- Компании
- Takeda. О компании, буклеты, каталоги, контакты
- Olympus. О компании, буклеты, каталоги, контакты
- Boston Scientific. О компании, буклеты, каталоги, контакты
- Pentax. О компании, буклеты, каталоги, контакты
- Fujifilm & R-Farm. О компании, буклеты, каталоги, контакты
- Erbe. О компании, буклеты, каталоги, контакты
- Еще каталоги
- Мероприятия
- Информация
- Обучение
- Классификации
- Атлас
- Quiz
- Разделы
- Пациенту
QR-код этой страницы

Для продолжения изучения на мобильном устройстве ПРОСКАНИРУЙТЕ QR-код с помощью спец. программы или фотокамеры мобильного устройства
Статьи: Рекомендации Российской гастроэнтерологической ассоциации по диагностике и лечению гастроэзофагеальной рефлюксной болезни 2020
Аннотация:
Цель. Настоящие рекомендации Российской гастроэнтерологической ассоциации разработаны с целью ознакомления практикующих врачей с современными методами диагностики, тактикой лечения и особенностями рациональной фармакотерапии больных с гастроэзофагеальной рефлюксной болезнью (ГЭРБ).
Основные положения. Распространенность ГЭРБ в Российской Федерации варьирует от 11,3 до 23,6 %. Диагноз ГЭРБ устанавливается на основании анамнестических данных и результатов инструментального обследования. Эзофагогастродуоденоскопия (ЭГДС) позволяет обнаружить признаки рефлюкс-эзофагита разной степени выраженности, выявить цилиндроклеточную метаплазию эпителия пищевода. Пациентам с рефрактерным течением заболевания (при отсутствии убедительной клинической и эндоскопической ремиссии в течение 4-8 недель проведения терапии стандартной дозой ИПП) или при наличии стриктур, пищевода Баррета необходимо проведение ЭГДС с биопсией пищевода и гистологическим исследованием биоптатов. По показаниям пациентам должны быть выполнены внутрипищеводная суточная рН-метрия или рН-импедансометрия, манометрия высокого разрешения, позволяющие полно изучить функциональное состояние пищевода и пищеводно-желудочного перехода, прогнозировать варианты течения заболевания и результаты его лечения.
Лечение пациентов ГЭРБ должно быть индивидуализировано в соответствии с клиническими проявлениями заболевания, интенсивностью симптомов и направлено на устранение симптомов, заживление эрозий при эрозивном эзофагите, предупреждение осложнений, профилактику прогрессирования пищевода Баррета и развития дисплазии и аденокарциномы пищевода.
Наиболее эффективными препаратами для лечения ГЭРБ являются ИПП, которые применяются для проведения как основной (4-8 нед), так и поддерживающей терапии. В качестве монотерапии редко возникающей изжоги, которая не сопровождается развитием эзофагита, а также в схемах комплексной терапии ГЭРБ для быстрого устранения симптомов пациентам рекомендованы антациды. Прокинетические препараты могут быть применены в составе комплексной терапии ГЭРБ вместе с ИПП, так как они способствуют восстановлению нормального физиологического состояния пищевода, воздействуя на патогенетические механизмы ГЭРБ.
При осложненном течении заболевания (повторные кровотечения, пептические стриктуры пищевода) больным показано антирефлюксное хирургическое лечение с предварительным исследованием функциональных показателей пищевода с помощью рН-импедансометрии и манометрии высокого разрешения.
Заключение. Настоящие клинические рекомендации обобщают актуальную информацию о ГЭРБ с позиции доказательной медицины. Соблюдение рекомендаций позволит улучшить качество оказания медицинской помощи пациентам ГЭРБ, а также проводить своевременную профилактику осложнений.
Полный текст статьи:
Рекомендации Российской гастроэнтерологической ассоциации по диагностике и лечению
гастроэзофагеальной рефлюксной болезни
В.Т. Ивашкин1, И.В. Маев2, А.С. Трухманов1,*, Т.Л. Лапина1, О.А. Сторонова1,
О.В. Зайратьянц2, О.Б. Дронова3, Ю.А. Кучерявый2, С.С. Пирогов4, Р.Г. Сайфутдинов5, Ю.П. Успенский6, А.А. Шептулин1, Д.Н. Андреев2, Д.Е. Румянцева1
1 ФГАОУ ВО «Первый Московский государственный медицинский университет им. И.М. Сеченова»
(Сеченовский Университет) Министерства здравоохранения Российской Федерации, Москва, Российская Федерация
2 ФГБОУ ВО «Московский государственный медико-стоматологический университет им. А.И. Евдокимова» Министерства здравоохранения Российской Федерации, Москва, Российская Федерация
3 ФГБОУ ВО «Оренбургский государственный медицинский университет» Министерства здравоохранения Российской Федерации, Оренбург, Российская Федерация
4 МНИОИ им. П.А. Герцена — филиал ФГБУ «Национальный медицинский исследовательский радиологический центр» Министерства здравоохранения Российской Федерации, Москва, Российская Федерация
5 Казанская государственная медицинская академия — филиал ФГБОУ ДПО «Российская медицинская академия непрерывного профессионального образования» Министерства здравоохранения Российской, Казань,
Российская Федерация
6 ФГБОУ ВО «Санкт-Петербургский государственный педиатрический медицинский университет» Министерства здравоохранения Российской Федерации, Санкт-Петербург, Российская Федерация
Цель. Настоящие рекомендации Российской гастроэнтерологической ассоциации разработаны с целью оз- накомления практикующих врачей с современными методами диагностики, тактикой лечения и особенно- стями рациональной фармакотерапии больных с гастроэзофагеальной рефлюксной болезнью (ГЭРБ).
Основные положения. Распространенность ГЭРБ в Российской Федерации варьирует от 11,3 до 23,6 %. Диагноз ГЭРБ устанавливается на основании анамнестических данных и результатов инструментального обследования. Эзофагогастродуоденоскопия (ЭГДС) позволяет обнаружить признаки рефлюкс-эзофагита разной степени выраженности, выявить цилиндроклеточную метаплазию эпителия пищевода. Пациентам с рефрактерным течением заболевания (при отсутствии убедительной клинической и эндоскопической ре- миссии в течение 4–8 недель проведения терапии стандартной дозой ИПП) или при наличии стриктур, пи- щевода Баррета необходимо проведение ЭГДС с биопсией пищевода и гистологическим исследованием биоптатов. По показаниям пациентам должны быть выполнены внутрипищеводная суточная рН-метрия или рН-импедансометрия, манометрия высокого разрешения, позволяющие полно изучить функциональное состояние пищевода и пищеводно-желудочного перехода, прогнозировать варианты течения заболевания и результаты его лечения.
Лечение пациентов ГЭРБ должно быть индивидуализировано в соответствии с клиническими проявлениями заболевания, интенсивностью симптомов и направлено на устранение симптомов, заживление эрозий при эрозивном эзофагите, предупреждение осложнений, профилактику прогрессирования пищевода Баррета и развития дисплазии и аденокарциномы пищевода.
Наиболее эффективными препаратами для лечения ГЭРБ являются ИПП, которые применяются для прове- дения как основной (4–8 нед), так и поддерживающей терапии. В качестве монотерапии редко возникающей изжоги, которая не сопровождается развитием эзофагита, а также в схемах комплексной терапии ГЭРБ для быстрого устранения симптомов пациентам рекомендованы антациды. Прокинетические препараты могут быть применены в составе комплексной терапии ГЭРБ вместе с ИПП, так как они способствуют восстанов- лению нормального физиологического состояния пищевода, воздействуя на патогенетические механизмы ГЭРБ.
При осложненном течении заболевания (повторные кровотечения, пептические стриктуры пищевода) боль- ным показано антирефлюксное хирургическое лечение с предварительным исследованием функциональных показателей пищевода с помощью рН-импедансометрии и манометрии высокого разрешения.
Заключение. Настоящие клинические рекомендации обобщают актуальную информацию о ГЭРБ с позиции доказательной медицины. Соблюдение рекомендаций позволит улучшить качество оказания медицинской помощи пациентам ГЭРБ, а также проводить своевременную профилактику осложнений.
Для цитирования: Ивашкин В.Т., Маев И.В., Трухманов А.С., Лапина Т.Л., Сторонова О.А., Зайратьянц О.В., Дронова О.Б., Кучерявый Ю.А., Пирогов С.С., Сайфутдинов Р.Г., Успенский Ю.П., Шептулин А.А., Андреев Д.Н., Румянцева Д.Е. Рекомендации Российской гастроэнтерологической ассоциации по диагностике и лечению гастроэзофагеальной рефлюксной болезни. Российский журнал гастроэнтерологии, гепатологии, колопроктологии. 2020;30(4):. https://doi. org/10.22416/1382-4376-2020-30-4-
Recommendations of the Russian Gastroenterological Association in Diagnosis and Treatment of Gastroesophageal Reflux Disease
Vladimir T. Ivashkin1, Igor V. Maev2, Alexander S. Trukhmanov1,*, Tatyana L. Lapina1, Olga A. Storonova1, Oleg V. Zayratyants2, Olga B. Dronova3, Yury A. Kucheryavyy2, Sergei S. Pirogov4, Rafik G. Sayfutdinov5, Yury P. Uspenskiy6, Arkady A. Sheptulin1, Dmitriy N. Andreev2, Diana E. Rumyantseva1
1 Sechenov First Moscow State Medical University (Sechenov University), Moscow, Russian Federation
2 Moscow State University of Medicine and Dentistry, Moscow, Russian Federation
3 Orenburg State Medical University, Orenburg, Russian Federation
4 Herzen Moscow Oncology Research Center — Branch of the National Medical Research Radiology Center, Moscow, Russian Federation
5 Kazan State Medical Academy — Branch of the Russian Medical Academy of Continuous Professional Education, Kazan, Russian Federation
6 Saint-Petersburg State Pediatric Medical University, St. Petersburg, Russian Federation
 |
For citation: Ivashkin V.T., Maev I.V., Trukhmanov A.S., Lapina T.L., Storonova O.A., Zayratyants O.V., Dronova O.B., Kucheryavyy Yu.A., Pirogov S.S., Sayfutdinov R.G., Uspenskiy Yu.P., Sheptulin A.A., Andreev D.N., Rumyantseva D.E.Recommendations of the Russian Gastroenterological Association in Diagnosis and Treatment of Gastroesophageal Reflux Disease. Russian Journal of Gastroenterology, Hepatology, Coloproctology. 2020;30(4): . https://doi.org/10.22416/1382-4376-2020-30-4- .
1. Общая информация
o гастроэзофагеальной рефлюксной болезни
1.1. Определение гастроэзофагеальной рефлюксной болезни, ее основных форм и пищевода Баррета
Гастроэзофагеальная рефлюксная болезнь (ГЭРБ) — это хроническое рецидивирующее забо- левание, обусловленное нарушением моторно-эва- куаторной функции органов гастроэзофагеальной зоны и характеризующееся регулярно повторяю- щимся забросом в пищевод желудочного и в ряде случаев дуоденального содержимого, что приводит к появлению клинических симптомов, ухудшаю- щих качество жизни пациентов, к повреждению слизистой оболочки дистального отдела пищево- да с развитием в нем дистрофических изменений неороговевающего многослойного плоского эпите- лия, катарального или эрозивно-язвенного эзофа- гита (рефлюкс-эзофагита), а у части больных ци- линдроклеточной метаплазии [1–3].
Неэрозивную рефлюксную болезнь (НЭРБ) и эрозивный эзофагит следует считать двумя фор- мами гастроэзофагеальной рефлюксной болезни. НЭРБ — это субкатегория ГЭРБ, характеризующа- яся наличием вызванных рефлюксом и снижающих качество жизни симптомов без эрозий слизистой оболочки пищевода, выявляемых при проведении обычного эндоскопического исследования, и в от- сутствие антисекреторной терапии в данный мо- мент. Подтвердить диагноз НЭРБ могут пробы с ингибиторами протонной помпы (ИПП), обнару- жение патологического рефлюкса при рН-метрии или выявление специфических эндоскопических признаков эзофагита при проведении высокотех- нологичных методов (увеличение с высоким раз- решением, узкоспектральная эндоскопия) [4–6]. Лекарственные пробы с применением антисекре- торных препаратов нельзя считать специфичными, однако их отрицательный результат демонстрирует высокую вероятность отсутствия ГЭРБ [7].
Пищевод Баррета — замещение плоского эпи- телия железистым цилиндрическим метаплазиро- ванным в слизистой оболочке дистального отдела пищевода, выявляемое при эндоскопическом ис- следовании, подтвержденное наличием кишечной метаплазии при гистологическом исследовании биоптата, и в ряде случаев повышающее риск раз- вития аденокарциномы пищевода (АКП) [8–11].
1.2. Эпидемиология
Истинную распространенность ГЭРБ достаточ- но трудно оценить, поскольку лишь около четвер- ти больных ГЭРБ обращаются за помощью к врачу [12, 13]. Эпидемиологические данные свидетель- ствуют о том, что распространенность заболевания варьирует от 8,8 до 33,1 %, а заболеваемость имеет неуклонную тенденцию к росту во всех регионах мира [14, 15]. Наиболее высокие показатели рас- пространенности регистрируются в Европе и Север- ной Америке, а низкие — в странах Азии [15, 16]. Согласно последнему метаанализу, опубликованно- му в 2018 году, общемировая распространенность ГЭРБ составляет 13,3 % (95 % ДИ: 12,0–14,6 %)
[17]. При этом частота заболевания выше у лиц старше 50 лет (ОШ 1,32; 95 % ДИ: 1,12–1,54), ку-
рильщиков (ОШ 1,26; 95 % ДИ 1,04–1,52), а так- же у лиц, страдающих ожирением (ОШ 1,73; 95 % ДИ 1,46–2,06) [17]. В России распространенность ГЭРБ варьирует от 11,3 до 23,6 %, а описанные факторы риска характерны и для мировой попу- ляции [18, 19]. В общей популяции распростра- ненность эзофагита оценивается в 5–6 %; при этом у 65–90 % больных отмечается незначительно вы- раженный и умеренный эзофагит, у 10–35 % — тя- желый эзофагит [20–24]. Частота возникновения тяжелого эзофагита в общей популяции составляет 5 случаев на 100 000 населения в год. Распростра- ненность пищевода Баррета среди лиц с эзофаги- том приближается к 8 % с колебаниями в диапазоне от 5 до 30 %.
В последние десятилетия наблюдается рост за- болеваемости АКП, которая развивается на фоне прогрессирования диспластических изменений в метаплазированном по кишечному типу эпителии слизистой оболочки дистального отдела пищево- да. АКП и дисплазия высокой степени развива- ется у 0,4–0,6 % больных с пищеводом Баррета с кишечной метаплазией в год. АКП развивается у 0,5 % больных при низкой степени дисплазии эпителия, у 6 % в год — при дисплазии высокой степени и менее чем у 0,1 % — без дисплазии [1, 8, 9, 11].
1.3. Этиология и патогенез
Гастроэзофагеальная рефлюксная болезнь — это кислотозависимое заболевание, при котором соляная кислота желудочного сока выступает ос- новным повреждающим фактором при развитии клинических симптомов и морфологических про- явлений ГЭРБ. Патологический рефлюкс при этом возникает вследствие недостаточности нижнего пи- щеводного сфинктера (НПС), то есть ГЭРБ — за- болевание с исходным нарушением двигательной функции верхних отделов желудочно-кишечного тракта (ЖКТ) [7, 25–28].
Ключевым фактором патогенеза ГЭРБ высту- пает патологически высокая частота и/или дли- тельность эпизодов заброса содержимого желудка в пищевод. Целостность слизистой оболочки пи- щевода обусловлена равновесием между фактора- ми агрессии и способностью слизистой оболочки противостоять повреждающему действию забрасы- ваемого содержимого желудка при гастроэзофаге- альном рефлюксе (ГЭР). Нарушение этого равно- весия у большой части пациентов сопровождается существенным замедлением восстановления рН дистальной части пищевода после каждого эпизода рефлюкса. Нарушение клиренса пищевода разви- вается вследствие комбинации нескольких факто- ров: ослабления перистальтики грудного отдела пищевода, снижения секреции слюны и муцина [29]. Первым барьером, оказывающим цитопро- тективный эффект, является слой слизи, покры- вающий эпителий пищевода и содержащий муцин [30]. Слизистый слой является одним из ключевых составляющих химического клиренса пищевода и восстановления рН в пищеводе до нормальных показателей, нарушение которого способству- ет ухудшению очищения пищевода от попавшего в него кислого, слабокислого или слабощелочного содержимого. Установлено, что секреция муцинов в слизи при ГЭРБ снижается в зависимости от тя- жести эзофагита, что является дополнительным фактором, предрасполагающим к развитию эро- зивного эзофагита в условиях продолжающегося ГЭР. Поэтому дополнительное повышение защит- ных свойств слизистого барьера наряду с кислото- супрессией является важным компонентом лечения ГЭРБ [31–33] (УУР В, УДД — 3).
Значительное увеличение секреции соляной кислоты желудка существенно повышает риск воз- никновения ГЭРБ.
У подавляющего большинства больных ГЭРБ эпизоды рефлюкса возникают преимущественно во время преходящих расслаблений нижнего пище- водного сфинктера (ПРНПС). Во время ПРНПС антирефлюксный барьер между желудком и пище- водом исчезает обычно на 10–15 секунд вне связи с актом глотания [22].
ПРНПС как принципиальный механизм реф- люкса осуществляется через те же проводящие пути от дорсального ядра блуждающего нерва (nucleus dorsalis и nucleus ambiguus), которые опосредуют перистальтику пищевода и расслабле- ние НПС у здорового человека. Механорецепторы, расположенные в верхней части желудка, реаги- руют на повышение давления внутри органа и по- сылают сигналы в задний мозг по афферентным волокнам блуждающего нерва. В центрах заднего мозга, воспринимающих данные сигналы, форми- руются моторные программы ПРНПС, по нисхо- дящим путям достигающие НПС. Эфферентные пути осуществляются через блуждающий нерв, где оксид азота (NO) является постганглионарным нейротрансмиттером. Сокращение ножек диафраг- мы контролируется дыхательным центром в ство- ле мозга и ядром диафрагмального нерва. Повы- шение внутрибрюшного давления при совпадении с ПРНПС существенно увеличивает вероятность рефлюкса.
В настоящее время в понимании механизма ГЭР следует руководствоваться парадигмой вза- имного влияния ПРНПС и последствий деструк- туризации пищеводно-желудочного соединения. Слабость ножек диафрагмы приводит либо к за- держке времени начала действия, либо к суще- ственной деградации собственно компрессионного эффекта сокращения диафрагмы на НПС. Грыжа пищеводного отверстия диафрагмы, в зависимости от ее размеров и строения, оказывает механиче- ское воздействие на НПС: ухудшает антирефлюкс- ную функцию во время ПРНПС и/или снижает собственно тоническую составляющую сфинктера. Наиболее важным следствием деструктуризации зоны пищеводно-желудочного соединения оказы- вается заброс из желудка в пищевод относительно больших объемов жидкого содержимого в период ПРНПС [22, 34].
У значительного количества больных эпизоды ГЭР развиваются при нормальных показателях давления НПС. Механизм ГЭР связан с высоким градиентом давления между желудком и пище- водом, обусловленным различными причинами: у части пациентов это нарушение эвакуации со- держимого, у другой части — высокое внутри- брюшное давление. В этих случаях ГЭР разви- вается вследствие неспособности запирательных механизмов противодействовать высокому гради- енту давления в желудке [35, 36]. Действительно, у половины больных с ГЭРБ обнаруживают сим- птомы функциональной диспепсии (ФД) и у 40– 52 % пациентов с ФД выявляют сопутствующую ГЭРБ [37]. Высокая частота сочетания ГЭРБ и ФД объясняется тем, что нарушения аккомо- дации фундального отдела желудка и замедление его опорожнения способствуют увеличению часто- ты эпизодов ПРНПС [38].
Результаты проведенных в последние годы ис- следований свидетельствуют об изменении микро- биоты пищевода и желудка у пациентов с ГЭРБ, пищеводом Баррета и АКП. Потенциальными медиаторами воспаления и канцерогенеза высту- пают толл-подобные рецепторы, цитокины, ядер- ный фактор κB, циклооксигеназа-2, экспрессия которых может модифицироваться в зависимости от состава микробиоты. В настоящее время убе- дительных данных о влиянии тех или иных из- менений бактериального состава на функциональ- ное и структурное состояние пищевода и желудка мало, и необходимы дальнейшие исследования в этом направлении [39–41].
Таким образом, с патофизиологической точки зрения ГЭРБ — это кислотозависимое заболева- ние, развивающееся на фоне первичного наруше- ния двигательной функции верхних отделов пище- варительного тракта.
1.4. Особенности кодирования ГЭРБ по Международной статистической классификации болезней и проблем, связанных со здоровьем
K21 — Гастроэзофагеальный рефлюкс
K21.0 — Гастроэзофагеальный рефлюкс с эзо- фагитом
K21.9 — Гастроэзофагеальный рефлюкс без эзо- фагита
K22.1 — Язва пищевода
1.5. Классификация и клиническая картина
Пищеводные проявления
Наиболее широко применяемой в мире класси- фикацией клинических проявлений ГЭРБ являет- ся Монреальская [42]. Она подразделяет клини- ческие проявления ГЭРБ на две большие группы: пищеводные проявления и внепищеводные прояв- ления. В свою очередь, пищеводные проявления включают такие клинические синдромы, как ти- пичный симптомокомплекс рефлюкса и некарди- альную боль в грудной клетке, а также синдромы, при которых кроме жалоб имеются эндоскопиче- ские проявления заболевания (эзофагит, пищевод Баррета, стриктуры и др.).
Типичный симптомокомплекс рефлюкса вклю- чает изжогу, отрыжку, срыгивание, одинофагию, которые являются мучительными для пациентов, значительно ухудшают качество их жизни, отри- цательно сказываются на их работоспособности. Особенно значительно снижается качество жизни больных ГЭРБ, у которых клинические симптомы заболевания наблюдаются в ночное время [1, 3, 23]. Изжога представляет собой наиболее характер- ный симптом, встречается у 83 % больных и возни- кает вследствие длительного контакта желудочно- го содержимого со слизистой оболочкой пищевода. Типичным для данного симптома считается усиле- ние при погрешностях в диете, приеме алкоголя, газированных напитков, физическом напряжении, наклонах и в горизонтальном положении [43, 44]. Отрыжка как один из ведущих симптомов ГЭРБ встречается достаточно часто и обнаружи- вается у 52 % больных. Отрыжка, как правило, усиливается после еды, приема газированных на- питков. Срыгивание, наблюдаемое у некоторых больных ГЭРБ, усиливается при физическом на- пряжении и при положении тела, способствующем регургитации.
Дисфагия и одинофагия наблюдаются у 19 % пациентов с ГЭРБ. В основе возникновения пре- ходящих эпизодов дисфагии лежит гипермоторная дискинезия пищевода, а причиной одинофагии может быть эрозивно-язвенное поражение слизи- стой оболочки. Появление более стойкой дисфагии и одновременное уменьшение изжоги может сви- детельствовать о формировании стеноза пищевода как доброкачественного, так и злокачественного характера.
Некардиальные боли в грудной клетке, по ходу пищевода (за грудиной), похожи на коронарную боль. Эти боли купируются нитратами, но в отли- чие от стенокардии не связаны с физической на- грузкой, а возникают вследствие гипермоторной дискинезии пищевода, причиной которой может быть дефект системы ингибирующего трансмитте- ра — оксида азота. Пусковым моментом для воз- никновения эзофагоспазма и соответственно боли служит патологический желудочно-пищеводный рефлюкс.
Внепищеводные проявления
Внепищеводные проявления ГЭРБ представ- ляют собой многообразные симптомы и синдро- мы, которые подразделяются на две группы: те, связь которых с ГЭРБ основана на достаточно убедительных клинических доказательствах (хро- нический кашель, связанный с рефлюксом, хро- нический ларингит, бронхиальная астма и эрозии эмали зубов), и те, связь которых с ГЭРБ лишь предполагается (фарингит, синусит, легочный фи- броз, средний отит) [42].
Многочисленные исследования показали увели- чение риска заболеваемости бронхиальной астмой, а также тяжести ее течения у больных ГЭРБ. ГЭР выявляется у 30–90 % больных бронхиальной аст- мой, предрасполагая к ее более тяжелому течению. Причинами развития бронхообструкции при ГЭРБ являются ваго-вагальный рефлекс и микроаспира- ция. Включение в таких случаях в комплексную терапию ИПП повышает эффективность лечения бронхиальной астмы [45].
Першение в горле, осиплость или даже по- теря голоса, сухой кашель могут быть резуль- татом заброса желудочного содержимого в гор- тань (отоларингологический синдром). Методом, верифицирующим связь подобных симптомов с ГЭР, является 24-часовая внутрипищеводная рН-импедансометрия. Данный метод позволяет установить наличие корреляции между появлением симптома и эпизодами рефлюкса (индекс симпто- ма > 50 %). Дополнительным методом диагностики может быть определение пепсина в слюне [46].
Стоматологический синдром проявляется по- ражением зубов вследствие повреждения зубной эмали агрессивным желудочным содержимым. У больных ГЭРБ возможен кариес, развитие дентальных эрозий. В редких случаях развивается аф- тозный стоматит.
Воспалительные изменения слизистой обо- лочки пищевода
Рефлюкс-эзофагит, выявляемый при эндоско- пическом исследовании, включает в себя простой (катаральный) эзофагит, эрозии и язвы пищевода. Эрозивный эзофагит может быть различной сте- пени тяжести — с А по D по Лос-Анджелесской классификации в зависимости от площади пораже- ния [21, 26].
Осложнения
К осложнениям ГЭРБ относят язвы пищевода, кровотечения, пептическую стриктуру и пищевод Баррета.
Кровотечения, обусловленные эрозивно-язвен- ными поражениями пищевода, могут наблюдаться как при наличии варикозно-расширенных вен пи- щевода, так и в их отсутствие.
Пептические стриктуры пищевода требуют в дальнейшем проведения дорогостоящих хирур- гических и эндоскопических (причем нередко повторных) процедур (бужирование, оперативное лечение и т. д.). Каждый подобный случай следует рассматривать как результат неадекватной кон- сервативной терапии, что обосновывает необхо- димость ее совершенствования для профилактики развития стриктур.
Грозное осложнение ГЭРБ — пищевод Баррета — представляет собой развитие цилиндрического (кишечного) метаплазированного эпителия в сли- зистой оболочке пищевода, повышающее в после- дующем риск развития АКП. Примерно 95 % слу- чаев АКП диагностируется у больных с пищеводом Баррета. Поэтому основную роль в профилактике и ранней диагностике рака пищевода играет диа- гностика и эффективное лечение пищевода Барре- та [8–11, 47]. Длительное применение ИПП может приводить к частичной регрессии ограниченного участка цилиндрической метаплазии.
Среди факторов риска развития осложнений ГЭРБ наибольшее значение имеют частота возникновения и длительность существования симптомов, в частности изжоги, выраженность эрозивного эзофагита, частота его рецидивов, наличие грыжи пищеводного отверстия диафрагмы (ГПОД), ожи- рение, наличие ночных рефлюксов.
Быстро прогрессирующая дисфагия и потеря веса могут указывать на развитие АКП, однако эти симптомы возникают лишь на поздних стадиях за- болевания, поэтому клиническая диагностика рака пищевода, как правило, запаздывает. Вследствие этого профилактика и ранняя диагностики рака пищевода предполагают своевременное выявление и адекватное лечение пищевода Баррета.
2. Диагностика ГЭРБ, медицинские показания и противопоказания
к применению методов диагностики
Критерии установления диагноза ГЭРБ
Диагноз ГЭРБ устанавливается на основании:
1) анамнестических данных (характерные жа- лобы, выявление ГЭРБ прежде);
2) инструментального обследования (обнаруже- ние рефлюкс-эзофагита при эндоскопическом ис- следовании пищевода, выявление патологического желудочно-пищеводного рефлюкса при рН- метрии и рН-импедансометрии).
2.1. Жалобы и анамнез
Характерные для пациентов с ГЭРБ жалобы и данные анамнеза указаны в подразделе 1.5.
2.2. Инструментальные диагностические исследования
• Пациентам с подозрением на ГЭРБ, при отсутствии противопоказаний, с целью подтвержде- ния диагноза и проведения дифференциального диагноза рекомендовано проведение эзофагога- стродуоденоскопии (УУР С, УДД — 5).
У больных, предъявляющих жалобы на изжогу, при эндоскопическом исследовании могут отмечаться признаки ГЭРБ различной степени выраженности. В их число входят гиперемия и рыхлость слизистой оболочки пищевода, эрозии и язвы (эрозивный эзофагит различной степени тя- жести — с А по D степень — в зависимости от пло- щади поражения), наличие экссудата, наложений фибрина или признаков кровотечения [44, 48].
Лос-Анджелесская классификация предус- матривает четыре степени рефлюкс-эзофагита на основании распространенности процесса. Ос- ложнения ГЭРБ: стриктуры, язвы, пищевод Бар- рета — рассматриваются отдельно и могут быть при любой степени.
Степень А — один (или более) участок повреж- денной слизистой оболочки размером до 5 мм, ко- торый не захватывает слизистую оболочку между складками (расположен на вершине складки).
Степень В — один (или более) участок повреж- денной слизистой оболочки размером более 5 мм, который не захватывает слизистую оболочку меж- ду складками (расположен на вершине складки).
Степень С — один (или более) участок по- врежденной слизистой оболочки, который рас- пространяется на слизистую оболочку между дву- мя или более складками, но вовлекает менее 75 % окружности пищевода.
Степень D — один (или более) участок повреж- денной слизистой оболочки, который вовлекает бо- лее 75 % окружности пищевода.
Помимо этого могут отмечаться пролапс желу- дочной слизистой оболочки в пищевод, особенно при рвотных движениях, истинное укорочение пищевода с расположением пищеводно-желудоч- ного перехода существенно выше диафрагмы, за- брос желудочного или дуоденального содержимого в пищевод. Оценить замыкательную функцию кар- дии при эзофагогастроскопии сложно, так как кар- дия может быть приоткрыта рефлекторно в ответ на введение эндоскопа и инсуффляцию воздуха.
• Всем пациентам ГЭРБ перед проведением зон- довых методов (ЭГДС, рН / рН-импедансометрия) необходимо исследовать анализы крови на гепати- ты В и С (антитела к HCV, HBsAg), ВИЧ, сифи- лис (УУР С, УДД — 5).
• Пациентам с рефрактерным течением забо- левания (отсутствии убедительной клинической и эндоскопической ремиссии в течение 4–8 недель проведения терапии стандартной дозой ИПП), а также пациентам с наличием осложнений забо- левания (стриктуры, пищевод Баррета) рекомен- довано проведение эзофагогастродуоденоскопии (ЭГДС) с биопсией пищевода и гистологическим исследованием биоптатов для исключения эозино- фильного эзофагита, а также пищевода Баррета и аденокарциномы (УУР В, УДД — 3).
Гистологическое исследование биоптатов сли- зистой оболочки пищевода при ГЭРБ выяв- ляет сочетание выраженных в разной степени дистрофических, некротических, острых и хро- нических воспалительных, а также репаративных и компенсаторных изменений. При НЭРБ из- менения выражены минимально и представлены межклеточным отеком неороговевающего много- слойного плоского эпителия и дистрофическими изменениями эпителиоцитов. Изменения эпителия сопровождаются микроциркуляторными наруше- ниями с гиперемией сосудов собственной пластин- ки слизистой оболочки. Характерны увеличение числа, изменение длины сосудисто-стромальных сосочков и гиперсекреция субэпителиальных кар- диальных и эзофагеальных желез (простой, ката- ральный рефлюкс-эзофагит). В части наблюдений обнаруживают атрофию многослойного плоского эпителия, причем в сочетании с относительно спец- ифичной для ГЭРБ очаговой гиперплазией его ба- зального слоя, занимающего до 10–15 % толщины эпителиального пласта. Гладкомышечные клетки собственной пластинки слизистой оболочки де- монстрируют признаки дистрофии или атрофии, а в редких случаях подвергаются коагуляционно- му некрозу. Дальнейшее прогрессирование патоло- гического процесса связано с некрозом различных по площади и глубине участков многослойного плоского эпителия с формированием эрозий (эро- зивный рефлюкс-эзофагит), а при более глубо- ких поражениях, вплоть до мышечной оболочки и глубже — язв (язвенный рефлюкс-эзофагит).
Во многих наблюдениях при НЭРБ признаки активно текущего воспаления в слизистой оболочке не обнаруживаются. В других случаях, и особенно при эрозивно-язвенных формах рефлюкс-эзофаги- та, в толще эпителия и в субэпителиальном слое выявляются очаговые (как правило, периваску- лярные и перифокальные к язвенным дефектам), а местами диффузные лимфо-плазмоклеточные инфильтраты с примесью нейтрофильных лейко- цитов и единичных эозинофилов. Воспалительные, некротические или гиперпластические изменения могут распространяться и на пищеводные железы. Появление интраэпителиальных нейтрофильных лейкоцитов и накопление их в воспалительном инфильтрате в сосудисто-стромальных сосочках и в собственной пластинке слизистой оболочки свидетельствует об обострении и прогрессирова- нии воспалительного процесса.
Существенное увеличение количества эозино- фильных лейкоцитов плотностью ≥15 в поле зрения микроскопа при большом увеличении (×400) по крайней мере в одном из биоптатов (около 60 эозинофилов в 1 мм 2), тем более интраэпите- лиальные эозинофильноклеточные микроабсцессы в сочетании с субэпителиальным склерозом соб- ственной пластинки слизистой оболочки, служат критериями диагноза эозинофильного эзофагита [49–53].
При длительном анамнезе ГЭРБ в слизистой оболочке пищевода отмечается разрастание рых- лой, а местами плотной волокнистой соединительной ткани (склероз), как и в дне персистирую- щих эрозий и язв. Базальная мембрана эпителия в большинстве случаев не изменена, но со време- нем также развиваются ее склероз и гиалиноз.
При гистологическом исследовании может быть обнаружена метаплазия многослойного плоского неороговевающего эпителия пищевода с появле- нием на его месте цилиндрического (железистого) эпителия с железами кардиального или фундаль- ного (желудочного) типов. Слизистая оболочка кардиального типа обычно имеет ворсинчатую поверхность, часто отличается короткими ямоч- ными углублениями без правильно сформирован- ных желез (фовеолярный тип), хотя последние могут быть полностью сформированы (железистый тип), но всегда представлены только слизистыми клетками, не содержит париетальных, главных или бокаловидных клеток. При появлении в ней единичных париетальных или главных клеток ее принято называть «слизистая оболочка кардиаль- ного кислотопродуцирующего типа». Слизистая оболочка фундального (желудочного) типа отли- чается наличием в железах большого числа кисло- топродуцирующих париетальных, а также главных клеток, а покровный эпителий формирует иногда типичные валики, покрытые покровно-ямочным эпителием. При цилиндроклеточной метаплазии, особенно кардиального типа, железы нередко рас- положены не регулярно, «сдавлены» разрастани- ями соединительной ткани и диффузным лимфо- плазмоклеточным, с примесью нейтрофильных лейкоцитов инфильтратом.
Принято считать, что при метаплазии слизи- стой оболочки пищевода кардиального, кардиаль- ного кислотопродуцирующего или фундального типов риск развития аденокарциномы пищевода не увеличивается. Однако если проксимальнее 1 см от пищеводно-желудочного соединения мета- плазия приводит к появлению т. н. «специализиро- ванного» эпителия, как в зарубежной литературе часто называют железистый эпителий кишечного типа, то ее расценивают как кишечную метапла- зию (КМ) — предраковый патологический про- цесс, который, в соответствии с большинством рекомендаций, называют пищеводом Баррета. Главным критерием гистологической диагностики КМ является выявление истинных бокаловидных клеток (хотя бы одной такой клетки в пределах биоптата, т. к. изменения слизистой оболочки от- личаются мозаичным характером и очаги КМ обычно локализуются среди слизистой оболочки кардиального типа). Для выявления бокаловид- ных клеток не рекомендуется применять такие гистохимические методы, как, например, ШИК- реакцию и другие, так как, в отличие от мета- плазированной слизистой оболочки желудка, в пищеводе они затрудняют дифференциальную диагностику с псевдобокаловидными клетками. Целесообразность использования иммуногистохи- мических и молекулярно-биологических методов для диагностики КМ не доказана, в частности, из-за отсутствия общепринятой трактовки резуль- татов их применения. Варианты КМ — полный или неполный, прогностического значения не име- ют. Своевременность выявления КМ, а тем бо- лее интраэпителиальной неоплазии (облигатного предракового процесса), во многом зависит от со- блюдения протоколов и точности взятия, а также количества биоптатов слизистой оболочки. Точ- ность диагностики интраэпителиальной неоплазии существенно повышают иммуногистохимический, молекулярно-биологические и генетические мето- ды исследования [11, 54, 55].
В результате регенераторных гиперпластиче- ских процессов новообразованный пласт много- слойного плоского эпителия может накрывать сверху и «замуровывать» участки метаплазии, в том числе и КМ, что при последней не снижает риска развития аденокарциномы пищевода.
• Пациентам с рефрактерным течением забо- левания (отсутствие убедительной клинической и эндоскопической ремиссии в течение 4–8 недель проведения терапии стандартной дозой ИПП), а также пациентам с наличием осложнений заболе- вания (стриктуры, пищевод Баррета) может быть рекомендовано проведение:
- внутрипищеводной суточной рН-метрии или рН-импедансометрии;
- пищеводной манометрии высокого разрешения;
- рентгенологического исследования пищевода и желудка;
- комплексного ультразвукового исследования органов брюшной полости;
- регистрации электрокардиограммы и другие специальные методы (УУР С, УДД — 5).
Рентгенологическое исследование пищевода не применяется с целью непосредственной диа- гностики ГЭРБ, но позволяет обнаружить грыжи пищеводного отверстия диафрагмы (ГПОД), диф- фузный эзофагоспазм, стриктуры пищевода и подо- зрение на короткий пищевод у тех пациентов, ко- торым предполагается хирургическое лечение [56].
• Пациентам с характерными симптомами ГЭРБ, купируемыми приемом ИПП, перед плани- руемым хирургическим лечением рекомендуется проведение суточной рН-метрии для подтвержде- ния воздействия кислоты на слизистую пищевода и оценки взаимосвязи симптома с кислым рефлюк- сом [57] (УУР А, УДД — 1).
В рандомизированном контролируемом иссле- довании при сравнении результатов лапароско- пического антирефлюксного лечения и терапии ингибиторами протонной помпы в течение 5-лет- него наблюдения была достигнута ремиссия у 85 % пациентов после оперативного лечения в услови- ях тщательного подбора группы (эндоскопически подтвержденный эзофагит, повышение % времени рН < 4 и симптоматический ответ на терапию ИПП) [58, 59]. При диагностике ГЭР результаты рН-метрии оценивают по общему времени, в течение которого рН имеет значение менее 4-х единиц, общему числу рефлюксов за сутки, числу реф- люксов продолжительностью более 5 минут, дли- тельности наиболее продолжительного рефлюкса. Процент времени рН < 4 менее 4 % и число ГЭР
* 40 за период суточного мониторирования сле- дует расценивать как вариант физиологической нормы, а более 6 % и 80 эпизодов соответственно свидетельствует в пользу диагноза ГЭРБ, при этом промежуточные значения показателей не служат достаточным критерием для постановки диагноза. Для оценки взаимосвязи симптома с рефлюксом применяют индекс симптома (ИС) и вероятность ассоциации симптома (ВАС), показатели более 50 и 95 % соответственно считают положительными [60, 61].
• При подборе минимально эффективной дозы лекарственных препаратов и контроле эффек- тивности проводимого консервативного лечения больным ГЭРБ может быть выполнена суточная рН-метрия [62] (УУР В, УДД — 3).
Суточная рН-метрия имеет высокую чувстви- тельность (88–95 %) в диагностике ГЭРБ и, кроме того, помогает в индивидуальном подборе лекар- ственных препаратов: определяет эффективность проводимой антисекреторной терапии, лечения ан- тацидами [63–65].
• Пациентам с рефрактерной ГЭРБ для оценки эффективности антисекреторной терапии ГЭРБ без отмены препарата рекомендовано проведе- ние рН-импедансометрии [57, 66–68] (УУР А, УДД — 1).
Импедансометрия пищевода — метод регистра- ции жидких и газовых рефлюксов, основанный на измерении сопротивления (импеданса), которое оказывает электрическому току содержимое, по- падающее в просвет пищевода. Это метод диагно- стики эпизодов рефлюкса в пищевод независимо от значения рН рефлюктата, физического состоя- ния (газ, жидкость), а также определения клиренса болюса, попавшего в пищевод во время рефлюкса. Кислотность рефлюктата (кислый, слабокислый, слабощелочной) определяется рН-датчиками.
Пациентам с установленным ранее диагнозом ГЭРБ с сохраняющимися типичными симптомами и/или отсутствием заживления эрозий на фоне полного курса терапии ИПП в стандартной дозе, в том числе при гипо- и анацидных состояниях (ре- зекция желудка, атрофический гастрит), рекомен- дуется проведение рН-импедансометрии с целью определения связи симптома с рефлюксом (ИС, ВАС), индивидуального подбора антисекретор- ных препаратов, а также коррекции их дозировки и времени приема. Возможно проведение исследо- вания на фоне приема двойной дозы ИПП. У 30 % пациентов на фоне однократного приема препарата сохраняются жалобы на изжогу, а при повышении дозы до 2 раз в сутки — только у 7 % [57, 69].
• Пациентам с атипичными формами и внепи- щеводными проявлениями ГЭРБ (боль в грудной клетке, не связанная с заболеваниями сердечно-со- судистой системы, хронический кашель, бронхи- альная астма, хронический фарингит, ларингит, выраженная отрыжка) рекомендуется проведение консультации специалистов: оториноларинголога, пульмонолога, кардиолога (УУР С, УДД — 5).
• Пациентам с подозрением на внепищеводные проявления ГЭРБ (боль в грудной клетке, не связан- ная с заболеваниями сердечно-сосудистой системы, хронический кашель, бронхиальная астма, хрони- ческий фарингит, ларингит, выраженная отрыжка) рекомендовано проведение рН-импедансометрии [57, 65, 67] (УУР А, УДД — 1).
В течение 5-летнего проспективного мульти- центрового открытого когортного исследования ProGERD, включавшего 6215 больных, данные о наличии внепищеводных проявлений ГЭРБ были получены в 32,8 % случаев, причем распростра- ненность достоверно выше наблюдалась в группе больных эрозивной формой заболевания (30,5 % НЭРБ против 34,9 % ЭРБ, р = 0,0002, ОШ = 1,22
(1,09; 1,35)). Ларингеальные симптомы выявля- лись у 10,4 % больных, и также чаще наблюдались в группе ЭРБ (р = 0,0234, ОШ = 1,21 (1,03; 1,42))
[70]. Внепищеводные симптомы ГЭРБ обусловле- ны ларингофарингеальным рефлюксом (ЛФР) [71]. Симптомы у больных с ЛФР в большей сте- пени обусловлены персистенцией слабокислых и слабощелочных, нежели кислых, высоких реф- люксов [67, 72].
Для диагностики ЛФР рекомендуется примене- ние комбинированного рН-импедансометрического зонда с расположением одного рН-датчика в же- лудке и двух в пищеводе, а также измерительных импедансных (Z) сегментов в пищеводе. Именно наличие проксимального рН-датчика в пищеводе в комбинации с Z-датчиками в области верхнего пищеводного сфинктера обуславливает диагности- ческую ценность исследования в отношении ЛФР [73, 74]. Требуется дальнейшая стандартизация интерпретации полученных результатов [60].
Супрагастральная отрыжка может быть са- мостоятельным функциональным заболеванием (синдром чрезмерной отрыжки), а может быть проявлением основного заболевания (ГЭРБ, функ- циональной диспепсии и др.) [75]. Так, среди па- циентов с диагностированной супрагастральной отрыжкой до 95 % предъявляют жалобы на изжо- гу, а повышение % времени рН < 4 при проведе- нии рН-импедансометрии выявляется у 41 % боль- ных [76].
• Пациентам с типичными клиническими про- явлениями (изжога) без выраженных эндоскопиче- ских изменений и c нормальной морфологической картиной СО пищевода может быть рекомендова- но проведение рН-импедансометрии [77] (УУР А, УДД — 1).
У пациентов с типичными проявлениями, ха- рактерными для ГЭРБ, исследование позволя- ет провести дифференциальный диагноз между НЭРБ, функциональной изжогой, гиперсенситив- ным рефлюксным синдромом (или гиперсенситив- ным пищеводом), а в случае с подтвержденной ра- нее ГЭРБ исключить их сочетание [78, 79].
• Пациентам перед планируемым оператив- ным лечением ГЭРБ рекомендовано проведение рН-импедансометрии [67] (УУР А, УДД — 1).
Мониторирование показано с целью выявления не только кислых, но и слабокислых, слабощелоч- ных ГЭР и подтверждения их связи с возникно- вением симптомов. Показаниями для проведения хирургического лечения служат наличие сим- птомов, связь которых доказана при проведении рН-импедансометрии с ГЭР, причем лучший ре- зультат достигается у пациентов, отвечающих на те- рапию ИПП [80]. Пациентам с симптомами ГЭРБ и нормальными показателями рН-импедансометрии от проведения оперативного лечения следует воз- держаться [81].
• Пациентам после антирефлюксных опера- ций для оценки эффективности хирургическо- го лечения при сохраняющихся симптомах забо- левания может быть рекомендовано проведение рН-импедансометрии [67] (УУР А, УДД — 1).
Большинство пациентов, прошедших тщатель- ное предоперационное обследование [81], после проведенной фундопликации имеют высокое ка- чество жизни. Тем не менее есть доля больных с сохраняющимися симптомами. Существует сла- бая корреляция между симптомами, характерны- ми для ГЭР, и фактически диагностируемым реф- люксом: 68 % пациентов, принимавших по поводу изжоги после оперативного лечения препараты, снижающие кислотность, имели нормальный % времени рН < 4 по данным рН-метрии [82]. Па- циентам с симптомами после антирефлюксно- го хирургического лечения должна проводиться pH- импедансометрия, что позволяет объектив- но исключить кислый ГЭР, а также другие при- чины симптомов, такие как некислый рефлюкс или супрагастральную отрыжку. Фундопликация изменяет численное соотношение типов отрыжки, уменьшая частоту физиологической гастральной отрыжки. Это побуждает пациентов воспроизво- дить супрагастральную отрыжку в попытке осво- бодить желудок от воздуха [83].
• Пациентам с сохраняющимися симптомами рекомендуется проведение рН-импедансометрии как на фоне приема антисекреторных препаратов, так и с их отменой [61] (УУР А, УДД — 1).
Пациентам с сохраняющимися типичными сим- птомами с доказанной ранее ГЭРБ по данным эн- доскопического исследования (эзофагитом степени С–D, пищеводом Баррета или пептической стрик- турой) и рН-метрии рекомендуется проведение рН-импедансометрии на фоне терапии ИПП, по- скольку это позволяет установить эффективность действия антисекреторного препарата, оценить связь симптома с наличием кислого, слабокислого или слабощелочного рефлюкса. Количественный анализ данных рН-импедансометрии позволяет ис- ключить сочетание ГЭРБ с функциональной изжо- гой и гиперсенситивным рефлюксным синдромом [77, 84]. Если у пациента ранее не доказано нали- чие ГЭРБ или данные неубедительны, то суточный мониторинг проводится с отменой препарата с це- лью определения патологического воздействия кис- лоты на слизистую оболочку пищевода ( % времени рН < 4), числа ГЭР, их химических и физических характеристик, высоты распространения и связи симптомов с ГЭР [57, 60, 61, 85].
При анализе импедансометрии следует рассчи- тывать дополнительные новые параметры: средний ночной базальный импеданс (СНБИ) и индекс пост-рефлюксной глоток индуцированной пери- стальтической волны (ПГПВ), позволяющие оце- нить клиренс пищевода, особенности поражения его слизистой оболочки (снижение ее резистентно- сти) и эффективность перистальтики [61]. Новые параметры служат дополнительными критериями, повышающими диагностическую ценность импе- дансометрии в постановке диагноза и определении формы ГЭРБ. Снижение уровня данных показате- лей у пациентов отражает вероятность более тяже- лого течения заболевания [86].
СНБИ — параметр, определяющий средний уро- вень базального импеданса СО, снижение которо- го отражает рефлюкс-индуцированное нарушение структурной целостности СО пищевода и сниже- ние ее тканевой резистентности даже при отсут- ствии макроскопических повреждений, в том числе на фоне нарушения двигательной функции стенки пищевода [87]. Индекс ПГПВ — параметр оценки химического пищеводного клиренса и эффектив- ности двигательной функции пищевода. Может рассматриваться как дополнительный критерий дифференциальной диагностики между эрозивной и неэрозивной формами заболевания [88].
• Пациентам с ГЭРБ для исследования двига- тельной функции пищевода может быть рекомен- довано проведение манометрии высокого разреше- ния (МВР) [89, 90] (УУР А, УДД — 1).
Совместное применение с импедансометрией расширяет диагностические возможности маноме- трии [57, 91]. Комбинированная импеданс-мано- метрия позволяет визуализировать транзит болюса по пищеводу и эффективность перистальтики, вы- являть тип отрыжки (гастральная, супрагастраль- ная), определять, является ли она проявлением основного заболевания или самостоятельным син- дромом, что дает возможность назначать патогене- тическую терапию [75].
При обследовании пациентов с ГЭРБ методом МВР рекомендуется придерживаться единой клас- сификации нарушений двигательной функции пи- щевода. В основе трехступенчатой классификации лежит пошаговый алгоритм анализа морфологии пищеводно-желудочного перехода и давления соб- ственно НПС, исследования моторики грудного отдела пищевода, направленного на выявление нормальной, фрагментированной, неэффективной перистальтики или ее отсутствия. При выявлении нарушенной перистальтики рекомендуется прове- дение дополнительных тестов для оценки сократи- тельной способности пищевода, в том числе теста быстрых глотков [92].
При анализе результатов, полученных методом МВР, следует пользоваться Чикагской классифи- кацией нарушений моторики пищевода [27, 90, 93–96].
• Пациентам с ГЭРБ для определения наличия показаний к проведению хирургического лече- ния, установления патогенеза развития симптомов ГЭРБ может быть рекомендовано изучение морфо- логии пищеводно-желудочного перехода (ПЖП) с помощью МВР (УУР С, УДД — 5).
Согласно принятым положениям выделяют три типа ПЖП, из которых I тип составляет физио- логическую норму, II тип — переходное состояние (начальный этап сепарации НПС и ножек диафраг- мы), а III тип соответствует диагнозу ГПОД. До- казано, что при II и III морфологических типах ПЖП у больных ГЭРБ рефлюкс регистрируется достоверно чаще. При выявлении деструктуриза- ции ПЖП не менее 2 см, когда пациент по тем или иным объективным или субъективным причи- нам не может получать консервативную терапию ГЭРБ, следует рассмотреть вопрос о хирургиче- ском лечении в условиях специализированного стационара при отсутствии противопоказаний [81, 92, 93, 97].
• Пациентам с ГЭРБ для прогнозирования тя- жести течения и возникновения осложнений забо- левания рекомендуется диагностика эффективно- сти перистальтической активности грудного отдела пищевода с помощью МВР (УУР С, УДД — 5).
У больных ГЭРБ чаще, чем в популяции, диа- гностируют гипомоторные дискинезии пищевода: неэффективную, фрагментированную перисталь- тику или ее полное отсутствие. Доказано, что толь- ко тяжелая форма неэффективной перистальтики (≥70 % неэффективных глотков) у ряда пациентов может привести к нарушению транзита болюса, за- медлению пищеводного клиренса. В этой группе пациентов чаще регистрируется повышение % вре- мени рН < 4, более значительное в ночное время, что доказано при проведении рН-импедансометрии, а по данным ЭГДС диагностируются более тяже- лые формы эзофагита, пищевод Баррета [98, 99].
Отсутствие перистальтики — самая тяжелая форма гипомоторной дискинезии пищевода и сопряжена с наиболее тяжелым течением ГЭРБ. Ди- агностируется у 3,2 % пациентов, направленных на хирургическое лечение [92, 99].
• Всем пациентам с ГЭРБ перед планируемым хирургическим антирефлюксным лечением реко- мендуется проведение манометрии пищевода высо- кого разрешения [81] (УУР А, УДД — 1).
Проведение МВР, в том числе в комбина- ции с импедансометрией, позволяет исключить состояния, симптоматически имитирующие ГЭРБ, например ахалазию кардии, синдром руминации, отрыжку [81, 92].
Пациентам с гиперконтрактильным пищеводом, функциональной болью в грудной клетке, ГЭРБ с нормальной функцией ПЖП хирургическое ле- чение не показано. Более того, наличие в доопера- ционном периоде гипермоторной дискинезии мо- жет быть предиктором развития боли в грудной клетке после фундопликации [81].
При выявлении неэффективной перистальтики пищевода необходимо проведение исследования ре- зерва сократительной способности пищевода (тест быстрых глотков) с целью оценки риска развития возникновения осложнений в постоперационном периоде после антирефлюксного хирургического лечения, в частности прогрессирования ослабления перистальтики и развития дисфагии [92, 93].
Определение резерва сократительной способно- сти пищевода методом теста быстрых глотков ре- комендуется проводить в дополнение к основному протоколу МВР, в том числе перед оперативным лечением [100]. Отсутствие резерва сократитель- ной активности пищевода, особенно у пациентов с неэффективной перистальтикой, может служить предиктором увеличения времени пищеводно- го клиренса и % времени с рН < 4, нарушения транзита болюса, в постоперационном периоде развития обструкции ПЖП и прогрессирования ослабления перистальтики [62, 64, 65, 68]. При ди- агностике неэффективной перистальтики, сопрово- ждающейся отсутствием резерва сократительной способности пищевода, рекомендуется пересмо- треть/адаптировать объем проводимого хирур- гического вмешательства в каждом конкретном случае, чтобы минимизировать риск развития по- стоперационной дисфагии [81, 101].
Отсутствие перистальтики пищевода можно рассматривать как относительное противопоказа- ние для проведения хирургического антирефлюкс- ного лечения [102].
• Пациентам с ГЭРБ после антирефлюксной хи- рургии для оценки эффективности хирургического лечения (определение состоятельности фундопли- кационной манжеты, исключение рецидива ГПОД) и возможных осложнений (при жалобах на дисфа- гию) может быть рекомендовано проведение мано- метрии пищевода [90] (УУР С, УДД — 3).
При сохранении жалоб или их рецидиве после проведенного оперативного лечения следует про- верить функционирование фундопликационной манжеты для исключения необходимости повторного вмешательства вследствие ее несостоятель- ности, а также выявления других причин перси- стенции симптомов. Предложены нормативные значения для постоперационной оценки проходи- мости ПЖП [103].
• Пациентам с ГЭРБ для определения уров- ня расположения НПС перед установкой зон- да для рН/рН-импедансометрии рекомендуется
проведение манометрии пищевода [57] (УУР А, УДД — 1).
Следует устанавливать рН-датчик на уровне 5 см выше края НПС, что минимизирует его сме- щение в желудок во время глотков. Манометрия пищевода является предпочтительным методом, с помощью которого локализуется уровень верх- него края НПС. При контрольной флюороскопии точность установки рН-датчика подтверждается в 95 % случаев [104].
2.3. Иные диагностические исследования
В диагностике ГЭРБ может быть использован такой метод, как импедансная планиметрия [105– 107].
Внедрение методов эндоскопии высокого разре- шения (HD), узкоспектральной эндоскопии (NBI), увеличительной эндоскопии, в том числе — в со- четании с NBI, помогает обнаружить метапла- стические и диспластические изменения эпителия пищевода с целью прицельного взятия биопсии для гистологического исследования [108–110]. При выявлении метаплазированного эпителия в пи- щеводе все большее значение приобретает метод эн- доцитоскопии — осмотра окрашенной 1 %-ным рас- твором метиленового синего с увеличением ×520, позволяющий верифицировать диагноз пищевода Баррета и дисплазии эпителия без выполнения би- опсии [111–113]. Эндоскопическое ультразвуковое исследование пищевода (эндосонография) служит основной методикой, позволяющей выявлять эн- дофитно растущие опухоли и признаки ахалазии (УУР С, УДД — 5).
3. Лечение, включая медикаментозную
и немедикаментозную терапию, диетотерапию
Лечение пациентов ГЭРБ должно быть индивидуализировано в соответствии с клинически- ми проявлениями заболевания и интенсивностью симптомов. Цель лечения — устранение симптомов, а при эрозивном эзофагите — заживление эрозий и предупреждение осложнений. У пациен- тов с пищеводом Баррета целью является профилактика прогрессирования и развития дисплазии и АКП [114].
следования, проведенные во многих странах мира, по- казали, что более чем у 80 % пациентов, не полу- чающих адекватного поддерживающего лечения, рецидив развился в течение ближайших 26 недель, а в течение года вероятность рецидива составляет 90–98 %. Из этого следует обязательная необходи- мость поддерживающего лечения [115, 116].
Лечение ГЭРБ должно быть комплексным и включать в себя не только назначение лекар- ственных препаратов, но и проведение широкого круга различных мероприятий: диетическое пита- ние, прекращение курения и злоупотребления ал- коголем, отказ от приема препаратов, обладающих повреждающим действием на слизистую оболочку пищевода и снижающих барьерную функцию пи- щеводно-желудочного перехода, нормализацию режима труда и отдыха, санаторно-курортное ле- чение.
Пациенты с неосложненным течением ГЭРБ подлежат консервативному лечению. В большин- стве случаев оно проводится амбулаторно. Од- нако при развитии осложнений, необходимости дообследования с целью верификации диагноза (например, при рефрактерном течении), тяжелых сопутствующих заболеваниях целесообразна го- спитализация пациентов.
3.1. Диетотерапия и изменение образа жизни
• Всем пациентам с ГЭРБ рекомендуется из- менение образа жизни (снижение массы тела при ее избытке, прекращение курения, избегание ситуаций, повышающих внутрибрюшное давление) и диетотерапия (УУР С, УДД — 5).
Изменение образа жизни следует считать обя- зательной предпосылкой эффективного антиреф- люксного лечения пациентов с ГЭРБ. В первую очередь необходимо снизить массу тела, если она избыточна [117], и прекратить курение [118, 119]. Пациентам следует избегать переедания; они долж- ны прекратить прием пищи за два часа до сна [120]. В то же время не следует увеличивать число приемов пищи: необходимо соблюдать трех-, четы- рехразовое питание и тщательно избегать так на- зываемых «перекусов». Рекомендации по частому дробному питанию не обоснованы.
Важно максимально избегать ситуаций, повы- шающих внутрибрюшное давление (ношения тугих поясов, корсетов и бандажей, поднятия тяжестей более 8–10 кг на обе руки, работ, сопряженных с наклоном туловища вперед, физических упраж- нений, связанных с перенапряжением мышц брюш- ного пресса). Поднятие изголовья кровати необхо- димо для пациентов, которых беспокоит изжога или регургитация в лежачем положении [121, 122]. Диетические рекомендации должны быть строго индивидуальны с учетом тщательного анализа анамнеза пациента. Целесообразно избегать упо- требления томатов в любом виде, кислых фрук- товых соков, продуктов, усиливающих газообра- зование, а также жирной пищи, шоколада, кофе. Необходимо максимально ограничить употребле- ние алкоголя, очень горячей или холодной еды и газированных напитков [118].
Больных нужно предупредить о побочном действии препаратов, которые снижают тонус НПС (нитраты, антагонисты кальция группы нифеди- пина, теофиллин, прогестерон, антидепрессанты), а также могут сами явиться причиной воспаления (нестероидные противовоспалительные средства, доксициклин, хинидин) [123].
3.2. Консервативное лечение
Антациды и алгинаты могут применяться как в качестве монотерапии редкой изжо- ги, не сопровождающейся развитием эзофагита, так и в схемах комплексной терапии ГЭРБ, так как оказываются эффективны в быстром устранении симптомов [124, 125] (УУР А, УДД — 1).
Антацидные средства — алюминия фосфат 2,08 г, комбинированные препараты — магалдрат 400 или 800 мг и симетикон 20 или 40 мг, алюминия гидроксид 400 мг и магния гидроксид
400 мг применяют в лечении умеренно выражен- ных и нечасто возникающих симптомов, особенно тех, которые связаны с несоблюдением рекомендо- ванного образа жизни [124, 126–128].
Комбинированный препарат, содержащий ма- галдрат и симетикон, способен быстро нейтрализо- вать соляную кислоту и длительно поддерживать стабильный уровень pH, очень активно связывать соли желчных кислот [125]. При его применении наблюдается исчезновение симптомов у большин- ства пациентов с ГЭРБ [129] (УУР А, УДД — 1). Алгинаты, создавая защитный барьер на по- верхности желудочного содержимого, способны уменьшать количество гастроэзофагеальных и ду- оденогастроэзофагеальных рефлюксов [130]. До- казана фармакологическая совместимость данных средств с антисекреторными препаратами для лечения ГЭРБ [130–132] (УУР А, УДД — 1).
Антациды и алгинаты следует принимать в зависимости от выраженности симптомов обычно после еды и на ночь до стойкого купирования симптомов заболевания, затем «по требованию». Данных, свидетельствующих о возможности их постоянного применения, недостаточно [133, 134] (УУР В, УДД — 2).
|
Эзофагопротекторы |
— |
новая |
фармакологи- |
|
ческая группа, представителем которой является биоадгезивная формула на основе гиалуроновой кислоты и хондроитина сульфата для защиты сли- зистой оболочки. Комбинация натрия гиалуроната и хондроитина сульфата натрия обеспечивает за- щиту слизистой оболочки желудка и пищевода. Наличие в составе компонента Полоксамер 407, обладающего высокой способностью к биоадгезии, обеспечивает надежный контакт комплекса гиа- луроновая кислота — хондроитина сульфат с по- верхностью стенки пищевода, способствуя ее защи- те от агрессивного воздействия соляной кислоты желудка. Хондроитина сульфат также способству- ет восстановлению слизистой оболочки пищево- да и желудка. Биоадгезивная формула на основе гиалуроновой кислоты и хондроитина сульфата для защиты слизистой оболочки способствует сни- жению воспаления и заживлению эрозий пищево- да, в том числе при комбинированном применении | |||
Прокинетики. Возможности применения про- кинетиков при лечении ГЭРБ обусловливаются их способностью влиять на важные звенья патогенеза заболевания. Они способствуют восстановлению нормального физиологического состояния пищево- да, уменьшая количество ПРНПС, улучшая пище- водный клиренс за счет стимуляции двигательной функции нижележащих отделов пищеваритель- ного тракта. Прокинетики повышают тонус НПС и ускоряют эвакуацию из желудка. Наибольший эффект они оказывают при сочетании ГЭРБ и ФД [145].
• Прокинетики могут применяться в составе комплексной терапии ГЭРБ вместе с ИПП [146– 152] (УУР А, УДД — 1).
Важную роль в патогенезе ГЭРБ играют нару- шения моторики пищевода и желудка: увеличение числа преходящих расслаблений нижнего пищевод- ного сфинктера, снижение пищеводного клирен-са, повышение внутрижелудочного давления. Эти факторы, а также наблюдающийся в ряде случаев некислотный характер рефлюктата, оправдывают применение прокинетиков в лечении данного забо- левания [145]. Метаанализ 12 рандомизированных контролируемых исследований, посвященных при- менению прокинетиков при ГЭРБ и включавших 2403 пациента, показал, что добавление прокине- тиков к ИПП способствовало более существенному уменьшению выраженности клинических симпто- мов и числа эпизодов рефлюкса [147].
Прокинетический препарат итоприда гидрох- лорид 50 мг 3 раза в день относится к средствам патогенетического лечения ГЭРБ, поскольку нор- мализует двигательную функцию верхних отделов пищеварительного тракта, уменьшает количество преходящих расслаблений нижнего пищеводногосфинктера [148–151]. При использовании ито- прида в составе комбинированной терапии с ИПП при ГЭРБ обнаружено, что он достоверно усилива- ет сократительную активность НПС, усиливает мо- торику желудка, желудочной эвакуации и восста- новление гастродуоденальной координации [149, 153] и оказывает достоверное влияние на купиро- вание изжоги [154]. Итоприд в комбинации с рабе- празолом доказано улучшает клиническое течение хронического кашля, обусловленного ГЭРБ [155].
Препарат тримебутин в дозе 100–200 мг 3 раза в день применяется для купирования изжоги и отрыжки при лечении неэрозивной рефлюксной болезни. Он нормализует скорость опорожнения желудка у пациентов с его замедленным опо- рожнением: время от момента поступления пищи в желудок до начала эвакуации пищи из желуд- ка существенно уменьшается [156, 157]. Тримебу- тин способствует более выраженному купирова- нию эзофагита и симптоматики ГЭРБ в сочетании с ИПП, чем при монотерапии ИПП. При такой комбинации полное купирование симптоматики на- блюдается достоверно чаще [158]. Также отмечено более выраженное действие комбинации тримебу- тина и ИПП по сравнению с монотерапией ИПП, в отношении нормализации показателей качества жизни и суточного мониторирования рН в пище- воде [159, 160]
• При наличии как пищеводных, так и внепи- щеводных проявлений ГЭРБ эффективно назначение ингибиторов протонной помпы.
Ингибиторы протонной помпы (ИПП) — это препараты, подавляющие активность фермента Н+, К+-АТФазы, находящегося на апикальной мембране париетальной клетки и осуществляю- щего последний этап синтеза соляной кислоты. На сегодняшний день ИПП считаются наиболее эффективными препаратами для лечения ГЭРБ. В клинических исследованиях ИПП постоян- но демонстрируют наибольшую эффективность в лечении эрозивного эзофагита и купировании ГЭРБ-ассоциированных симптомов [133, 134] (УУР А, УДД — 1). Снижение кислотной про- дукции считается основным фактором, способствующим заживлению эрозивно-язвенных пора- жений. При наличии единичных эрозий пищевода (А степень) вероятность их заживления в тече- ние 4 недель лечения высока. Поэтому основной курс в данном случае, может составлять 4 недели с использованием стандартной дозы ИПП (рабе- празол в дозе 20 мг в день [161–163] (УУР А, УДД — 1), или эзомепразол 40 мг в день [111, 164] (УУР А, УДД — 1), или омепразол в дозе 20 мг 2 раза в день, или декслансопразол в дозе 60 мг [165–168] (УУР А, УДД — 1), или пантопразол 40 мг в день) желательно с проведени-
ем контрольного эндоскопического исследования. При выявлении множественных эрозий пищевода (В–D степени эзофагита), а также осложнений ГЭРБ, курс лечения любым препаратом из группы ИПП должен составлять не менее 8 недель, так как при такой продолжительности терапии можно добиться 90–95 % эффективности. При необосно- ванном сокращении курса лечения множествен- ных эрозий пищевода до 4-х недель частота их заживления оказывается значительно ниже. Кро- ме того, такое необоснованное сокращение сроков лечения эрозивных форм ГЭРБ может быть при- чиной быстрого последующего рецидивирования, а также развития осложнений [115, 116]. Пациен- там с типичным симптомокомплексом рефлюкса, которые не дают адекватного ответа на терапию ИПП в стандартной дозе один раз в день, может быть рекомендован прием ИПП дважды в день. При этом следует учитывать, что данная дозиров- ка не утверждена в инструкциях по применению данных препаратов. Поддерживающую терапию после заживления эрозий следует проводить, как минимум, в течение 16–24 недель. При на- личии осложнений ГЭРБ поддерживающую тера- пию следует проводить ингибиторами протонной помпы также в полной дозе [169–171] (УУР А, УДД — 1).
ИПП эффективно контролируют уровень рН в нижней трети пищевода, поэтому выраженность симптомов быстро уменьшается, и они исчеза- ют у пациентов как с эрозивным эзофагитом, так и неэрозивной рефлюксной болезнью. В отсутствие эрозий пищевода для лечения НЭРБ возможно на- значение половинной дозы ИПП: в том числе, ра- бепразола в дозе 10 мг один раз в день при курсо- вом лечении, а также при приеме по требованию, что является фармакоэкономически оправданным [172–174] (УУР А, УДД — 1), а также декслансо- празола 30 мг один раз в день [175, 176] (УУР А, УДД — 1).
Рекомендуется применять индивидуальный подход к назначению антисекреторной терапии и выбору препарата при лечении больных ГЭРБ, основанный на тщательном анализе клинической картины и данных эзофагогастродуоденоскопии. В первую очередь, анализируются жалобы больно- го, в частности изжога (кроме изжоги могут при- ниматься во внимание и другие доказанные сим- птомы ГЭРБ). Критериями оценки жалоб служат: частота их возникновения: редко (1–2 р/нед.) и часто (>2 р/нед.), а также длительность суще- ствования: небольшая (<6 месяцев) и значитель- ная (>6 месяцев). При оценке статуса пациента и анамнеза учитываются мужской пол и возраст старше 50 лет как факторы риска развития реци- дива, указания на наличие эрозивного эзофагита при проведении ЭГДС в прошлом, причем суще- ственное значение имеет степень существовавшего ранее эрозивного эзофагита. При оценке статуса больного также следует обратить внимание на на- личие избыточной массы тела (ИМТ > 25) и ожи- рения (ИМТ > 30) и грыжи пищеводного отвер- стия диафрагмы. Необходимо исключить наличие симптомов тревоги: дисфагии, похудания, анемии.
Следует учитывать особенности отдельных антисекреторных препаратов. Блокаторы Н2 ре- цепторов не должны использоваться в качестве терапии первой линии в связи с гораздо меньшей эффективностью по сравнению с ИПП [177].
Благодаря высокой константе диссоциации рКа, рабепразол способен быстро аккумулировать- ся в большом числе париетальных клеток и при- водить к быстрому и выраженному торможению секреции кислоты, ингибируя протонную помпу, что обеспечивает высокую скорость действия и по- зволяет достичь стойкого антисекреторного эф- фекта уже после первых суток приема препарата [178–182]. Фармакокинетические особенности ра- бепразола обуславливают эффективное купирова- ние дневной и контроль ночной изжоги с первого дня терапии [183, 184], высокую частоту зажив- ления эрозий пищевода [172] и поддержания дли- тельной ремиссии ГЭРБ, в том числе при приеме по требованию [163, 183, 184] (УУР A, УДД — 1). Эзомепразол благодаря стереоселективным особенностям взаимодействия с цитохромом P450 обладает большой биодоступностью и пред- сказуемым контролем секреции соляной кислоты [185], длительно поддерживая уровень рН > 4, что обеспечивает эффективность терапии НЭРБ и эрозивного эзофагита [164, 186–191]. Лекар- ственная форма таблетки эзомепразола MUPS (мультипартикулярная система доставки), покры- той кислотоустойчивой оболочкой, обеспечивает быстрое и предсказуемое всасывание независимо от приема еды. Возможность растворения в воде таблетки MUPS может быть удобна пациентам с дисфагией и при использовании через назгогастральный зонд [192, 193].
Декслансопразол — единственный ИПП с мо- дифицированным высвобождением активного ве- щества. Его капсула включает два типа гранул, высвобождающих активное вещество в зависи- мости от pH в разных областях тонкой кишки через 1–2 часа и через 4–5 часов после приема препарата [194–197]. Двойное отсроченное высво- бождение активного вещества позволяет пролон- гировать его действие и способствует снижению секреции соляной кислоты в течение продолжи- тельного времени. Пролонгирование эффекта декс- лансопразола способствует эффективному контро- лю ночных симптомов ГЭРБ [198, 199] (УУР A, УДД — 1).
В целом ИПП демонстрируют невысокую ча- стоту побочных эффектов (<2 %), среди которых могут наблюдаться диарея, головная боль, тошнота [200, 201]. При назначении ИПП в больших до- зах на длительный срок следует также учитывать возможность развития таких побочных эффектов, как остеопороз (хотя применение ИПП не долж- но рассматриваться как самостоятельный и неза- висимый фактор риска развития остеопороза [202, 203]), избыточный бактериальный рост, инфекция Clostridium difficile и пневмония среди пациентов из групп риска, в первую очередь старше 65 лет [204–206]. При длительном лечении ИПП воз- можно назначать по требованию и прерывистыми курсами [207, 208]. Решение о длительности под- держивающей терапии ГЭРБ и об ее отмене долж- но приниматься индивидуально с учетом стадии эзофагита, имеющихся осложнений, возраста па- циента, прогноза заболевания, а также стоимости и безопасности лечения ИПП. Рабепразол демон- стрирует высокий уровень безопасности в отноше- нии частоты побочных эффектов и переносимости, а его метаболизм минимально зависит от систе- мы цитохрома 450 [161, 173, 209], что позволя- ет рекомендовать его в качестве препарата выбора у полиморбидных пациентов, минимизируя риск межлекарственного взаимодействия, что важно при необходимости длительных курсов (пищевод Баррета, эрозивный эзофагит C/D) [210–212] (УУР А, УДД — 1).
Нет необходимости определения инфекции
H. pylori и, тем более, ее эрадикации при ГЭРБ. Однако следует определить наличие инфекции
H. pylori и провести ее эрадикацию при назначе- нии терапии ИПП на длительный срок [213].
Необходимо особо подчеркнуть то, что симптоматическое улучшение при терапии ИПП может иметь место и при других заболеваниях, в том числе злокачественном новообразовании желуд- ка, поэтому необходимо исключить такие заболе- вания.
При осложненных формах ГЭРБ возможно применение коротких курсов внутривенных форм ИПП, преимуществами которых является быстрое достижение антисекреторного эффекта и более высокая концентрация препарата в крови.
Термин «рефрактерная ГЭРБ» используют в случае неполного заживления слизистой обо- лочки пищевода и/или сохранения типичных симптомов ГЭРБ после проведения полного курса (4–8 недель) лечения стандартной (один раз в сут- ки) дозой ИПП [214, 215].
Наиболее распространенной причиной, при- водящей к уменьшению эффекта от проводимой терапии, является недостаточная приверженность больных к лечению, то есть несоблюдение паци- ентами рекомендаций по изменению образа жизни и правилам приема ИПП. На соблюдение (или несоблюдение) предписанных врачом рекоменда- ций влияет, прежде всего, наличие симптомов и их тяжесть, знание основ патогенеза заболевания, сопутствующая терапия, побочные эффекты, воз- раст, социально-экономический статус, мотивация больного. Безусловно, выполнение рекомендаций врача, в том числе по режиму питания, нормали- зации массы тела, следует считать фундаментом успешного лечения. Неэффективность терапии нередко наблюдается также при неправильном на- значении и несоблюдении дозировки ИПП и сро- ков терапии [216].
Фактором развития рефрактерной ГЭРБ яв- ляется генетический полиморфизм CYP2C19. Быстрые метаболизаторы CYP2C19 имеют по- вышенный риск рефрактерности к терапии ИПП по сравнению с медленными метаболизаторами. В настоящее время выделен еще один тип мета- болизаторов по изоферменту CYP2C19, названный «ультрабыстрым», который может встречаться в европейской популяции. В отдельных случаях такие больные нуждаются в применении высоких доз антисекреторных препаратов, что должно быть верифицировано с помощью 24-часовой рН-метрии [217, 218].
Cекреция муцинов в слизи при ГЭРБ снижа- ется в зависимости от тяжести эзофагита [31–33], что является дополнительным фактором, пред- располагающим к развитию эрозивного эзофагита в условиях продолжающегося гастроэзофагеально- го рефлюкса. Двойной механизм действия рабепра- зола — кислотосупрессия наряду с цитопротектив- ными свойствами: стимуляция секреции муцинов и повышение их концентрации в слизи пищевода, обеспечивает его дополнительные терапевтические преимущества [219, 220] (УУР C, УДД — 4).
Действие ребамипида, заключающееся в ре- гуляции синтеза простагландинов через ЦОГ-2 опосредованные механизмы, влиянии на ЭФР, повышении экспрессии белков плотных межкле- точных контактов в эпителиальных клетках СО, снижении уровня ИЛ-8 и свободных радикалов кислорода, направлено на защиту слизистой обо- лочки желудочно-кишечного тракта и восстанов- ление ее естественных барьерных свойств. Со- гласно данным ряда клинических исследований, эффективность комбинации ИПП и ребамипида способствует большему регрессу жалоб у пациен- тов с ГЭРБ и меньшей частоте рецидивов заболе- вания, чем при монотерапии ИПП. В настоящее время проводится активное изучение и выработ- ка рекомендаций по методике применения ре- бамипида у пациентов с ГЭРБ, что оправдано ввиду наличия у этого препарата уникального механизма действия, направленного на устра- нение основных этапов патогенеза заболевания, существенно увеличивающего эффективность ле- чения ГЭРБ [221].
Причиной неэффективности ингибиторов секре- ции соляной кислоты может быть наличие слабо- кислого рефлюкса, а также преобладание в реф- люктате содержимого двенадцатиперстной кишки с преимущественно щелочной средой, когда изжога и другие симптомы ГЭРБ возникают в результате действия на слизистую оболочку пищевода компо- нентов желчи и панкреатических ферментов.
Компоненты дуоденального содержимого, повреждаю- щие слизистую оболочку пищевода, представлены желчными кислотами, лизолецитином и трипси- ном. Из них наиболее хорошо изучена роль желч- ных кислот, которым, по-видимому, принадлежит основная роль в патогенезе повреждения пище- вода при дуоденогастроэзофагеальном рефлюксе (ДГЭР).
При смешанном рефлюксе (кислый с желчным компонентом) ИПП оказывают клинический эф- фект не только вследствие подавления собственно кислотопродукции, но и за счет уменьшения обще- го объема желудочного секрета, что ведет к умень- шению объема рефлюктата. Однако повышение доз ИПП с целью купирования симптоматики в таком случае не показано.
прокинетики, урсодезоксихолевая кислота, реба- мипид (УУР С, УДД — 4).
При неэффективности лечения пациентов с ГЭРБ в течение 4 недель следует провести под- тверждение наличия гастроэзофагеального реф- люкса с помощью объективного метода исследова- ния 24-часовой рН-импедансометрии [43, 222].
Пациенты с сохраняющимися симптомами, у ко- торых при проведении рН-импедансометрии не обнаруживаются патологические рефлюксы и отсут- ствует корреляция рефлюксов с возникновением симптомов, скорее всего, страдают не ГЭРБ, а так называемой «функциональной изжогой» [223].
3.3. Хирургическое лечение
Антирефлюксное хирургическое лечение счи- тается показанным при осложненном течении за- болевания (повторные кровотечения, пептические стриктуры пищевода, развитие пищевода Баррета с дисплазией эпителия высокой степени, доказан- ной двумя морфологами, частые аспирационные пневмонии). В некоторых случаях, когда пациент по тем или иным объективным или субъективным причинам не может получать консервативную те- рапию ГЭРБ, следует рассмотреть вопрос о хирур- гическом лечении и при неосложненном течении. Хирургическое лечение ГЭРБ может быть более эффективным у тех пациентов ГЭРБ, у которых имеются типичные проявления ГЭРБ и их лече- ние с помощью ИПП тоже эффективно [59, 224]. При неэффективности ИПП, а также при внепище- водных проявлениях хирургическое лечение также будет менее эффективным.
Рассматривать вопрос об оперативном лечении нужно лишь совместно с опытным в данной об- ласти хирургом, если выполнены все меропри- ятия по нормализации образа жизни, доказано (с помощью рН-импедансометрии) наличие пато- логического желудочно-пищеводного рефлюкса, а с помощью манометрии пищевода отсутствие больших дефектов перистальтики грудного отде- ла пищевода.
4. Профилактика и диспансерное наблюдение, медицинские показания и противопоказания к применению методов профилактики
• Диспансерное наблюдение пациентов с эзофагитом без пищевода Баррета рекомендуется прово- дить 1 раз в 6 месяцев в течение 3 лет с момента последнего обострения (Приказ МЗ РФ от 21 де- кабря 2012 г. № 1344 н «Об утверждении порядка проведения диспансерного наблюдения»)) (УУР С, УДД — 5).
• Пациентам с пищеводом Баррета рекомендует- ся диспансерное наблюдение для предупреждения АКП и ранней диагностики дисплазии эпителия, сроки которого определяются наличием и степенью дисплазии.
Пациентам с верифицированным диагнозом пищевода Баррета при выявлении дисплазии низкой степени необходимо назначить ИПП с повторением гистологического исследования через 3 месяца. При сохранении дисплазии низ- кой степени больным рекомендуется продолжить постоянный прием полной дозы ИПП и провести гистологическое исследование через 3 и 6 меся- цев. Затем гистологическое исследование прово- дится ежегодно. Если выявляется дисплазия вы- сокой степени, необходимо назначить двойную дозу ИПП с параллельной оценкой результатов гистологического исследования и последующим решением вопроса об эндоскопическом или хи- рургическом лечении больного. Более подробные алгоритмы ведения больных с пищеводом Барре- та изложены в специальных клинических реко- мендациях [47].
5. Дополнительная информация (в том числе факторы, влияющие на исход заболевания или состояния)
5.1. Особенности лечения ГЭРБ при беременности
Лечение ГЭРБ у беременных представляет непростую задачу и требует индивидуального под- бора терапии с учетом потенциального вреда лекарственных средств. Универсальными можно считать рекомендации по изменению образа жизни, а так- же приему алгинатов при необходимости и после консультации с врачом. Благодаря доказанной высокой эффективности и безопасности во всех триместрах беременности, эти препараты являются препаратами выбора для лечения изжоги беремен- ных [225–227] (УУР А, УДД — 1). Поскольку алгинаты почти не имеют побочных эффектов, их можно рекомендовать не только беременным, но и кормящим женщинам.
.
Список литературы:
2. Ivashkin V.T., Trukhmanov A.S., Sheptulin A.A. Gastroezofageal'naya reflyuksnaya bolezn'. Rekomendatsii po diagnostike i lecheniyu. M., 2013.
3. Trukhmanov A.S., Dzhakhaya N.L., Kaibysheva V.O., Storonova O.A. Novye aspekty rekomendatsii po lecheniyu bol'nykh gastroezofageal'noi reflyuksnoi bolezn'yu. Gastroenterologiya i Gepatologiya: novosti, mneniya, obuchenie. 2013;1:2-9.
4. Ivashkin V.T., Trukhmanov A.S. Sovremennyi podkhod k terapii gastroezofageal'noi reflyuksnoi bolezni vo vrachebnoi praktike. Russkii meditsinskii zhurnal. Bolezni organov pishchevareniya. 2003;5(2):43.
5. Maev I.V., V'yuchnova E.S., Lebedeva E.G., Dicheva D.T., Antonenko O.M., Shcherbenkov I.M. Gastroezofageal'naya reflyuksnaya bolezn' (uchebno-metodicheskoe posobie). M.: VUNTsMZ RF, 2000.
6. Modlin I.M., Hunt R.H., Malfertheiner P., Moayyedi P., M Quigley E., N J Tytgat G., et al. Nonerosive reflux disease - defining the entity and delineating the management. Digestion. 2008;78(1):1-5. https://doi.org/10.1159/000151248
7. Maev I.V., Andreev D.N., Dicheva D.T. Gastroezofageal'naya reflyuksnaya bolezn': ot patogeneza k terapevticheskim aspektam. Consilium medicum. 2013;15(8.):30-4.
8. Zairat'yants O.V., Maev I.V., Smol'yannikova V.A., Movtaeva P.R. Patologicheskaya anatomiya pishchevoda Barreta. Arkhiv patologii. 2011;73(3):21-6.
9. Zairat'yants O.V. Zairat'yants G.O., Movtaeva P.R. Problemy sovremennoi gastroenterologii: pishchevod Barreta. Klinicheskaya i eksperimental'naya morfologiya. 2012;2:9-16.
10. Chandrasoma P.T., DeMeester T.R. GERD. Reflux to Esophageal Adenocarcinoma. Burlington: Academic Press; 2006.
11. Ivashkin V.T., Maev I.V., Trukhmanov A.S. Pishchevod Barreta. M.: Shiko; 2011.
12. Richter J.E., Friedenberg F.K. Gastroesophageal Reflux Disease. In.: Sleisenger and Fordtran's Gastrointestinal and Liver Disease: Pathophysiology, Diagnosis, Management. edited by Mark Feldman, Lawrence S Friedman, Laurence J Brandt. 10th ed., 2015.
13. Maev I.V., Yurenev G.L., V'yuchnova E.S., Andreev D.N., Dicheva D.T., Partsvania-Vinogradova E.V. Gastroezofageal'naya reflyuksnaya bolezn'. M.: GEOTAR-Media; 2019.
14. Chatila A.T., Nguyen M.T.T., Krill T., Roark R., Bilal M., Reep G. Natural history, pathophysiology and evaluation of gastroesophageal reflux disease. Dis Mon. 2020;66(1):100848. https://doi.org/10.1016/j.dis-amonth.2019.02.001
15. El-Serag H.B., Sweet S., Winchester C.C., Dent J. Update on the epidemiology of gastro-oesophageal reflux disease: a systematic review. Gut. 2014;63(6):871-80. https://doi.org/10.1136/gutjnl-2012-304269
16. Savarino E., Marabotto E., Bodini G., Pellegatta G., Coppo C., Giambruno E., et al. Epidemiology and natural history of gastroesophageal reflux disease. Minerva Gastroenterol Dietol. 2017;63(3):175-83. https://doi.org/10.23736/S1121-421X.17.02383-2
17. Eusebi L.H., Ratnakumaran R., Yuan Y., Solaymani-Dodaran M., Bazzoli F., Ford A.C. Global prevalence of, and risk factors for, gastro-oesophageal reflux symptoms: a meta-analysis. Gut. 2018;67(3):430-40. https://doi.org/10.1136/gutjnl-2016-313589
18. Lazebnik LB, Masharova AA, Bordin DS, Vasil'ev YuV, Tkachenko EI, Abdulkhakov RA, i dr. Rezul'taty Mnogotsentrovogo issledovaniya «Epidemiologiya Gastroezofageal'noi REflyuksnoi bolezni v Rossii» (MEGRE). Terapevticheskii arkhiv. 2011;83(1):45-50.
19. Bor S., Lazebnik L.B., Kitapcioglu G., Manannikof I., Vasiliev Y. Prevalence of gastroesophageal reflux disease in Moscow. Dis Esophagus. 2016;29(2):159-65. https://doi.org/10.1111/dote.12310
20. Gallinger Yu.I., Godzhello E.A. Operativnaya endoskopiya pishchevoda. M., 1999. 273 c.
21. Dronova O.B., Kagan I.I., Tret'yakov A.A., Mishchenko A.N. Diagnostika gastroezofageal'noi reflyuksnoi bolezni. Orenburg; 2008. 90 c.
22. Ivashkin V.T., Trukhmanov A.S. Evolyutsiya predstavlenii o roli narushenii dvigatel'noi funktsii pishchevoda v patogeneze gastroezofageal'noi reflyuksnoi bolezni. Ros zhurn gastroenterol gepatol koloproktol. 2010;20(2):13-9.
23. Shul'pekova Yu.O., Ivashkin V.T. Gastroezofageal'naya reflyuksnaya bolezn': klinicheskie i farmakologicheskie aspekty. RMZh. 2002;10(4):200-5.
24. Stanghellini V. Three-month prevalence rates of gastrointestinal symptoms and the influence of demographic factors: Results from the Domestic International Gastroenterology Surveillance Study (DIGEST). Scand J Gastroenterol. 1999;231:20-8.
25. Trukhmanov A.S., Ivashkina N.Yu. Klinicheskoe znachenie narushenii dvigatel'noi funktsii pishchevoda, zheludka i dvenadtsatiperstnoi kishki. Terapevticheskii arkhiv. 2019;91(8):127-34. https://doi.org/10.26442/00403660.2019.08.000390
26. Dronova O.B., Mironchev O.A. Anatomo-endoskopicheskie osobennosti pishchevodno-zheludochnogo perekhoda i ikh klinicheskoe znachenie. Voprosy rekonstruktivnoi i plasticheskoi khirurgii. 2007;3-4:40-2.
27. Trukhmanov A.S., Storonova O.A., Ivashkin V.T. Klinicheskoe znachenie issledovaniya dvigatel'noi funktsii pishchevaritel'noi sistemy: proshloe, nastoyashchee, budushchee. Ros zhurn gastroenterol gepatol koloproktol. 2013;23(5):4-14.
28. Trukhmanov A.S. Vliyanie antagonistov dopaminovykh retseptorov na dvigatel'nuyu funktsiyu zheludochnokishechnogo trakta. Lechashchii vrach. 2012;9:80-3.
29. Storonova O.A., Trukhmanov A.S., Dzhakhaya N.L., Ivashkin V.T. Narusheniya pishchevodnogo klirensa pri gastroezofageal'noi reflyuksnoi bolezni i vozmozhnosti ikh korrektsii. Ros zhurn gastroenterol gepatol koloproktol. 2012;21(2):14-21.
30. Storonova O.A., Trukhmanov A.S., Ivashkin V.T. Rol' zashchitnykh faktorov slizistoi obolochki pishchevoda v lechenii gastroezofageal'noi reflyuksnoi bolezni. Klinicheskie perspektivy gastroenterologii, gepatologii. 2014;(5):37-42.
31. Namiot Z., Sarosiek J., Marcinkiewicz M. Edmunds M.C., McCallum R.W. Declined human esophageal mucin secretion in patients with severe reflux esophagitis. Dig. Dis. Sci. 1994;39:2523-9. https://doi.org/10.1007/BF02087685
32. Niv Y., Fass R. The role of mucin in GERD and its complications. Gastroenterol. Hepatol. 2011;9(1):55-9. https://doi.org/10.1038/nrgastro.2011.211
33. Van Roon A.H., Mayne G.C., Wijnhoven B.P.L., Watson D.I., Leong M.P., Neijmanet G.E. et al. Impact of gastro-esophageal reflux on mucin mRNA expression in the esophageal mucosa. J. Gastrointest. Surg. 2008;12:1331-40. https://doi.org/10.1007/s11605-008-0522-y
34. Dent J. Pathogenesis of gastro-oesophageal reflux disease and novel options for its therapy. Neurogastroenterol Motil. 2008;20(1):91-102. https://doi.org/10.1111/j.1365-2982.2008.01096.x
35. Tsoukali E., Sifrim D. Investigation of extraesophageal gastroesophageal reflux disease Ann Gastroenterol. 2013;26:1-6.
36. Wu J.C., Mui L.M., Cheung C.M., Chan Y., Sung J.J. Obesity is associated with increased transient lower esophageal sphincter relaxation. Digestion. 2007;132(3):883-9. https://doi.org/10.1053/j.gastro.2006.12.032
37. Ivashkin V.T., Sheptulin A.A., Trukhmanov A.S. Klinicheskie aspekty funktsional'noi dispepsii i effektivnost' ganatona (itoprida gidrokhlorida) v ee lechenii. Ros zhurn gastroenterol gepatol koloproktol. 2009;19(6):17-22.
38. Pauwels A., Altan E., Tack J. The gastric accommodation response to meal determines the occurrence of transient lower esophageal sphincter relaxations and reflux events in patients with gastro-esophageal reflux disease. Neurogastroenterol Motil. 2014;26:581-8. https://doi.org/10.1111/nmo.12305
39. Evsyutina Yu.V., Ivashkin V.T. Rol' mikrobioma v razvitii boleznei pishchevoda. Ros zhurn gastroenterol gepatol koloproktol. 2016;26(3):11-6. https://doi.org/10.22416/13824376-2016-26-3-11-16
40. Rumyantseva D.E., Trukhmanov A.S., Kudryavtseva A.V., Krasnov G.S., Paraskevova A.V., Storonova O.A. i dr. Mikrobiota pishchevoda i zheludka u bol'nykh gastroezofageal'noi reflyuksnoi bolezn'yu i zdorovykh dobrovol'tsev. Ros zhurn gastroenterol gepatol koloproktol. 2018;28(4):36-46. https://doi.org/10.22416/1382-4376-2018-28-4-36-46
41. Rumyantseva D.E., Trukhmanov A.S., Kudryavtseva A.V., Ivashkin V.T. Vliyanie kislotosupressii na mikrobiotu zheludochno-kishechnogo trakta. Ros zhurn gastroenterol gepatol koloproktol. 2018;28(1):78-88. https://doi.org/10.22416/1382-43762018-28-1-78-88.
42. Vakil N., van Zanten S.V., Kahrilas P., Dent J., Jones R., Global Consensus Group. The Montreal Definition and Classification of GERD. Am J Gastroenterol. 2006;101:1900-20. https://doi.org/10.1111/j.1572-0241.2006.00630.x
43. Tytgat G.N., McColl K., Tack J, Holtmann G., Hunt R.H., Malfertheiner P., et al. New algorithm for the treatment of gastro-oesophageal reflux disease. Aliment Pharmacol Ther. 2008;27:249-56. https://doi.org/10.1111/j.1365-2036.2007.03565.x
44. Katz P.O., Gerson L.B., Vela M.F. Guidelines for the diagnosis and management of gastroesophageal reflux disease. Am J Gastroenterol. 2013;108:308-12. https://doi.org/10.1038/ajg.2012.444
45. Roshchina T.V. Gastroezofageal'naya reflyuksnaya bolezn' u bol'nykh bronkhial'noi astmoi: dis. ... kand. med. nauk. M.; 2002.
46. Hayat J.O., Gabieta-Somnez S., Yazaki E., Kang J-Y., Woodcock A., Dettmar P., et al. Pepsin in saliva for the diagnosis of gastro oesophageal reflux disease. Gut. 2015;64:373-80. https://doi.org/10.1136/gutjnl-2014-307049
47. Ivashkin V.T., Maev I.V., Kaprin A.D., Agapov M.Yu., Andreev D.N., Vodoleev A.S. i dr. Rannee vyyavlenie onkologicheskikh zabolevanii organov pishchevareniya (metodicheskoe rukovodstvo Rossiiskoi gastroenterologicheskoi assotsiatsii i Assotsiatsii onkologov Rossii dlya vrachei pervichnogo zvena zdravookhraneniya). Ros zhurn gastroenterol gepatol koloproktol. 2019;29(5):53-74. https://doi.org/10.22416/13824376-2019-29-5-53-74
48. Shaheen N.J., Weinberg D.S., Deaberg T.D., Chou R., Qaseem A., Shekelle P., et al. Upper endoscopy for gastroesophageal reflux disease: Best practice advice from the clinical guidelines of the American College of Physicians. Ann Intern Med. 2012;157:803-16. https://doi.org/10.7326/00034819-157-11-201212040-00008
49. Abe Y., Sasaki Y., Yagi M., Yaoita T., Nishise S., Ueno Y. Diagnosis and treatment of eosinophilic esophagitis in clinical practice. Clin J Gastroenterol. 2017;10(2):87-102. https://doi.org/10.1007/s12328-017-0725-4
50. Lucendo A.J., Molina-Infante J., Arias A., von Arnim U., Bredenoord A.J., Bussmann C., et al. Guidelines on eosinophilic esophagitis: evidence-based statements and recommendations for diagnosis and management in children and adults. United European Gastroenterol J. 2017;5(3):335-58. https://doi.org/10.1177/2050640616689525
51. Dellon E.S., Gonsalves N., Hirano I., Furuta G.T., Liacouras C.A., Katzka D.A., et al. ACG clinical guideline: evidenced based approach to the diagnosis and management of esophageal eosinophilia and eosinophilic esophagitis. Am J Gastroenterol. 2013;108:679-92. https://doi.org/10.1038/ajg.2013.71
52. Dellon E.S., Speck O., Woodward K., Covey S., Rusin S., Shaheen N.J., et al. Distribution and variability of esophageal eosinophilia in patients undergoing upper endoscopy. Mod Pathol. 2015;28:383-90. https://doi.org/10.1038/modpathol.2014.110
53. Ivashkin V.T., Maev I.V., Trukhmanov A.S., Andreev D.N., Lapina T.L., Baranskaya E.K. i dr. Klinicheskie rekomendatsii rossiiskoi gastroenterologicheskoi assotsiatsii po diagnostike i lecheniyu eozinofil'nogo ezofagita. Ros zhurn gastroenterol gepatol koloprok-tol. 2018;28(6):84-98. https://doi.org/10.22416/1382-4376-2018-28-6-84-98
54. Zairat'yants O.V., Kononov A.V. Pishchevod Barreta. Klinicheskie rekomendatsii Rossiiskogo obshchestva patologoanatomov. M.: GEOTAR-Media; 2016. http://www.patolog.ru
55. Fitzgerald R.C., di Pietro M., Ragunath K., Ang Y., Kang J., Watson P., et al. British Society of Gastroenterology guidelines on the diagnosis and management of Barrett's oesophagus. Gut. 2014;63(1):7-42. https://doi.org/10.1136/gutjnl-2013-305372
56. Saleh C.M.G., Smout J.P.M., Bredenoord A.J. The diagnosis of gastro-esophageal reflux disease cannot be made with barium esophagograms. Neurogastroenterol Motil. 2015;27:195-200.
57. Trudgill N.J, Sifrim D., Sweis R., Fullard M., Basu K., McCord M., et al. British Society of Gastroenterology guidelines for oesophageal manometry and oesophageal reflux monitoring. Gut. 2019;66:1-20. https://doi.org/10.1136/gutjnl-2018-318115
58. O'Boyle C.J., Watson D.I., DeBeaux A.C., Jamieson G.G. Preoperative prediction of long-term outcome following laparoscopic fundoplication. ANZ J Surg. 2002;72:471-5. https://doi.org/10.1046/j.1445-2197.2002.02455.x
59. Galmiche J.P., Hatlebakk J., Attwood S., Ell C., Fioc-ca R., Eklund S., et al. Laparoscopic antireflux surgery vs esomeprazole treatment for chronic GERD. JAMA. 2011;305:1969-77. https://doi.org/10.1001/jama.2011.626.
60. Gyawali C.P., Kahrilas P.J., Savarino E., Zerbib F., Mion F., Smout A.J.P.M., et al. Modern diagnosis of GERD: the Lyon Consensus. Gut. 2018;67:1351-62. https://doi.org/10.1136/gutjnl-2017-314722
61. Roman S., Gyawali C.P., Savarino E., Yadlapati R., Zerbib F., Wu J., et al. Ambulatory reflux monitoring for diagnosis of gastro-esophageal reflux disease: Update of the Porto consensus and recommendations from an international consensus group. Neurogastroenterol Motil. 2017;29:e13067. https://doi.org/10.1111/nmo.13067
62. Trukhmanov A.S., Storonova O.A., Ivashkin V.T. Klinicheskoe znachenie 24-chasovoi rN-metrii v diagnostike i otsenke effektivnosti lekarstvennykh preparatov u bol'nykh s zabolevaniyami pishchevoda i zheludka. Ros zhurn gastroenterol gepatol koloproktol. 2016;6:55-68.
63. Dzhakhaya N.L., Trukhmanov A.S., Kon'kov M.Yu., Sklyanskaya O.A., Sheptulin A.A., Ivashkin V.T. Vozmozhnosti 24-chasovogo monitorirovaniya rN v pishchevode v diagnostike i kontrole effektivnosti lecheniya GERB. Ros zhurn gastroenterol gepatol koloproktol. 2012;1:23-30.
64. Storonova O.A., Trukhmanov A.S. Prakticheskomu vrachu o prodolzhitel'noi intragastral'noi rN-metrii: posobie dlya vrachei. 2-e izd. M.; 2015.
65. Hirano I., Richter J.E., Practice Parameters Committee of the American College of Gastroenterology. ACG practice guidelines: Esophageal reflux testing. Am J Gastroenterol. 2007;102:668-85. https://doi.org/10.1111/j.1572-0241.2006.00936.x
66. Villa N., Vela M.F. Impedance-pH testing. Gastroenterol Clin N Am. 2013;42:17-26. https://doi.org/10.1016/j.gtc.2012.11.003
67. Sifrim D., Fornari F. Esophageal impedance-pH monitoring. Dig Liver Dis. 2008;40:161-6. https://doi.org/10.1016/j.dld.2007.10.023
68. Kaibysheva V.O., Storonova O.A., Trukhmanov A.S., Ivashkin V.T. Vnutripishchevodnaya rN-impedansometriya v diagnostike GERB. Ros zhurn gastroenterol gepatol koloproktol. 2013;(2):4-12.
69. Charbel S., Khandwala F., Vaezi M.F. The role of esophageal pH monitoring in symptomatic patients on PPI therapy. Am J Gastroenterol. 2005;100:283-9. https://doi.org/10.1111/j.1572-0241.2005.41210.x
70. Jaspersen D., Kulig M., Labenz J., Leodolter A., Lind T., Meyer-Sabellek W., et al. Prevalence of extra-oesophageal manifestations in gastro-oesophageal reflux disease: an analysis based on the ProGERD Study. Aliment Pharmacol Ther. 2003;17:1515-20. https://doi.org/10.1046/j.1365-2036.2003.01606.x
71. Lechien J.R., Akst L.M., Hamdan A.L., Schindler A., Karkos P.D., Barillari M.R., et al. Evaluation and Management of Laryngopharyngeal Reflux Disease: State of the Art Review. Otolaryngol Head Neck Surg. 2019;160(5):762-82. https://doi.org/10.1177/0194599819827488
72. Lee J.S., Jung A.R., Park J.M., Park M.J., Lee Y.C., Eun Y.G. Comparison of characteristics according to reflux type in patients with laryngopharyngeal reflux. Clin Exp Otorhinolaryngol. 2018;11:141-5. https://doi.org/10.21053/ceo.2017.00577
73. Wang A.J., Liang M.J., Jiang A.Y., Lin J.K., Xiao Y.L., Peng S., et al. Gastroesophageal and laryngopharyngeal reflux detected by 24-hour combined impedance and pH monitoring in healthy Chinese volunteers. J Dig Dis. 2011;12:173-80. https://doi.org/10.1111/j.1751-2980.2011.00502.x
74. Patterson N., Mainie I., Rafferty G., McGarvey L., Heaney L., Tutuian R., et al. Nonacid reflux episodes reaching the pharynx are important factors associated with cough. J Clin Gastroenterol. 2009;43:414-9. https://doi.org/10.1097/MCG.0b013e31818859a3
75. Sheptulin A.A., Storonova O.A. Chrezmernayaotryzhka - samostoyatel'nyi sindrom ili dopolnitel'nyi simptom funktsional'noi dispepsii? Ros zhurn gastroenterol gepatol koloproktol. 2020;30(3):55-60. https://doi.org/10.22416/1382-4376-2020-30-3-55-60
76. Koukias N., Woodland P., Yazaki E., Sifrim D. Supragastric Belching: Prevalence and Association With Gastroesophageal Reflux Disease and Esophageal Hypomotility. J Neurogastroenterol Motil. 2015;21(3):398-403. https://doi.org/10.5056/jnm15002
77. Aziz Q., Fass R., Gyawali C.P., Miwa H., Pandolfino J.E., Zerbib F. Esophageal Disorders. Gastroenterology. 2016;150:1368-79. https://doi.org/10.1053/j.gastro.2016.02.012
78. Patel A., Sayuk G.S., Kushnir V.M., Chan W.W., Gyawali C.P. GERD phenotypes from pH-impedance monitoring predict symptomatic outcome on prospective evaluation. Neurogastroenterol Motil. 2016;28(4):513-21. https://doi.org/10.1111/nmo.12745
79. Andreev D.N., Zaborovskii A.V., Trukhmanov A.S., Maev I.V., Ivashkin V.T. Evolyutsiya predstavlenii o funktsional'nykh zabolevaniyakh zheludochno-kishechnogo trakta v svete Rimskikh kriteriev IV peresmotra (2016 g.). Ros zhurn gastroenterol gepatol koloproktol. 2017;27(1):4-11. https://doi.org/10.22416/1382-43762017-27-1-4-11
80. Francis D.O., Goutte M., Slaughter J.C., Garrett C.G., Hagaman D., Holzman M.D., et al. Traditional reflux parameters and not impedance monitoring predict outcome after fundoplication in extraesophageal reflux. Laryngoscope. 2011;121(9):1902-9. https://doi.org/10.1002/lary.21897
81. Pauwels A., Boecxstaens V., Andrews C.N., Attwood S.E., Berrisford R., Bisschops R., et al. How to select patients for antireflux surgery? The ICARUS guidelines (international consensus regarding preoperative examinations and clinical characteristics assessment to select adult patients for antireflux surgery). Gut. 2019;68(11):1928-41. https://doi.org/10.1136/gutjnl-2019-318260
82. Galvani C., Fisichella P.M., Gorodner M.V., Perretta S., Patti M.G. Symptoms are a poor indicator of reflux status after fundoplication for gastroesophageal reflux disease. Arch Surg. 2003;138:514-9. https://doi.org/10.1001/arch-surg.138.5.514
83. Broeders J.A., Bredenoord A.J., Hazebroek E.J., Broeders I.A.M.J., Gooszen H.G., Smout A.J.P.M. Effects of anti-reflux surgery on weakly acidic reflux and belching. Gut. 2011;60:435-41. https://doi.org/10.1136/gut.2010.224824
84. Storonova O.A., Trukhmanov A.S. 24-chasovaya rN-impedansometriya. Differentsial'nyi diagnoz funktsional'nykh zabolevanii pishchevoda. Posobie dlya vrachei. M.: Medpraktika; 2018.
85. Hemmink G.J., Bredenoord A.J., Weusten B.L., Monkelbaan J.F., Timmer R., Smout A.J. Esophageal pH-impedance monitoring in patients with therapy-resistant reflux symptoms: 'on' or 'off' proton pump inhibitor? Am J Gastroenterol. 2008;103:2446-53. https://doi.org/10.1111/j.1572-0241.2008.02033.x
86. Storonova O.A., Trukhmanov A.S., Makushina A.A., Paraskevova A.V., Ivashkin V.T. Novye parametry rN-impedansometrii v postanovke diagnoza gastroezofageal'noi reflyuksnoi bolezni i prognoze tyazhesti techeniya zabolevaniya. Ros zhurn gastroenterol gepatol koloproktol. 2019;29(2):35-44. https://doi.org/10.22416/1382-4376-2019-29-2-35-44
87. Frazzoni L., Frazzoni M., de Bortoli N., Tolone S., Furnari M., Martinucci I., et al. Postreflux swallow-induced peristaltic wave index and nocturnal baseline impedance can link PPI-responsive heartburn to reflux better than acid exposure time. Neurogastroenterol Motil. 2017; 29(11): 10.1111/nmo.13116. https://doi.org/10.1111/nmo.13116.
88. Frazzoni M., Manta R., Mirante V.G., Mirante V.G., Conigliaro R., Frazzoni L., Melotti G. Esophageal chemical clearance is impaired in gastroesophageal reflux disease - A 24 h impedance-pH monitoring assessment. Neurogastroenterol Motil. 2013;25(5):399-406, e295. https://doi.org/10.1111/nmo.12080
89. Pandolfino J.E., Kahrilas P.J., American Gastroenterological Association. American Gastroenterological Association medical position statement: Clinical use of esophageal manometry. Gastroenterology. 2005;128(1):207-8 https://doi.org/10.1053/j.gastro.2004.11.007
90. Ivashkin V.T., Maev I.V., Trukhmanov A.S., Storonova O.A., Abdulkhakov S.R., Andreev D.N. i dr. Rekomendatsii Rossiiskoi gastroenterologicheskoi assotsiatsii po klinicheskomu primeneniyu manometrii vysokogo razresheniya pri zabolevaniyakh pishchevoda. Ros zhurn ga-stroenterol gepatol koloproktol. 2020;30(3):61-88. https://doi.org/10.22416/1382-4376-2020-30-3-61-88
91. Bredenoord A.J., Weusten B.L.A.M., Sifrim D., Timmer R., Smout A.J.P.M. Aerophagia, gastric, and supragastric belching: a study using intraluminal electrical impedance monitoring. Gut. 2004;53(11):1561-5. https://doi.org/10.1136/gut.2004.042945
92. Gyawali C.P., Roman S., Bredenoord A.J., Fox M., Keller J., Pandolfino J.E., et al. Classification of esophageal motor findings in gastro-esophageal reflux disease: Conclusions from an international consensus group. Neurogastroenterol Motil. 2017;29(12): 10.1111/nmo.13104. https://doi.org/10.1111/nmo.13104.
93. Kahrilas P.J., Bredenoord A.J., Fox M., Gyawali C.P., Roman S., Smout A.J.P.M., et al. The Chicago Classification of Esophageal Motility Disorders, v3.0. Neuro-gastroenterol Motil. 2015;27(2):160-74. https://doi.org/10.1111/nmo.12477
94. Ivashkin V.T., Maev I.V., Trukhmanov A.S., Storonova O.A., Kucheryavyi Yu.A., Barkalova E.V. i dr. Manometriya vysokogo razresheniya i novaya klassifikatsiya narushenii motoriki pishchevoda. Terapevticheskii Arkhiv. 2018;90(5):93-100.
95. Maev I.V., Barkalova E.V., Ovsepyan M.A., Andreev D.N., Kucheryavyi Yu.A. Pokazateli rN-impedansometrii i manometrii pishchevoda vysokogo razresheniya u patsientov s razlichnymi formami gastroezofageal'noi reflyuksnoi bolezni. Ros zhurn gastroenterol gepatol koloproktol. 2018;28(4):23-35. https://doi.org/10.22416/1382-4376-2018-28-4-23-35
96. Storonova O.A., Trukhmanov A.S., Ivashkin V.T. Manometriya vysokogo razresheniya v klinicheskoi praktike: analiz dvigatel'noi funktsii pishchevoda v sootvetstvii s Chikagskoi klassifikatsiei. Ros zhurn gastroenterol gepatol koloproktol. 2018;28(2):11-23. https://doi.org/10.22416/1382-43762018-28-2-11-23
97. Pandolfino J.E., Kim H., Ghosh S.K., Clarke J.O., Zhang Q., Kahrilas P.J. High-resolution manometry of the EGJ: an analysis of crural diaphragm function in GERD. Am J Gastroenterol. 2007;102:1056-63. https://doi.org/10.1111/j.1572-0241.2007.01138.x
98. Gyawali C.P., Sifrim D., Carlson D.A., Hawn M., Katzka D.A., Pandolfino J.E., et al. Ineffective esophageal motility: Concepts, future directions, and conclusions from the Stanford 2018 symposium. Neurogastroenterol Motil. 2019;31(9):e13584. https://doi.org/10.1111/nmo13584
99. Reddy CA, Patel A, Gyawali CP. Impact of symptom burden and health-related quality of life (HRQOL) on esophageal motor diagnoses. Neurogastroenterol Motil. 2017;29(4):10.1111/nmo.12970. https://doi.org/10.1111/nmo.12970
100. Min Y.W., Shin I., Son H.J., Rhee P. Multiple Rapid Swallow Maneuver Enhances the Clinical Utility of High-Resolution Manometry in Patients Showing Ineffective Esophageal Motility. Medicine (Baltimore). 2015;94(40):e1669. https://doi.org/10.1097/MD.0000000000001669
101. Stoikes N., Drapekin J., Kushnir V., Shaker A., Brunt L.M., Gyawali C.P. The value of multiple rapid swallows during preoperative esophageal manometry before laparoscopic antireflux surgery. Surg Endosc. 2012;26(12):3401-7. https://doi.org/10.1007/s00464-012-2350-0
102. Smout A., Fox M. Weak and absent peristalsis. Neurogas-troenterol Motil. 2012;24(1):40-7. https://doi.org/10.1111/j.1365-2982.2011.01831.x
103. Weijenborg P.W., Savarino E., Kessing B.F., Roman S., Costantini M., Oors J.M., et al. Normal values of esophageal motility after antireflux surgery; a study using high-resolution manometry. Neurogastroenterol Motil. 2015;27(7):929-35. https://doi.org/10.1111/nmo.12554
104. Mones J., Clave P., Mearin F. Esophageal pH monitoring: are you sure that the electrode is properly placed? Am J Gastroenterol. 2001;96:975-8. https://doi.org/10.1111/j.1572-0241.2001.03680.x
105. Smeets F.G., Keszthelyi D., Bouvy N.D., Masclee A.A.M., Conchillo J.M. Does measurement of esophagogastric junction distensibility by EndoFLIP predict therapy-responsiveness to endoluminal fundoplication in patients with gastroesophageal reflux disease? J Neurogastroenterol Motil. 2015;21:255-64. https://doi.org/10.5056/jnm14111
106. Kwiatek M.A., Pandolfino J.E., Hirano I., Kahri-las P.J. Esophagogastric junction distensibility assessed with an endoscopic functional luminal imaging probe (EndoFLIP). Gastrointest Endosc. 2010;72:272-8. https://doi.org/10.1016/j.gie.2010.01.069
107. Hirano I., Pandolfino J.E., Boeckxstaens G.E. Functional Lumen Imaging Probe for the Management of Esophageal Disorders: Expert Review From the Clinical Practice Updates Committee of the AGA Institute. Clin Gastroenterol Hepatol. 2017;15(3):325-34. https://doi.org/10.1016/j.cgh.2016.10.022
108. Hoffman A., Basting N., Goetz M., Tresch A., Mudter J., Biesterfeld S., et al. High-definition endoscopy with i-Scan and lugol's solution for more precise detection of mucosal breaks in patients with reflux symptoms. Endoscopy. 2009;41:103-12. https://doi.org/10.1055/s-0028-1119469
109. Sharma P., Wani S., Bansal A., Hall S., Puli S., Mathur S., et al. A feasibility trial of narrow band imaging endoscopy in patientes with gastroesophageal reflux disease. Gastroenterology. 2007;133:454-64. https://doi.org/10.1053/j.gastro.2007.06.006
110. Swager A., Curvers W.L., Bergman J.J. Diagnosis by endoscopy and advanced imaging. Best Pract Res Clin Gastroenterol. 2015;29:97-111. https://doi.org/10.1016/j.bpg.2014.11.011
111. Thekkek N., Anandasabapathy S., Richards-Kortum R. Optical Molecular Imaging for Detection of Barrett's-associated Neoplasia. World J Gastroenterol. 2011;17(1):53-62. https://doi.org/10.3748/wjg.v17.i1.53
112. Singh R., Yeap S.P. Endoscopic Imaging in Barrett's Esophagus. Expert Rev Gastroenterol Hepatol. 2015;9(4):475-85. https://doi.org/10.1586/17474124.2015.983080
113. Pirogov S., Sokolov V., Kaprin A., Volchenko N.N., Karpova E.S., Pavlov P.V., et al. Endocytoscopy-novel endoscopic diagnostics approach: principles and procedure. Eksp Klin Gastroenterol. 2015;(4):12-21.
114. Kahrilas P.J., Shaheen N.J., Vaezi M.F., Hiltz S.W., Black E., Modlin I.M., et al. American Gastroenterological Association Medical Position Statement on the Management of Gastroesophageal Reflux Disease. Gastroenterology. 2008;135:1383-91. https://doi.org/10.1053/j.gastro.2008.08.045
115. Gunaratnam N.T., Jessup T.P., Inadomi J. Sub-optimal proton pump inhibitor dosing is prevalent in patients with poorly controlled gastrooesophageal reflux disease Aliment Pharmacol Ther. 2006;23:1473-7. https://doi.org/10.1111/j.1365-2036.2006.02911.x
116. Schindlbeck N.E., Klauser A.G., Berghammer G., Lon-dong W., Muller-Lissner S.A. Three year follow up of patients with gastrooesophageal reflux disease. Gut. 1992;33:1016-9. https://doi.org/10.1136/gut.33.8.1016
117. Jacobson B.C., Somers S.C., Fuchs C.S., Kelly C.P., Camargo C.A. Jr. Body-mass index and symptoms of gastro esophageal reflux in women. N Engl J Med. 2006;354:2340-8. https://doi.org/10.1056/NEJMoa054391
118. Kaltenbach T., Crockett S., Gerson L.B. Are lifestyle measures effective in patients with gastroesophageal reflux disease? An evidence-based approach. Arch Intern Med. 2006;166:965-71. https://doi.org/10.1001/archinte.166.9.965
119. Ness-Jensen E., Hveem K., El-Serag H., Lagergren J. Lifestyle intervention in gastroesophageal reflux disease. Clin Gastroenterol Hepatol. 2016;14(2):175-82. https://doi.org/10.1016/j.cgh.2015.04.176
120. Piesman M., Hwang I., Maydonovitch C., Wong R.K.H. Nocturnal reflux episodes following the administration of a standardized meal. Does timing matter? Am J Gastroenterol. 2007;102:2128-34. https://doi.org/10.1111/j.1572-0241.2007.01348.x
121. Stanciu C., Bennett J.R. Effects of posture on gastro-oesophageal reflux. Digestion. 1977;15:104-9. https://doi.org/10.1159/000197991
122. Hamilton J.W., Boisen R.J., Yamamoto D.T., Wagner J.L., Reichelderfer M. Sleeping on a wedge diminishes exposure of the esophagus to refluxed acid. Dig Dis Sci. 1988;33:518-22. https://doi.org/10.1007/BF01798350
123. Osadchuk A.M., Davydkin I.L., Gritsenko T.A., Osad-chuk M.A. Gastroezofageal'naya reflyuksnaya bolezn' i ezofagit, assotsiirovannye s primeneniem lekarstvennykh preparatov: sovremennoe sostoyanie problemy. Terapevticheskii arkhiv. 2019;91(8):135-40. https://doi.org/10.26442/00403660.2019.08.000228
124. Sulz M.C., Manz M., Grob P., Meier R., Drewe J., Beglinger C. Comparison of two antacid preparations on intragastric acidity - a two-centre open randomised cross-over placebo-controlled trial. Digestion. 2007;75(2-3):69-73. https://doi.org/10.1159/000102627
125. McCafferty D.F., Woolfson A.D. A Comparative Assessment of a New Antacid Formulation Based on Magaldrate. Journal of Clinical Pharmacy and Therapeutics. 1983;8(4):349-55. https://doi.org/10.1111/j.1365-2710.1983.tb01058.x
126. Trukhmanov A.S., Gromova O.A. Magaldrat - unikal'nyi antatsid novogo pokoleniya. Obosnovanie tselesoobraznosti ispol'zovaniya antatsidov v klinicheskoi praktike: gastroenterolog i farmakolog. Effektivnaya farmakoterapiya. 2018;16:52-4.
127. Vatier J., Celice-Pingaud C., Farinotti R. Interests of the ‘artificial stomach' techniques to study antacid formulations: comparison with in vivo evaluation. Fundam Clin Pharmacol. 1998;12(6):573-83. https://doi.org/10.1111/j.1472-8206.1998.tb00989.x
128. Simoneau G. Absence of rebound effect with calcium carbonate. Eur J Drug Metab Pharmacokinet. 1996;21(4):351-7. https://doi.org/10.1007/BF03189738
129. Giannini E.G., Zentilin P., Dulbecco P., Iiritano E., Bilardi C., Savarino E., et al. A comparison between sodium alginate and magaldrate anhydrous in the treatment of patients with gastroesophageal reflux symptoms. Digestive diseases and sciences. 2006;51(11):1904-9. https://doi.org/10.1007/s10620-006-9284-0
130. Kwiatek M.A., Roman S., Fareeduddin A., Pandolfino J.E., Kahrilas P.J. An alginate-antacid formulation (Gaviscon Double Action Liquid) can eliminate or displace the postprandial ‘acid pocket' in symptomatic GERD patients. Aliment Pharmacol Ther. 2011;34:59-66. https://doi.org/10.1111/j.1365-2036.2011.04678.x
131. Thomas E., Wade A., Crawford G., Jenner B., Levinson N., Wilkinson J. Randomised clinical trial: relief of upper gastrointestinal symptoms by an acid pocket-targeting alginate-antacid (Gaviscon Double Action) - a double-blind, placebo-controlled, pilot study in gastro-oesophageal reflux disease. Aliment Pharmacol Ther. 2014;39:595-602. https://doi.org/10.1111/apt.12640
132. Dettmar P.W., Hampson F.C., Taubel J., Lorch U., Johnstone L.M., Sykes J., et al. The suppression of gastro-oesophageal reflux by alginates. Int J Clin Pract. 2007;61(10):1654-62. https://doi.org/10.1111/j.1742-1241.2007.01524.x
133. Khan M., Santana J., Donnellan C., Preston C., Moayyedi P. Medical treatments in the short term management of reflux oesophagitis. The Cochrane Database of Systematic Reviews. 2007;18(2):CD003244. https://doi.org/10.1002/14651858.CD003244.pub2
134. Tran T., Lowry A.M., El-Serag H.B. Meta-analysis: The efficacy of over-the-counter gastro-oesophageal reflux disease therapies. Aliment Pharmacol Ther. 2007;25:143-53. https://doi.org/10.1111/j.1365-2036.2006.03135.x
135. Palmieri B., Merighi A., Corbascio D., Rottigni V., Fistetto G., Esposito A. Fixed combination of hyaluronic acid and chondroitin-sulphate oral formulation in a randomized double blind, placebo controlled study for the treatment of symptoms in patients with non-erosive gastroesophageal reflux. Eur Rev Med Pharmacol Sci. 2013;17:3272-8.
136. Savarino V., Pace F., Scarpignato C., Esoxx Study Group. Randomised clinical trial: mucosal protection combined with acid suppression in the treatment of non-erosive reflux disease - efficacy of Esoxx, a hyaluronic acid-chondroitin sulphate based bioadhesive formulation. Aliment Pharmacol Ther. 2017;45(5):631-42. https://doi.org/10.1111/apt.13914
137. Maev I.V., Andreev D.N., Kucheryavyi Yu.A., Shaburov R.I. Sovremennye dostizheniya v lechenii gastroezofageal'noi reflyuksnoi bolezni: fokus na ezofagoprotektsiyu. Terapevticheskii arkhiv. 2019;91(8):4-11. https://doi.org/10.26442/00403660.2019.08.000387
138. Di Simone M.P., Baldi F., Vasina V., Scorrano F., Bacci M.L., Ferrieri A., et al. Barrier effect of Esoxx on esophageal mucosal damage: experimental study on ex-vivo swine model. Clin Exp Gastroenterol. 2012;5:103-7. https://doi.org/10.2147/CEG.S31404
139. Carrasco E., Lopez-Campos F., Sastre-Gallego S., Barrionuevo P., Martin M., Vallejo C., et al. How Efficacious is Ziverel® for Symptomatic Relief of Acute Radiation-Induced Esophagitis? Retrospective Study of Patients Receiving Oncologic Treatment. Canc Therapy & Oncol Int J. 2017;7(5):555724. https://doi.org/10.19080/CTOIJ.2017.07.555724
140. Iannitti T., Morales-Medina J.C., Merighi A., Boari-no V., Laurino C., Vadala M., et al. A hyaluronic acid-and chondroitin sulfate-based medical device improves gastritis pain, discomfort, and endoscopic features. Drug Deliv. and Transl. Res. 2018;8:994-9. https://doi.org/10.1007/s13346-018-0531-7
141. Bariev E.A. Razrabotka sostava i tekhnologii proizvodstva lekarstvennoi formy naloksona gidrokhlorida v vide spreya: dis. ... kand. farm. nauk. M.: 2017.
142. Guelfi G., Stefanetti V., Zampini D., Oommen O.P., Brecchia G., Dall'Aglio C., et al. Gold nanoparticles approach to detect chondroitin sulphate and hyaluronic acid urothelial coating. Scientific reports. 2017;7:10355. https://doi.org/10.1038/s41598-017-09872-0
143. Trapkov V.A. Issledovanie biofizicheskikh mekhanizmov protivoyazvennogo deistviya khondroitina sul'fata: dis. ... kand. biol. nauk. Kupavna; 1984.
144. Palmieri B., Corbascio D., Capone S., Lodi D. Preliminary clinical experience with a new natural compound in the treatment of esophagitis and gastritis: symptomatic effect. Trends Med. 2009;9(4):241-7.
145. Sheptulin A.A., Kurbatova A.A., Baranov S.A. Sovremennye vozmozhnosti primeneniya prokinetikov v lechenii bol'nykh s gastroezofageal'noi reflyuksnoi bolezn'yu. Ros zhurn gastroenterol gepatol koloproktol. 2018;28(1):71-7. https://doi.org/10.22416/1382-4376-2018-28-1-71-77
146. Champion M.C. Prokinetic therapy in gastroesophageal reflux disease. Can J Gastroenterol. 1997;11:55B-65B.
147. Ren L., Chen W.X., Qian L.J., Li S., Gu M., Shi R. Addition of prokinetics to PPI therapy in gastroesophageal reflux disease: A meta-analysis. World J Gastroenterol. 2014;20:2412-9. https://doi.org/10.3748/wjg.v20.i9.2412
148. Kim Y.S., Kim T.H., Choi C.S., Shon Y.W., Kim S.W., Seo G.S., et al. Effect of itopride, a new prokinetic, in patients with mild GERD: a pilot study. World J Gastroenterol. 2005;11(27):4210-4. https://doi.org/10.3748/wjg.v11.i27.4210
149. Ezzat W.F., Fawaz S.A., Fathey H., El Demerdash A. Virtue of adding prokinetics to proton pump inhibitors in the treatment of laryngopharyngeal reflux disease: prospective study. J Otolaryngol Head Neck Surg. 2011;40(4):350-6.
150. Chun B.J., Lee D.S. The effect of itopride combined with lansoprazole in patients with laryngopharyngeal reflux disease. Eur Arch Otorhinolaryngol. 2013;270(4):1385-90. https://doi.org/10.1007/s00405-012-2341-8
151. Fedorchenko Yu.L. Sravnitel'naya kharakteristika prokinetikov pri lechenii gastroezofageal'noi reflyuksnoi bolezni u bol'nykh sakharnym diabetom Eksperimental'naya i klinicheskaya gastroenterologiya. 2013;5:42-8.
152. Maev I.V., Trukhmanov A.S., Sheptulin A.A., Simanenkov V.I., Abdulkhakov S.R., Agafonova N.A. i dr. Rol' narushenii motoriki v patogeneze funktsional'nykh rasstroistv zheludochno-kishechnogo trakta i sovremennye vozmozhnosti ikh lecheniya (Rezolyutsiya Ekspertnogo soveta i obzor literatury). Ros zhurn gastroenterol gepatol koloproktol. 2019;29(6):7-14. https://doi.org/10.22416/1382-4376-2019-29-6-7-14
153. Babu S. Drug Therapy of Gastroesophageal Reflux Disease (GERD): Focus on Itopride Hydrochloride. Indian Practitioner. 2003;56(12):827-30.
154. Minushkin O.N., Loshchinina Yu.N. Effektivnost' primeneniya preparata Ganaton v lechenii bol'nykh GERB. Effektivnaya farmakoterapiya v gastroenterologii. 2008;3:20-4.
155. Takeda N., Takemura M., Kanemitsu Y., Hijikata H., Fukumitsu K., Asano T., et al. Effect of anti-reflux treatment on gastroesophageal reflux-associated chronic cough: Implications of neurogenic and neutrophilic inflammation. Journal of Asthma. 2019;15:1-9. https://doi.org/10.1080/02770903.2019.1641204
156. Kardasheva S.S., Kartavenko I.M., Maksimova N.B., Yur'eva E.Yu., Popova I.R., Pavlov Ch.S. i dr. Effektivnost' trimebutina maleata v lechenii patsientov s funktsional'noi dispepsiei: rezul'taty nablyudatel'nogo issledovaniya «TREND». Ros zhurn gastroenterol gepatol koloproktol. 2018;28(5):67-76. https://doi.org/10.22416/1382-4376-2018-28-5-67-76
157. Aktas A., Caner B., Ozturk F., Bayhan H., Narin Y., Menteset T. The effect of trimebutine maleate on gastric emptying in patients with non-ulcer dyspepsia. Annals of nuclear medicine. 1999;13(4):231-4. https://doi.org/10.1007/BF03164897
158. Kountouras J., Chatzopoulos D., Zavos C., Boura P., Venizelos J., Kalis A. Efficacy of trimebutine therapy in patients with gastroesophageal reflux disease and irritable bowel syndrome. Hepato-gastroenterology. 2002;49(43):193-7.
159. Shaporova N.L., Pidzhimyan V.P., Dudina O.V., Yablonskaya V.N., Sarkisyan S.R. Primenenie trimebutina v kompleksnoi terapii gastroezofageal'noi reflyuksnoi bolezni. Vestnik Rossiiskoi voenno-meditsinskoi akademii. 2016;1:67-71.
160. Gosselin A. Effect of Debridat on gastroesophageal reflux as measured by prolonged pH metry. Gaz Med France. 1982;89:22.
161. Robinson M., Fitzgerald S., Hegedus R., Murthy A., Jokubaitis L., FAST Trial Investigators. Onset of symptom relief with rabeprazole: a community-based, open-label assessment of patients with erosive oesophagitis. Aliment Pharmacol Ther. 2002;16:445-54. https://doi.org/10.1046/j.1365-2036.2002.01181.x
162. Caos A., Moskovitz M., Dayal Y., Perdomo C., Nieces-tro R., Barth J. Rabeprazole for the prevention of pathologic and symtomatic Relapse of erosive or ulcerative Gastroesophageal Reflux disease. The American Journal of Gastroenterology. 2000;95(11):3081-8. https://doi.org/10.1111/j.1572-0241.2000.03179.x
163. Birbara C., Breiter J., Perdomo C., Hahne W. Rabeprazole for the prevention of recurrent erosive or ulcerative gastro-esophageal reflux disease. Eur Journ of Gastroenterology and Hepatology. 2000;12:889-97. https://doi.org/10.1097/00042737-200012080-00008
164. Trukhmanov A.S., Rumyantseva D.E. Taktika vedeniya patsientov s raznymi formami gastroezofageal'noi reflyuksnoi bolezni. Gastroenterologiya. Khirurgiya. Intensivnaya terapiya. Consilium Medicum. 2019;1:7-12. https://doi.org/10.26442/26583739.2019.1.190242
165. Fass R., Inadomi J., Han C., Mody R., O'Neil J., Perez M.C. Maintenance of heartburn relief after step-down from twice-daily proton pump inhibitor to once-daily dex-lansoprazole modified release. Clin Gastroenterol Hepatol. 2012;10(3):247-53. https://doi.org/10.1016/j.cgh.2011.11.021
166. Howden C.W., Larsen L.M., Perez M.C., Palmer R., Atkinson S.N. Clinical trial: efficacy and safety of dexlansoprazole MR 60 and 90 mg in healed erosive oesophagitis - maintenance of healing and symptom relief. Aliment Pharmacol Ther. 2009;30(9):895-907. https://doi.org/10.1111/j.1365-2036.2009.04119.x
167. Metz D.C., Howden C.W., Perez M.C, Larsen L., O'Neil J., Atkinson S.N. Clinical trial: dexlansoprazole MR, a proton pump inhibitor with dual delayed-release technology, effectively controls symptoms and prevents relapse in patients with healed erosive oesophagitis. Aliment Pharmacol Ther. 2009;29(7):742-54. https://doi.org/10.1111/j.1365-2036.2009.03954.x
168. Sharma P., Shaheen N.J., Perez M.C., Pilmer B.L., Lee M., Atkinson S.N., et al. Clinical trials: healing of erosive oesophagitis with dexlansoprazole MR, a proton pump inhibitor with a novel dual delayed-release formulation-results from two randomized controlled studies. Aliment Pharmacol Ther. 2009;29(7):731-41. https://doi.org/10.1111/j.1365-2036.2009.03933.x
169. Fass R., Sontag S.J., Traxler B., Sostek M. Treatment of patients with persistent heartburn symptoms: A double-blind, randomized trial. Clin Gastroenterol Hepatol. 2006;4:50-6. https://doi.org/10.1016/s1542-3565(05)00860-8
170. Vigneri S., Termini R., Leandro G., Badalamenti S., Pantalena M., Savarino V., et al. A comparison of five maintenance therapies for reflux esophagitis. N Engl J Med. 1995;333:1106-10. https://doi.org/10.1056/NEJM199510263331703
171. Hatlebakk J.G., Katz P.O., Kuo B., Kuo B., Castell D.O. Nocturnal gastric acidity and acid breakthrough on different regimens of omeprazole 40mg daily. Aliment Pharmacol Ther. 1998;122:1235-40. https://doi.org/10.1046/j.1365-2036.1998.00426.x
172. Miner P., Orr W., Filippone J., Jokubaitis L., Sloan S. Rabeprazole in Nonerosive Gastroesophageal Reflux Disease: A Randomized Placebo-Controlled Trial. The American Journal Of Gastroenterology. 2002; 97(6):1332-9. https://doi.org/10.1111/j.1572-0241.2002.05769.x
173. Bytzer P., Blum A., De Herdt D., Dubois D., Trial Investigators. Six-month trial of on-demand rabeprazole 10 mg maintains symptom relief in patients with non-erosive reflux disease. Aliment Pharmacol Ther. 2004;20:181-8. https://doi.org/10.1111/j.1365-2036.2004.01999.x
174. Hughes D., Bodger K., Bytzer P., de Herdt D., Dubois D. Economic Analysis of On-Demand Maintenance Therapy with Proton Pump Inhibitors in Patients with Non-Erosive Reflux Disease. Pharmacoeconomics. 2005;23(10):1031-41. https://doi.org/10.2165/00019053200523100-00006
175. Fass R., Chey W.D., Zakko S.F., Andhivarothai N., Palmer R.N., Perez M.C., et al. Clinical trial: the effects of the proton pump inhibitor dexlansoprazole MR on daytime and nighttime heartburn in patients with non-erosive reflux disease. Aliment Pharmacol Ther. 2009;29(12):1261-72. https://doi.org/10.1111/j.1365-2036.2009.04013.x
176. Peura D., Pilmer B., Hunt B., Mody R., Perez M.C. Distinguishing the impact of dexlansoprazole on heartburn vs. regurgitation in patients with gastro-oesophageal reflux disease. Aliment Pharmacol Ther. 2013;38:1303-11. https://doi.org/10.1111/apt.12504
177. Sigterman K.E., van Pinxteren B., Bonis P.A., Lau J., Numans M.E. Short-term treatment with proton pump inhibitors, H2-receptor antagonists and prokinetics for gastro-oesophageal reflux disease-like symptoms and endoscopy negative reflux disease. Cochrane Database Syst Rev. 2013;5:CD002095. https://doi.org/10.1002/14651858.CD002095.pub5
178. Robinson M., Horn J. Clinical Pharmacology of Proton Pump Inhibirors. What the Practising Physycian needs to know. Drug. 2003;63(24):2739-54. https://doi.org/10.2165/00003495-200363240-00004
179. Besancon M., Simon A., Sachs G., Shin J.M. Sites of reaction of the gastric H,K-ATPase with extracytoplasmic thiol reagents. J. Biol Chem. 1997;272:22438-46. https://doi.org/10.1074/jbc.272.36.22438
180. Kromer W. Relative efficacies of gastric proton-pump inhibitors on a milligram basis: desired and undesired SH reactions. cokinetic profiles of PPIs can influence their safety Impact of chirality. Scand J Gastroenterol Suppl. 2001;234:3-11. https://doi.org/10.1080/003655201753265389
181. Kromer W., Kruger U., Huber R., Hartmann M., Steini-jans V.W. Differences in pH dependent activation rates of substituted benzimidazoles and control over acid secretion and onset of symptom biological in vitro correlates. Pharmacology. 1998;56:57-70. https://doi.org/10.1159/000028183
182. Pantoflickova D., Dorta G., Ravic M., Jornod P., Blum A.L. Acid inhibition on the first day of dosing: comparison of four proton pump inhibitors. Aliment Pharmacol Ther. 2003;17:1507-14. https://doi.org/10.1046/j.1365-2036.2003.01496.x
183. Horn J. Review article: understanding the pharmacodynamic and pharmacokinetic differences between proton pump inhibitors - focus on pKa and metabolism. Alimentary Pharmacology & Therapeutics Symposium Series. 2006;2:340-50. https://doi.org/10.1111/j.1746-6342.2006.00065.x
184. Dekkers C.P., Beker J.A., Thjodleifsson B., Gabryele-wicz A., Bell N.E., Humphries T.J. Double-blind placebo controlled comparison of rabeprazole 20 mg vs. omeprazole 20 mg in the treatment of erosive or ulcerative gastro-oesophageal reflux disease. The European Rabeprazole Study Group. Aliment Pharmacol Ther. 1999;13(1):49-57. https://doi.org/10.1046/j.1365-2036.1999.00438.x
185. Scott J.L., Dunn C.J., Mallarkey G., Sharpe M. Esomeprazole. A review of its use in the management of acid-ralated disorders. Drugs. 2002;62(10):1503-38. https://doi.org/10.2165/00003495-200262100-00006
186. Miner P. Jr, Katz P.O., Chen Y., Sostek M. Gastric acid control with esomeprazole, lansoprazole, omeprazole, pantoprazole, and rabeprazole: A five-way crossover study. Am J Gastroenterol. 2003;98:2616-20. https://doi.org/10.1111/j.1572-0241.2003.08783.x
187. Miner P. Jr, Katz P.O., Chen Y., Sostek M. Reanalysis of intragastric pH results based on updated correction factors for Slimline® and Zinetics™ 24 single-use pH catheters. Am J Gastroenterol. 2006;101(2):404-5. https://doi.org/10.1111/j.1572-0241.2006.00401_3.x
188. Lind T., Rydberg L., Kyleback A., Jonsson A., Andersson T., Hasselgren G., et al. Esomeprazole provides improved acid control vs. omeprazole in patients with symptoms of gastro-oesophageal reflux disease. Aliment Pharmacol Ther. 2000;14:861-7. https://doi.org/10.1046/j.1365-2036.2000.00813.x
189. Li M.J., Li Q., Sun M., Liu L. Comparative effectiveness and acceptability of the FDA-licensed proton pump inhibitors for erosive esophagitis. Medicine (Baltimore). 2017;96(39):e8120. https://doi.org/10.1097/MD.0000000000008120
190. Kahrilas P. J., Falk G. W., Johnson D. A., Schmitt C., Collins D.W., Whipple J., et al. Esomeprazole improves healing and symptom resolution as compared with omeprazole in reflux oesophagitis patients: a randomized controlled trial. Aliment Pharmacol Ther. 2000;14(10):1249-58. https://doi.org/10.1046/j.1365-2036.2000.00856.x
191. Richter J. E., Kahrilas P. J., Johanson J., Maton P., Breiter J.R., Hwang C., et al. Efficacy and safety of esomeprazole compared with omeprazole in GERD patients with erosive esophagitis: a randomized controlled trial. Am J Gastroenterol. 2001;96(3):656-65. https://doi.org/10.1111/j.1572-0241.2001.3600_b.x
192. Bhad M.E., Abdul S., Jaiswal S., Chandewar A.V. MUPS Tablets - A Brief Review. International Journal of PharmTech Research. 2010;2(1):847-55.
193. Shindina T.S., Maksimov M.L., Kropova O.E. Ingibitory protonnoi pompy v terapii kislotozavisimykh zabolevanii. RMZh. 2014;22(20):1459-63.
194. Kukulka M., Wu J., Perez M.C. Pharmacokinetics and safety of dexlansoprazole MR in adolescents with symptomatic GERD. J Pediatr Gastroenterol Nutr. 2012;54(1):41-7. https://doi.org/10.1097/MPG.0b013e31822a323a
195. Vakily M., Zhang W., Wu J., Atkinson S.N., Darcy M. Pharmacokinetics and pharmacodynamics of a known active PPI with a novel Dual Delayed Release technology, dexlansoprazole MR: a combined analysis of randomized controlled clinical trials. Curr Med Res Opin. 2009;25(3):627-38. https://doi.org/10.1185/03007990802693883
196. Zhang W., Wu J., Atkinson S. Pharmacokinetics, pharmacodynamics, and safety evaluation of a single and multiple 60 mg, 90 mg, and 120 mg oral doses of modified-release TAK-390 (TAK-390MR) and 30 mg oral doses of lansoprazole in healthy subjects. Gastroenterology. 2007;132(52):487A.
197. Behm B.W., Peura D.A. Dexlansoprazole MR for the management of gastroesophageal reflux disease. Expert Rev Gastroenterol Hepatol. 2011;5:439-45. https://doi.org/10.1586/egh.11.37
198. Shin J.M., Kim N. Pharmacokinetics and Pharmacodynamics of the Proton Pump Inhibitors. J Neuro-gastroenterol Motil. 2013;19:25-35. https://doi.org/10.5056/jnm.2013.19.1.25
199. Fass R., Johnson D.A., Orr W.C., Han C., Mody R., Stern K.N., et al. The Effect of Dexlansoprazole MR on Nocturnal Heartburn and GERD-Related Sleep Disturbances in Patients With Symptomatic GERD. Am J Gastroenterol. 2011;106(3):421-31. https://doi.org/10.1038/ajg.2010.458
200. Freedberg D.E., Kim L.S., Yang Y.X. The Risks and Benefits of Long-term Use of Proton Pump Inhibitors: Expert Review and Best Practice Advice From the American Gastroenterological Association. Gastroenterology. 2017;152(4):706-15. https://doi.org/10.1053/j.gastro.2017.01.031
201. Moayyedi P., Delaney B., Forman D. Gastro-oesophageal reflux disease. Clin Evid. 2005;14:567-81.
202. Targownik L.E., Lix L.M., Leung S., Leslie W.D. Proton-pump inhibitor use is not associated with osteoporosis or accelerated bone mineral density loss. Gastroenterology. 2010;138:896-904. https://doi.org/10.1053/j.gastro.2009.11.014
203. Ngamruengphong S., Leontiadis G.I., Radhi S., Den-tino A., Nugent K. Proton pump inhibitors and risk of fracture: a systematic review and meta-analysis of observational studies. Am J Gastroenterol. 2011;106:1209-18. https://doi.org/10.1038/ajg.2011.113
204. Bavishi C., Dupont H.L. Systematic review: The use of proton pump inhibitors and increased susceptibility to enteric infection. Aliment Pharmacol Ther. 2011;34:1269-81. https://doi.org/10.1111/j.1365-2036.2011.04874.x
205. Eom C.S., Jeon C.Y., Lim J.W., Cho E., Park S.M., Lee K. Use of acid-suppressive drugs and risk of pneumonia: A systematic review and meta-analysis. CMAJ. 2011;183:310-9. https://doi.org/10.1503/cmaj.092129
206. Johnstone J., Nerenberg K., Loeb M. Meta-analysis: Proton pump inhibitor use and the risk of community-acquired pneumonia. Aliment Pharmacol Ther. 2010;31:1165-77. https://doi.org/10.1111/j.1365-2036.2010.04284.x
207. Lind T., Havelund T., Lundell L., Glise H., Lauritsen K., Pedersen S.A., et al. On demand therapy with omeprazole for the long-term management of patients with heartburn without oesophagitis - a placebo-controlled randomized trial. Aliment Pharmacol Ther. 1999;13:907-14. https://doi.org/10.1046/j.1365-2036.1999.00564.x
208. Pace F., Tonini M., Pallotta S., Molteni P., Porro G.B. Systematic review: Maintenance treatment of gastro-oesophageal reflux disease with proton pump inhibitors taken “on-demand”. Aliment Pharmacol Ther. 2007;26:195-204. https://doi.org/10.1111/j.1365-2036.2007.03381.x
209. Ogawa R., Echizen N. Drug-drug interaction profiles of proton pump inhibitors. Clin Pharmacokinet. 2010;49(8):509-33. https://doi.org/10.2165/11531320-000000000-00000
210. Kirchheiner J., Glatt S., Fuhr U., Klotz U., Meineke I., Seufferlein T., Brockmoller J. Relative potency of proton-pump inhibitors-comparison of effects on intragastric pH. Eur J Clin Pharmacol. 2009;65(1):19-31. https://doi.org/10.1007/s00228-008-0576-5
211. Caos A., Breiter J., Perdomo C., Barth J. Long-term prevention of erosive or ulcerative gastro-oesophageal reflux disease relapse with rabeprazole 10 or 20 mg vs. placebo: results of a 5-year study in the United States. Alim Pharmacol Ther. 2005;22:193-202. https://doi.org/10.1111/j.1365-2036.2005.02555.x
212. Zaborovskii A.V., Maev I.V., Andreev D.N., Tararina L.A. Pleiotropnye effekty rabeprazola i ikh rol' v lechenii patsientov s kislotozavisimymi zabolevaniyami. Ros zhurn gastroenterol gepatol koloprok-tol. 2017;27(3):18-26. https://doi.org/10.22416/1382-4376-2017-27-3-18-26
213. Ivashkin V.T., Maev I.V., Abdulkhakov R.A., Alekseeva O.P., Alekseenko S.A., Baranovskii A.Yu. i dr. Infektsiya Helicobacter pylori pri dlitel'noi terapii kislotozavisimykh zabolevanii ingibitorami protonnoi pompy (Obzor literatury i rezolyutsiya Ekspertnogo soveta, 22 marta 2018 g.). Ros zhurn gastroenterol gepatol koloproktol. 2018;28(3):26-32. https://doi.org/10.22416/1382-4376-2018-28-3-26-32
214. Ivashkin V.T., Maev I.V., Trukhmanov A.S., Rumyantseva D.E. Sovremennye dostizheniya v diagnostike i lechenii refrakternoi formy gastroezofageal'noi reflyuksnoi bolezni. Terapevticheskii arkhiv. 2018;90(8):4-12. https://doi.org/10.26442/terarkh20189084-12
215. Roman S., Mion F. Refractory GERD, Beyond Proton Pump Inhibitors. Curr Opin Pharmacol. 2018;43:99-103. https://doi.org/10.1016/j.coph.2018.09.001
216. Evsyutina Yu.V., Trukhmanov A.S. Algoritm vedeniya patsientov s refrakternoi formoi GERB. RMZh. 2015;28:1682-3.
217. Ichikawa H., Sugimoto M., Sugimoto K., Andoh A., Furuta T. Rapid metabolizer genotype of CYP2C19 is a risk factor of being refractory to proton pump inhibitor therapy for reflux esophagitis. Journal of Gastroenterology and Hepatology. 2016;31:716-26. https://doi.org/10.1111/jgh.13233
218. Samer C.F., Lorenzini K.I., Rollason V., Daali Y., Desmeules J.A., et al. Applications of CYP450 Testing in the Clinical Setting. Mol Diagn Ther. 2013;17:165-84. https://doi.org/10.1007/s40291-013-0028-5
219. Sarosiek I., Olyaee M., Majewski M., Sidorenko E., Roeser K., Sostarich S., et al. Significant Increase of Esophageal Mucin Secretion in Patients with Reflux Esophagitis After Healing with Rabeprazole: Its Esoph-agoprotective Potential. Dig. Dis. Sci. 2009;54:2137-42. https://doi.org/10.1007/s10620-008-0589-z
220. Takiuchi H., Asado S., Umegaki E., Tahashi Y., Ohshiba S. Effects of proton pump inhibitors: omeprazole, lansoprazole and E-3810 on the gastric mucin. In: Proc. 10* World Congress of Gastroenterol. Los Angeles, 1994.
221. Ivashkin V.T., Trukhmanov A.S., Gonik M.I. Primenenie rebamipida v lechenii gastroezofageal'noi reflyuksnoi bolezni. Terapevticheskii arkhiv. 2020;92(4):98-104. https://doi.org/10.26442/00403660.2020.04.000568.
222. Pandolfino J.E., Vela M.F. Esophageal-reflux monitoring. Gastrointest Endosc. 2009;69:917-30. https://doi.org/10.1016/j.gie.2008.09.022
223. Sablin O.A., Il'chishina T.A. Problemy notsitseptsii pri gastroezofageal'noi reflyuksnoi bolezni: diagnostika i lechenie razdrazhennogo pishchevoda. Terapevticheskii arkhiv. 2018;90(8):118-24. https://doi.org/10.26442/terarkh2018908118-124
224. Wileman S.M., McCann S., Grant A.M., Krukows-ki Z.H., Bruce J. Medical versus surgical management for GERD in adults. Cochrane Database Syst Rev. 2010;17;(3):CD003243. https://doi.org/10.1002/14651858.CD003243.pub2
225. Strugala V., Bassin J., Swales V.S., Lindow S.W., Dettmar P.W., Thomas E.C.M. Assessment of the Safety and Efficacy of a Raft-Forming Alginate Reflux Suppressant (Liquid Gaviscon) for the Treatment of Heartburn during Pregnancy. International Scholarly Research Network Obstetrics and Gynecology. 2012(9):481870. https://doi.org/10.5402/2012/481870
226. Lindow S.W., Regnell P., Sykes J., Little S. An openlabel, multicentre study to assess the safety and efficacy of a novel reflux suppressant (Gaviscon Advance) in the treatment of heartburn during pregnancy. International Journal of Clinical Practice. 2003;57(3):175-9.
227. Mandel K.G., Daggy B. P., Brodie D. A., Jacoby H. I. Review article: alginate-raft formulation in the treatment of heartburn and acid reflux. Aliment. Pharmacol. Ther. 2000;14:669-90. https://doi.org/10.1046/j.1365-2036.2000.00759.x
Статьи по теме
Рекомендуемые статьи
Эластография при эндосонографии (ЭУС или эндоУЗИ)
Эластография (эластосонография) – метод виртуальной пальпации (технология улучшенной визуализации при ЭУС диагностике), позволяющий дифференцировать злокачественные и доброкачественные поражения лимфоузлов. Основана на принципе, что более мягкие ткани при сжатии легче деформируются, это позволяет объективно оценить консистенцию ткани, показать различия в плотности между нормальными и патологически измененными тканями.
При эндоскопическом исследовании в случае бронхоэктазов в стадии ремиссии выявляется
частично диффузный бронхит I степени воспаления
Активируйте PUSH уведомления в браузер
Отключите PUSH уведомления в браузер
Содержание
Интернет магазин
Популярное
- О нас
- Правовые вопросы
- Политика
обработки персональных
данных EndoExpert.ru - Связаться с нами
- Стать партнером
© 2016-2022 EndoExpert.ru

Вы находитесь в разделе предназначенном только для специалистов (раздел для пациентов по ссылке). Пожалуйста, внимательно прочитайте полные условия использования и подтвердите, что Вы являетесь медицинским или фармацевтическим работником или студентом медицинского образовательного учреждения и подтверждаете своё понимание и согласие с тем, что применение рецептурных препаратов, обращение за той или иной медицинской услугой, равно как и ее выполнение, использование медицинских изделий, выбор метода профилактики, диагностики, лечения, медицинской реабилитации, равно как и их применение, возможны только после предварительной консультации со специалистом. Мы используем файлы cookie, чтобы предложить Вам лучший опыт взаимодействия. Файлы cookie позволяют адаптировать веб-сайты к вашим интересам и предпочтениям.
Я прочитал и настоящим принимаю вышеизложенное, хочу продолжить ознакомление с размещенной на данном сайте информацией для специалистов.

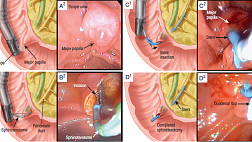







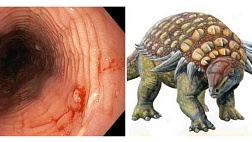


.jpg)
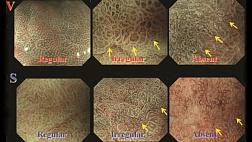


.png)













Комментарии