второй - все эндоскопы были высокого разрешения.
Виртуальная хромоэндоскопия превосходила WLE в двух
сопутствующие исследования у лиц с ЛС (Table3Bs) [42,43]. На
с другой стороны, виртуальная хромоэндоскопия уступала
основанная на хромоэндоскопии в двух параллельных исследованиях [40,63].
Таким образом, в настоящее время роль виртуальной хромоэндоскопии в
наблюдение за лицами с ЛС еще не установлено.
Комментарий: Утилита хромоэндоскопии. За последние 10 лет
частота выявления колоректальных повреждений постепенно увеличивается,
из-за улучшений в эндоскопической технологии, а также
внедрение качественных показателей при скрининге
копия. Дополнительный эффект хромоэндоскопии по сравнению с WLE для
обнаружение аденомы в ЛС, возможно, было переоценено до
причина методологических ограничений в большинстве предыдущих исследований
х годов. Фактически, в параллельных исследованиях ADR WLE варьировались от 9%
до 23%, и в двух недавних параллельных исследованиях АДР WLE варьировались
с 26% до 28%. Это может означать, что тщательный осмотр
эндоскопистами детекторов высокого уровня и использованием
Эти эндоскопы могут перевесить положительный эффект
хромоэндоскопии. Тем не менее, для детектора низкого уровня эндо-
кописты или когда высокая четкость недоступна, использование
Мендоскопия до сих пор остается желательной.
3.3 Наблюдение за желудком
Люди с LS имеют совокупный риск в течение жизни
от 0,7% до 13% развивающегося рака желудка [64]. Данные
показать тенденцию к увеличению распространенности рака желудка
для носителей патогенных вариантов генов MLH1 или MSH2
по сравнению с носителями патогенного варианта MSH6
ген [64]. Большинство случаев рака желудка были диагностированы в
лица старше 45 лет, средний возраст которых колеблется
от 55 до 64 лет (общий диапазон 27–85) [65–68]. Среди всех
у лиц с LS, у которых развился рак желудка, 0–31% имели
семейный анамнез рака желудка [65–68].
РКИ, оценивающие эффект обследования желудка, отсутствуют.
копье у людей с ЛС, но три обсервационных исследования
были опубликованы [68–70] (табл. 4). В двух ретроспективе
Наблюдательные когортные исследования около 30% людей с
ЛС прошла эзофагогастродуоденоскопию [68,69].
В турецком исследовании 19,1% носителей мутаций имели H. pylori
гастрит, атрофический гастрит или желудочно-кишечная метаплазия [69].
Положительная семейная история не была значительно связана с
с аномальными результатами эзофагогастродуоденоскопии [69].
В голландском исследовании эзофагогастродуоденоскопия показала
рак у трех человек (6,1%), биопсия подтвердила
у 23 (17,4%), кишечная метаплазия у 4 (3,0%) и нет
патологические или эндоскопические нарушения у 97 (73,5%) [68]. из
эти люди с LS, 20% были H. pylori-позитивными [68]. В
нерандомизированное сравнительное финское исследование, единое эзофаго-
гастродуоденоскопия проводилась как на носителях
тогенный вариант в гене MLH1 (средний возраст 49 лет) и
у членов семьи с отрицательной мутацией (средний возраст 51 год)
[70]. У лиц с патогенным вариантом MLH1
ген, инфекция H. pylori наблюдалась у 26%, атрофия у 14%,
и кишечная метаплазия в 14%; эти выводы были похожи на
в контрольной группе [70]. Так что ввиду видимо
ограниченный риск рака желудка у лиц с LS и отсутствием доказательств
о пользе надзора за желудком, такие
Копье обычно не рекомендуется.
Метаанализ, включающий 7 рандомизированных контролируемых исследований в
население показало, что эрадикация H. pylori
Заболеваемость раком желудка на 35% [71]. Кроме того, население
Установлено, что скрининг на H. pylori является экономически эффективным
[72]. Хотя прямых доказательств нет, можно предположить,
что люди с ЛС также выиграют от скрининга H. pylori
и искоренение.
3.4 Тонкокишечное наблюдение
У людей с ЛС кумулятивный риск развития
Рак тонкой кишки в возрасте до 70 лет варьировался от
0,6% (95% ДИ от 0,1% до 1,3%) до 7,2% (95% ДИ от 1,5% до 12,9%) в
представители патогенного варианта гена MLH1 [64]. Существует
100-кратное увеличение риска развития рака тонкой кишки
у лиц, имеющих LS по сравнению с населением в целом
[73]. Заболеваемость раком тонкой кишки у лиц с LS
был самым высоким среди носителей патогенных вариантов MLH1
или гены MSH2 и чаще всего встречаются у мужчин (57–79%) [74–
76]. Средний возраст диагноза варьировал от 39 до 53 лет.
[77-83]. Большинство раковых заболеваний тонкой кишки были обнаружены
в двенадцатиперстной кишке или тощей кишке [77–82] и гистология показала
аденокарцинома в 81–100% случаев [79,81].
Два исследования исследовали использование видео капсулы
эндоскопия (VCE) у бессимптомных носителей патогенного разнообразия
РЕКОМЕНДАЦИЯ
ESGE не рекомендует проводить регулярное обследование тонкой кишки-
копье у лиц с синдромом Линча.
Сильная рекомендация, доказательства среднего качества,
уровень согласия 100%.
РЕКОМЕНДАЦИЯ
ESGE не рекомендует регулярное наблюдение за желудком в
лица с синдромом Линча.
Сильная рекомендация, доказательства низкого качества, уровень
соглашение 100%.
РЕКОМЕНДАЦИЯ
ESGE предлагает (неинвазивное) тестирование на Helicobacter
привратники желудка у лиц с синдромом Линча.
Слабая рекомендация, умеренное качество доказательств, уровень
соглашения 90%.
Ван Леердам Моник Э. и соавт. Эндоскопическое лечение синдрома Линча и семейного риска колоректального рака ... Эндоскопия
муравейник и наблюдаемая распространенность новообразования тонкой кишки 1,5%
и 8,6% [84,85] (табл. 5). В голландском исследовании, в том числе 200
индивидуумы с LS, один пациент был диагностирован с T2N0Mx
рак двенадцатиперстной кишки через 7 месяцев после отрицательного VCE [84]. Другой
Исследование, среди 35 человек с ЛС, не сообщало о тонкой кишке
раковые заболевания после среднего периода наблюдения 40 месяцев [85]. В дальнейшем-
более 70% людей имели ложноположительные результаты, в результате чего
в ненужных инвазивных вторичных процедурах, таких как баллон
энтероскопия или магнитно-резонансная томография (МРТ) энтероклис
[84]. Во втором исследовании сравнивали VCE с компьютерной томографией.
рафиозный (КТ) энтероклис и показал, что КТ энтероклис пропущен
два из трех случаев неоплазии тонкой кишки [85]. Другая
Исследование показало, что повторение VCE после среднего интервала
2,2 года у 78% пациентов с бессимптомным течением
Тед не обнаружил новообразования тонкой кишки [86].
В недавнем французском проспективном исследовании среди 154 человек
с LS, который оценивал выход эзофагогастродуоденоза-
Копия выполняется каждые 3-4 года по случаю колонос
копия, всего 3 случая аденокарциномы двенадцатиперстной кишки и 4
Были обнаружены случаи аденомы полости рта [87]. Из 7 человек с
неоплазия двенадцатиперстной кишки, 3 были носителями патогенного варианта в
ген MSH2.
В настоящее время сообщается о распространенности неоплазии тонкой кишки
среди бессимптомных людей с ЛС низкий и польза
из наблюдения за тонкой кишкой не ясно; рутинное наблюдение за
тонкая кишка не рекомендуется. Большое проспективное исследование
необходимо определить ценность наблюдения пищевода-
гастродуоденоскопия при раке желудка и двенадцатиперстной кишки
риск в людях с LS.
4 Семейный риск колоректального рака
4.1 Определение
Примерно у 20–30% людей с диагнозом «CRC» семья
История болезни CRC сообщается [3]. Риск CRC у лиц с
Семейная история CRC зависит от числа пострадавших
члены семьи и возраст диагностики CRC в семье.
Согласно различным рекомендациям, люди с семьей
CRC должна подвергаться более интенсивной
чем население в целом, начиная с более раннего возраста [88–
90]. Тем не менее, определения того, кто должен пройти
Наблюдения за местами обитания показывают значительные географические различия
Пять мета-анализов оценили влияние семьи
история относительного и абсолютного риска CRC [91–95]. В
опубликованный систематически обзор и метаанализ, Вонг
и другие. обнаружили, что лица, имеющие по крайней мере одну первую степень
родственник (FDR) с CRC имел более низкий повышенный риск развития
CRC (относительный риск [ОР] 1,76, 95% ДИ 1,57–1,97; P <0,001) [91]
чем ранее сообщенные оценки риска (ОР от 2,24
до 2,26) [92–94]. Эта более низкая оценка риска развития
CRC среди FDR был подтвержден недавним метаанализом, который
сгруппированные оценки риска по дизайну исследования; это сообщило объединенный RR
среди когортных исследований 1,67 (95% ДИ 1,52–1,82) и объединенные
ОР среди исследований случай-контроль 2,22 (95% ДИ 2,00–2,48) в
наличие хотя бы одного FDR с CRC (табл. 6) [95].
более высокий RR был обнаружен в присутствии двух или более
FDR, с объединенными RR CRC 2,40 (когорта) и 2,81 (случай–
контроль) [95]. Когда CRC был диагностирован в возрасте до 50 лет
годы в FDR объединенные RR составляли 3,26 (95% CI 2,82–3,77;
когорта) и 3,57 (95% ДИ 1,07–11,85; случай – контроль) [95]. поскольку
Когортные исследования с меньшей вероятностью будут содержать смещение отзыва, авторы
считает, что итоговые оценки когортных исследований
Сер к правде. Эти ОР соответствовали кумулятивному
Лютенький риск для CRC, в 85 лет в Западной Европе, 4,8% (95% ДИ
2,7% -8,3%) для тех, у кого был один пораженный FDR, увеличившись до 8,2
% (95% ДИ от 6,1% до 10,9%) для людей с двумя или более пораженными
FDRs и 11% (95% CI 9,5% -12,4%), когда было
перенес ФДР в возрасте до 50 лет при постановке диагноза [95]. индивиду-
лица, имеющие по крайней мере одного родственника второй степени с CRC
не показали клинически значимого повышенного риска развития
CRC с объединенным RR среди когортных исследований 1,09 (95% ДИ
1.03–1.15).
Ранее опубликованные руководства сообщили, что семейные
риск CRC должен быть определен как имеющий
риск развития CRC, часто установлен в два-три раза
риск населения в целом [89,96,97]. Поэтому ESGE предлагает
определить семейный риск CRC как наличие у тех, кто имеет два
или более FDR с CRC или один FDR с CRC до возраста
50 лет
4.2 Наблюдение за семейным риском CRC
4.2.1 Защитный эффект
Только два исследования касались защитного эффекта
Ионоскопия у лиц с по крайней мере одним FDR с CRC [98,99]
(Table7s). Дав-Эдвин и соавт. зарегистрировал результаты
скрининговая колоноскопия в клинике для семей с высоким риском во время
16 лет, с целью определения, в какой степени
данные с различными семейными историями CRC (указаны в таблицах 7)
польза от колоноскопического наблюдения [98]. Среди 1678
наблюдаемое количество случаев CRC было ниже, чем
ожидаемое количество случаев в отсутствие наблюдения, с
снижение заболеваемости CRC на 80% и снижение
РЕКОМЕНДАЦИЯ
ESGE рекомендует колоноскопическое наблюдение в первую очередь
Степень родственников случаев CRC в семьях, которые выполняют
определение семейного риска колоректального рака.
Сильная рекомендация, доказательства среднего качества,
уровень согласия 100%.
РЕКОМЕНДАЦИЯ
ESGE рекомендует определение семейного риска колоректального
рак как наличие по крайней мере двух
Tive с колоректальным раком или, по крайней мере, одной первой степени
родственник с колоректальным раком в возрасте до 50 лет.
Сильная рекомендация, доказательства среднего качества,
уровень согласия 92%.
Ван Леердам Моник Э. и соавт. Эндоскопическое лечение синдрома Линча и семейного риска колоректального рака ... Эндоскопия
директива
tality 81%. Тем не менее, это исследование имеет несколько ограничений, таких как
как отсутствие надежной контрольной группы, а также возможность
занижения данных о CRC, поскольку исследование основывалось на
данные реестра служб здравоохранения (NHS). Во втором исследовании
Hatfield et al. описал результаты скрининг-колоноскопии
в когорте из 20 семей и 332 человек с семейным типом X
риск CRC (семьи, отвечающие амстердамским критериям, но
с MMR-опытными опухолями), включая 162 человека, получавших
Колоноскопия и 162 не получают
Копье. В этом исследовании они обнаружили, что колоноскопия наблюдения повторно
снизили заболеваемость CRC (мужчины, ОР 0,27 [95% ДИ 0,10–0,71];
женщины, 0,19 руб. (95% ДИ 0,07–0,48]) и смертность, связанная с КРР
Ity (мужчины, 0,38 руб. [95% ДИ 0,15–0,94]; женщины, 0,19 руб. [95% ДИ
0,07–0,49]) [99]. Это исследование также имело несколько ограничений, таких как
как нерандомизированное распределение вмешательства, историческое
контроль, ретроспективный сбор данных и неполное медицинское
записей.
Таким образом, у лиц со значительной семейной историей
CRC, колоноскопическое наблюдение, по-видимому, снижает частоту CRC
и смертность; Тем не менее, необходимы дополнительные исследования для того, чтобы
знаю, в какой степени.
4.2.2 Интервалы наблюдения
Предыдущие рекомендации рекомендуют интервал между
5 лет у тех, у кого семейный анамнез CRC [88,
89]. Различные исследования проанализировали риск развития CRC
или прогрессирующее новообразование после отрицательной колоноскопии среди
лица с по крайней мере одним FDR с CRC (исключая физических лиц
с ЛС). Подавляющее большинство этих исследований не показывают каких-либо
увеличение риска метахронной неоплазии после колоноскопии (Ta-
ble7s).
В популяционном исследовании случай-контроль Brenner et al.
показал, что риск развития CRC низок до 20 лет
после отрицательной колоноскопии [100]. Отношение шансов (ИЛИ) для
Разработка CRC для лиц с хотя бы одним FDR с CRC была
0,66 (95% ДИ 0,27–1,58) в течение 5–9 лет после отрицательного
Лоноскопия и 0,47 (95% ДИ 0,14–1,59) более 10 лет
после отрицательной колоноскопии. Защитный эффект у индивидов
показатель без семейной истории был выше, с ИЛИ 0,23
(95% ДИ 0,15–0,36) в течение 5–9 лет и 0,33 (95% ДИ 0,23–
0,48) более 10 лет после негативной колоноскопии. Мех-
кроме того, Samadder et al. выполнил наблюдательную когорту
исследование включало 131 349 человек и показало, что по сравнению
с населением штата Юта, стандартизированные
Коэффициент плотности (SIR) для CRC был постоянно низким до 10 лет
после отрицательной колоноскопии, но у лиц с по крайней мере
один FDR с CRC, это снижение риска продлевается только до 5 лет
после негативной колоноскопии [101]. В последней группе первый
отрицательная колоноскопия была связана со статистически значимым
не может снизить заболеваемость CRC только в течение первых 5 лет (SIR
0,39, 95% ДИ 0,13–0,64); после этого 5-летнего интервала, отрицательный
колоноскопия больше не защищала от CRC (SIR 0,74, 95% ДИ
0.32-1.16). Тем не менее, это исследование имеет некоторые ограничения, с
очень небольшое количество наблюдаемых случаев CRC после 5-летнего ограничения
статистическая сила результатов.
Наблюдение после удаления полипа По данным исследований
оценка эффективности колоноскопии после удаления аденомы,
нет никаких доказательств в пользу сокращения срока наблюдения
интервал у лиц с семейным анамнезом CRC (Table7s).
Существует только одно рандомизированное контролируемое исследование, сравнивающее
Интервалы колоноскопии (6 против 3 лет) у людей с
Семейная история CRC [102]. В этом исследовании, которое включало 528
индивидуумы (с одним пораженным FDR в возрасте <50 лет или двумя пострадавшими
FDRs) с 0–2 аденомами в начале исследования, Hennink et al. не нашел
значительная разница в доле лиц с
Ваденозная аденома при первом повторном осмотре в 6 лет
(6,9%) против 3 лет (3,5%), с сырым OR 2,0 (ДИ 0,9–
4,7). Авторы пришли к выводу, что ввиду относительно низкого
частота прогрессирующих аденом в 6 лет и очень низкий риск
CRC (только один CRC был обнаружен в 3-летней группе), 6-летний
интервал наблюдения следует рассматривать как соответствующий.
На основании ограниченных данных, 5-летний интервал наблюдения
рекомендуется после негативной колоноскопии для лиц с
семейный риск CRC. Кроме того, руководящие принципы наблюдения за
Популяции среднего риска после удаления аденомы могут быть следующими
мычала.
4.2.3 Начальный возраст для колоноскопического надзора
Большинство руководств рекомендуют начать колоноскопию
скрининг у лиц с семейным анамнезом CRC (в основном
оштрафован как затронутый FDR в возрасте менее 60 лет или двух пострадавших
FDRs) в возрасте 40 лет или на 10 лет раньше, чем возраст
младший индекс случай [88,89]. Обоснование для возраста 40 лет
изначально исходит из исследования Fuchs et al. [103] (табл. 8). В
это исследование, для 40-летних людей с семейной историей
CRC, совокупная частота CRC была сопоставима с
РЕКОМЕНДАЦИЯ
ESGE рекомендует начать колоноскопический надзор в
возраст 40 лет, когда существует семейный риск развития
Рака.
Сильная рекомендация, доказательства среднего качества,
уровень согласия 92%.
РЕКОМЕНДАЦИЯ
ESGE рекомендует 5-летний интервал наблюдения за
носкопия после нормального высококачественного исходного обследования
в условиях семейного риска колоректального рака.
Сильная рекомендация, доказательства низкого качества, уровень
согласие 83%.
РЕКОМЕНДАЦИЯ
ESGE рекомендует последующее наблюдение после удаления полипа в
люди с семейным риском колоректального рака должны
следовать руководящим принципам наблюдения для общего
численность населения.
Сильная рекомендация, доказательства среднего качества,
уровень согласия 92%.
Ван Леердам Моник Э. и соавт. Эндоскопическое лечение синдрома Линча и семейного риска колоректального рака ... Эндоскопия
50-летних людей без семейной истории. Хемминки и
Ли в большом проспективном когортном исследовании обнаружил похожие результаты,
отчет SIR 2,01 (95% ДИ 1,71–2,33) для физических лиц
в возрасте 40–49 лет на момент постановки диагноза, по крайней мере с одним пораженным FDR
с CRC, по сравнению с SIR 1,18 (95% CI 0,99–1,39) для
лица старше 50 лет на диагностике [104]. Другие исследования
обнаружили увеличение заболеваемости и смертности от КРК в возрасте
моложе 50 лет у родственников пациентов с КРР [105–107].
Заболеваемость КРК была увеличена с ОР 2,07 (95% ДИ 0,99–
3.80) для родственников в возрасте 50 лет и младше [105]. CRC стенд
Коэффициент смертности от сердечно-сосудистых заболеваний колебался в пределах 12,5 (95% ДИ 1,52–
45,14) и 3,66 (95% ДИ 1,47–7,55) у лиц в возрасте от 35 лет.
и 55 лет [106]. Кроме того, найдено исследование типа «случай-контроль».
что лица моложе 50 лет имели значительно
Это относительный риск CRC по сравнению с теми, кто старше 50 лет
возраст (ОР <50 лет 8,54 [95% ДИ 1,9–39] против ОР 50 лет 1,87
[95% ДИ 1,4–2,8]) [107]. Это подтверждается еще одним случаем -
контрольное исследование, включающее 18 208 пациентов с КРР из-за рака
исследование, которое обнаружило повышенный риск FDR в более молодом возрасте (<
50 лет) и хотя FDRs в обеих возрастных группах (<50 и> 50
лет) постоянно повышенный риск развития рака,
у молодых пациентов с КРР (<40 лет) был самый высокий семейный
риск, когда они были моложе 50 лет (ЧСС 7,0 [95%
CI 2,86–17,09]) [108].
Нет никаких доказательств того, что колоноскопия за 10 или 5 лет до
самый молодой диагноз CRC в семье является полезным; тем не мение
это может быть рекомендовано в индивидуальном порядке после полного консультирования
человек о рисках и преимуществах процедуры.
Основываясь на этих результатах, мы советуем начать колоноскопию
наблюдение в возрасте 40 лет за лицами с семейными
Риск колоректального рака.
С другой стороны, все эти результаты получены из наблюдательных
исследования и основаны на оценках относительного риска. В недавней системе
тематический обзор и метаанализ, оценки абсолютного риска
для CRC в разных возрастах были рассчитаны [95]. Результаты, достижения
показал, что риск CRC составляет менее 1% в ближайшие 10 лет
для 40-летних лиц, удовлетворяющих критериям семейного риска
CRC, и приближается к 2% в следующие 10 лет для этих
особи в 50 лет. В ближайшее время, когда больше доказательств
эти результаты могут помочь начать наблюдение за
люди с семейным риском CRC в 50 лет.
Комментарии
Это руководство обеспечивает основу для эндоскопического
возраст лиц с LS, и предлагает определение
милиарный риск развития колоректального рака для выявления группы
У которых обоснован колоноскопический надзор, так как они
имеют высокий риск (ОР> 2,5) для развития CRC.
Доказательства ограничены в нескольких областях, и дальнейшие исследования
необходимо. Такие области включают, среди прочего: оценку
оптимальный возраст и интервалы для колоноскопического наблюдения
среди людей с LS и тех, у кого есть семейный риск CRC;
надзор за желудком и тонкой кишкой при ЛС; а также
Выход скрининга фекального иммунохимического теста (FIT) среди
люди с семейным риском CRC.
отказ
Правовая оговорка для руководящих принципов ESGE [8] относится к этому
Руководство.
Подтверждения
Авторы выражают благодарность профессору К. Хасану из
больница им. Маргариты, Рим, и д-р С. Энгель, Института
по медицинской информатике, статистике и эпидемиологии, Лейпциг,
за их ценные комментарии к рукописи.
Кроме того, мы хотели бы поблагодарить Ариадну Санчес, Лизет
Риверо-Санчес, Сабела Карбалл, Каролина Мангас-Санджуан,
Герхард Юнг, Александар Гаврик, д-р Дора Колусси, д-р Chiara
Пирантони и Фариди ван Эттен-Джамалудин за помощь
о систематических поисках и обзоре литературы.
Наконец, мы хотели бы поблагодарить Клэр Гай за организацию
Процедура Фи и Полин Рошто и Франсуаза Хайден-
Рейх для организации всех встреч и телефонных конференций
CES для Руководства.
Конкурирующие интересы
Э. Деккер был председателем консультативного совета по профилактике рака
ceuticals (2019) и является соредактором по эндоскопии. М. Ф. Каминский имеет
получал спикерские, преподавательские и консультационные услуги от Olympus
(С 2017 года по настоящее время) и оплату услуг докладчиков и преподавателей, а также кредит
оборудование от Fujifilm (2019). Х. Нейман предоставил консультанта-
Cy услуги для Fujifilm и Pentax (с 2012 года по настоящее время). М. Пеллисе
Норгина Иберия (2019 г.), гонорар консультантов
из Casen Recordati (2017–2019), Olympus (2017) и Янсен
(2018), и является соредактором по эндоскопии; ее отдел получил
Кредит на оборудование от Fujifilm (с 2017 года по настоящее время) и исследование
пожертвование от Fujifilm (2019). JE van Hooft получил плату за лекцию
Medtronics (2014–2015) и Cook Medical (2019), а также
сборы за обучение от Boston Scientific (2014–2017); ее отдел имеет
получил исследовательские гранты от Cook Medical (2014–2018) и Ab-
консервы (2014–2017). Ф. Балагер, Р. Джовер, А. Латчфорд, Л. Риккардиелло,
VH Roos, M. Rupińska, J.-C. Саурин, П.Дж. Танис, М.Е. ван Леердам и
У А. Вагнера нет конкурирующих интересов.
Список литературы:
Рекомендуемые статьи
Эндоскопическая ретроградная холангиопанкреатография
- рентген-эндоскопический метод диагностики патологии желчных и панкреатических протоков.
При эндоскопическом исследовании в случае бронхоэктазов в стадии ремиссии выявляется
частично диффузный бронхит I степени воспаления
Активируйте PUSH уведомления в браузер
Отключите PUSH уведомления в браузер
Содержание
Интернет магазин
Популярное
- О нас
- Правовые вопросы
- Политика
обработки персональных
данных EndoExpert.ru - Связаться с нами
- Стать партнером
© 2016-2022 EndoExpert.ru

Вы находитесь в разделе предназначенном только для специалистов (раздел для пациентов по ссылке). Пожалуйста, внимательно прочитайте полные условия использования и подтвердите, что Вы являетесь медицинским или фармацевтическим работником или студентом медицинского образовательного учреждения и подтверждаете своё понимание и согласие с тем, что применение рецептурных препаратов, обращение за той или иной медицинской услугой, равно как и ее выполнение, использование медицинских изделий, выбор метода профилактики, диагностики, лечения, медицинской реабилитации, равно как и их применение, возможны только после предварительной консультации со специалистом. Мы используем файлы cookie, чтобы предложить Вам лучший опыт взаимодействия. Файлы cookie позволяют адаптировать веб-сайты к вашим интересам и предпочтениям.
Я прочитал и настоящим принимаю вышеизложенное, хочу продолжить ознакомление с размещенной на данном сайте информацией для специалистов.














.jpg)


.png)













Комментарии