- Компании
- Takeda. О компании, буклеты, каталоги, контакты
- Olympus. О компании, буклеты, каталоги, контакты
- Boston Scientific. О компании, буклеты, каталоги, контакты
- Pentax. О компании, буклеты, каталоги, контакты
- Fujifilm & R-Farm. О компании, буклеты, каталоги, контакты
- Erbe. О компании, буклеты, каталоги, контакты
- Еще каталоги
- Мероприятия
- Информация
- Обучение
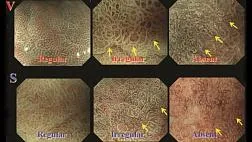
- Классификации
- Атлас
- Quiz
- Разделы
- Пациенту
QR-код этой страницы
Для продолжения изучения на мобильном устройстве ПРОСКАНИРУЙТЕ QR-код с помощью спец. программы или фотокамеры мобильного устройства
Статьи: Российский консенсус по актуальным вопросам диагностики и лечения синдрома механической желтухи
Полный текст статьи:
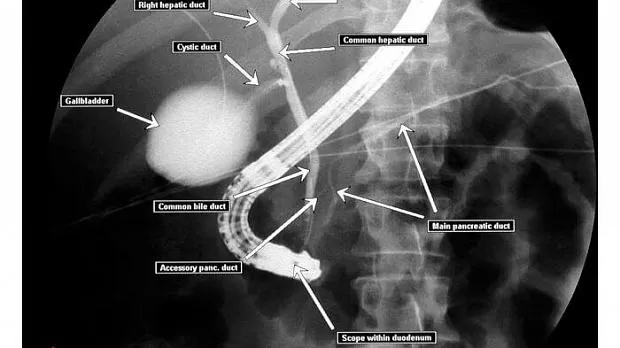
Российский консенсус (согласительный документ) по актуальным вопросам диагностики и лечения синдрома механической желтухи подготовлен группой экспертов различных областей хирургии, эндоскопии, интервенционной радиологии, лучевой диагностики и интенсивной терапии. Цель консенсуса — выяснение и консолидация мнений российских специалистов по таким актуальным вопросам, как срок диагностики механического характера желтухи, порядок выполнения диагностических исследований, необходимость и возможности консервативных мероприятий при механической желтухе, тактика декомпрессии желчных протоков в зависимости от причины и уровня билиарного блока.
- И. Е. Хатьков
ГБУЗ «МКНЦ им. А.С. Логинова ДЗМ», Москва, Россия - Р. Г. Аванесян
СПб ГБУЗ «Городская Мариинская больница», Санкт-Петербург, Россия - Г. Г. Ахаладзе
ФГБУ «РНЦРР» МЗ РФ, Москва, Россия - А. Г. Бебуришвили
ФУВ ФГБОУ ВО «ВолгГМУ», Волгоград, Россия - А. Ю. Буланов
ГБУЗ «Городская клиническая больница № 52 ДЗМ», Москва, Россия - М. И. Быков
ГБУЗ «Краевая клиническая больница № 1 им. С.В. Очаповского» МЗКК, Краснодар, Россия - Э. Г. Виршке
ФГБУ «НМИЦ онкологии им. Н.Н. Блохина» МЗ РФ, Москва, Россия - С. А. Габриэль
ГБУЗ «Краевая клиническая больница № 2» МЗКК, Краснодар, Россия - Д. А. Гранов
ФГБУ «РНЦРиХТ им. А.М. Гранова» МЗ РФ, Санкт-Петербург, Россия - В. В. Дарвин
ГБУ «Сургутская окружная клиническая больница», Сургут, Россия - Б. И. Долгушин
ФГБУ «НМИЦ онкологии им. Н.Н. Блохина» МЗ РФ, Москва, Россия - Т. Г. Дюжева
ФГАОУ ВО «Первый МГМУ им. И.М. Сеченова» МЗ РФ, Москва, Россия - М. Г. Ефанов
ГБУЗ «МКНЦ им. А.С. Логинова ДЗМ», Москва, Россия - В. Л. Коробко
ГБУЗ РО «Ростовская областная клиническая больница», Ростов-на-Дону, Россия - М. П. Королев
СПб ГБУЗ «Городская Мариинская больница», Санкт-Петербург, Россия - В. В. Кулабухов
ФГБУ «НМИЦ онкологии им. Н.Н. Блохина» МЗ РФ, Москва, Россия - Н. А. Майстренко
ФГБВОУ ВО «Военно-медицинская академия им. С.М. Кирова», Санкт-Петербург, Россия - О. В. Мелехина
ГБУЗ «МКНЦ им. А.С. Логинова ДЗМ», Москва, Россия - И. Ю. Недолужко
ГБУЗ «МКНЦ им. А.С. Логинова ДЗМ», Москва, Россия - О. И. Охотников
БМУ «Курская областная клиническая больница» КЗКО, Курск, Россия - В. Ю. Погребняков
ГУЗ ЗК «Краевая клиническая больница, Чита, Россия - А. А. Поликарпов
ГБУЗ «Краевая клиническая больница № 2» МЗКК, Краснодар, Россия - М. И. Прудков
ГБУЗ СО «Свердловская областная клиническая больница №1», Свердловск, Россия - В. А. Ратников
ФГБУЗ «Клиническая больница № 122 им. Л.Г. Соколова» ФМБА России, Санкт-Петербург, Россия - Е. Н. Солодинина
ФГБУ «ЦКБ с поликлиникой» Управления делами Президента РФ, Москва, Россия - Ю. А. Степанова
ФГБУ «НМИЦ хирургии им. А.В. Вишневского» МЗ РФ, Москва, Россия - В. В. Субботин
ГБУЗ «МКНЦ им. А.С. Логинова ДЗМ», Москва, Россия - Е. Д. Федоров
ФГАОУ ВО «РНИМУ им. Н.И. Пирогова» МЗ РФ, Москва, Россия - А. В. Шабунин
ГБУЗ «ГКБ им. С.П. Боткина» ДЗМ, Москва, Россия - С. Г. Шаповальянц
ФГАОУ ВО «РНИМУ им. Н.И. Пирогова» МЗ РФ, Москва, Россия - А. М. Шулутко
ФГАОУ ВО «Первый МГМУ им. И.М. Сеченова» МЗ РФ, Москва, Россия - К. В. Шишин
ГБУЗ «МКНЦ им. А.С. Логинова ДЗМ», Москва, Россия - В. Н. Цвиркун
ГБУЗ «МКНЦ им. А.С. Логинова ДЗМ», Москва, Россия - А. В. Чжао
ФГБУ «НМИЦ хирургии им. А.В. Вишневского» МЗ РФ, Москва, Россия - Ю. В. Кулезнева
ГБУЗ «МКНЦ им. А.С. Логинова ДЗМ», Москва, Россия
Список литературы:
1. Руководство по хирургии желчных путей: 2-е изд. Под ред. Э.И. Гальперина, П.С. Ветшева. М.: Видар-М; 2009.
2. Шевченко Ю.Л., Ветшев П.С., Стойко Ю.М. и др. Диагностика и хирургическая тактика при синдроме механической желтухи. Анналы хирургической гепатологии. 2008;13(4):96-107.
3. Гальперин Э.И., Момунова О.Н. Классификация тяжести механической желтухи. Хирургия. Журнал им. Н.И. Пирогова. 2014; 1:5-9.
4. Майстренко Н.А., Стукалов В.В. Холедохолитиаз. СПб: ЭЛБИ-СПб; 2000.
5. Fargo MV, Grogan SP, Saguil A. Evaluation of Jaundice in Adults. Am Fam Physician. 2017 Feb 1;95(3):164-168. Review.
6. Taylor A, Stapley S, Hamilton W. Jaundice in primary care: a cohort study of adults aged more 45 years using electronic medical records. Fam Pract. 2012;29:416-420.
7. Center SA. Diseases of the gallbladder and biliary tree. Vet Clin North Am Small Anim Pract. 2009;39(3):543-598.
8. Gallstone Disease: Diagnosis and Management of Cholelithiasis, Cholecystitis and Choledocholithiasis. Internal Clinical Guidelines Team (UK)London: National Institute for Health and Care Excellence (UK); 2014 Oct. PMID: 25473723
9. Williams E, Beckingham I, Sayed G, et al. Updated guideline on the management of common bile duct stones (CBDS). 2017;66(5):765-782.
10. Шулутко А.М, Овчиннников А.А., Ветшев П.С. Рабочий диагноз в трудных хирургических ситуациях. М.: Медицина; 2003.
11. Подолужный В.И. Механическая желтуха: принципы диагностики и современного хирургического лечения. Фундаментальная и клиническая медицина. 2018;3(2):82-92.
12. Национальное руководство «Клиническая хирургия». Т. 2. М.: ГЭОТАР-Медиа; 2009.
13. Miyazaki M, Yoshitomi H, Miyakawa S, et al. Clinical practice guidelines for the management of biliary tract cancers 2015: the 2nd English edition. J Hepatobiliary Pancreat Sci. 2015;22:249-273.
14. Creditt AB, Tozer J, Joyce M. Biliary Ultrasound. Clinical Ultrasound; 2018:149-165.
15. Katon RM. Algorithm for an aggressive diagnostic approach to obstructive jaundice. RM Katon, MK Bilbao, J Rsoch. West J Med. 1975; 122(3):206-216.
16. Gurusamy KS, Giljaca V, Takwoingi Y, et al. Ultrasound versus liver function tests for diagnosis of common bile duct stones. Cochrane Database Syst Rev. 2015;(2):CD011548.
17. Tse F, Barkun JS, Romagnuolo J, et al. Nonoperative imaging techniques in suspected biliary tract obstruction. HPB. 2006;8:409-425.
18. Badger WR, Borgert AJ, Kallies KJ. Utility of MRCP in clinical decision making of suspected choledocholithiasis: An institutional analysis and literature review. Am J Surg. 2017;214(2):251-255.
19. Venkata S Katabathina, Anil K Dasyam, Navya Dasyam. Adult Bile Duct Strictures: Role of MR Imaging and MR Cholangiopancreatography in Characterization. RadioGraphics. 2014;34(3):565-586.
20. Addlev J, Mitchell RM. Advances in the investigation of obstructive jaundice. Curr Gastroenterol Rep. 2012;14(6):511-519.
21. Нечипай А.М., Орлов С.Ю., Федоров Е.Д. ЭУСбука. Руководство по эндоскопической ультрасонографии. Практическая медицина; 2013.
22. Hidalgo M, Alvarez R, Gallego J, et al. Consensus guidelines for diagnosis, treatment and follow-up of patients with pancreatic cancer in Spain. Clinical and Translational Oncology. 2017;19(6):667-681.
23. Petrescu I, Bratu AM, Petrescu S. CT vs. MRCP in choledocholithiasis jaundice. J Med Life. 2015;8(2):226-231.
24. Joo I, Lee JM, Yoon JH. Imaging Diagnosis of Intrahepatic and Perihilar Cholangiocarcinoma: Recent Advances and Challenges. Radiology. 2018 July;288(1):7-13. Epub 2018 Jun 5.
25. Hekimoglu K, Ustundag Y, Dusak A, et al. MRCP vs. ERCP in the evaluation of biliary pathologies: review of current literature. J Dig Dis. 2008;9:162-169.
26. Xin-dao Y, Li-ping W, Ling-quan LU, et al. Favorite Get Role of combining MR cholangiopancreatography and T_1WI in detecting micro-choledocholithiasis. Journal of China Clinic Medical Imaging. 2007;07.
27. Arain MA, Freeman ML, Howell DA, et al. Choledocholithiasis: Clinical manifestations, diagnosis, and management. Literature review current through: Nov 2018.
28. Karlsen TH, Folseraas T, Thorburn D, Vesterhus M. Primary sclerosing cholangitis – a comprehensive review. Journal of Hepatology. 2017;67:1298-1323.
29. Naess S, Bjornsson E, Anmarkrud JA, et al. Small duct primary sclerosing cholangitis without inflammatory bowel disease is genetically different from large duct disease. Liver Int. 2014;34(10):1488-1495.
30. Eimorn Mairiang. Clinical manifestation of opisthorchiasis and treatment, Acta Tropica Dec. 2003;88(3):221-227. https://doi.org/10.1016/j.actatropica.2003.03.001
31. Deltenre P, Valla DCh. Ischemic cholangiopathy. Review. Journal of Hepatology. 2006;44:806-817.
32. European Association for the Study of the L. EASL Clinical Practice Guidelines: management of cholestatic liver diseases. Journal of Hepatology. 2009;51(2):237-267.
33. Lee DW, Chan AC, Lam YH, Ng EK, Lau JY, Law BK, et al. Biliary decompression by nasobiliary catheter or biliary stent in acute suppurative cholangitis: a prospective randomized trial. Gastrointest Endosc. 2002;56:361-365.
34. Bratzler DW, Dellinger EP, Olsen KM, et al. Clinical practice guidelines for antimicrobial prophylaxis in surgery. Am J Health-Syst Pharm. 2013;70:195-283.
35. Gomi H, Solomkin JS, Schlossberg D, et al. Tokyo Guidelines 2018: antimicrobial therapy for acute cholangitis and cholecystitis. J Hepatobiliary Pancreat Sci. 2018 Jan 9;25(1):3-16. Epub 2018 Jan 9.
36. Deitch EA, Sittig K, Li M, Berg R, Specian RD. Obstructive jaundice promotes bacterial translocation from the gut. Am J Surg. 1990;159:79-84.
37. Клинические рекомендации Федерации анестезиологов и реаниматологов России «Периоперационное ведение больных с нарушениями системы гемостаза», 2018 г.
38. Wang L, Yu W-F. Obstructive jaundice and perioperative management. Acta Anaesth. Taiwanica. 2014;52:22-29.
39. Pavlidis ET, Pavridis TE. Pathophysiological consequences of obstructive jaundice and perioperative management. Hepatobiliary Pancreat Dis Int. 2018;17:17-21.
40. Egan RJ, Nicholis J, Walker S, et al. Routine coagulation screening is an unnecessary step to ERCP in patients without biochemical evidence a cross-centre study. Int J Surgery. 2014;12:1216-1220.
41. Abbas MA, Shamshad T, Ashraf VA, Javaid R. Jaundice: a basic review. International Journal of Research in Medical Sciences. Int J Res Med Sci. 2016 May;4(5):1313-1319.
42. Clarke DL, Pillay Y, Anderson F, Thomson SR. The current standard of care in the periprocedural management of the patient with obstructive jaundice. Ann R Coll Surg Engl. 2006;88:610-616.
43. Bergasa NV. Medical palliation of the jaundiced patient with pruritus. Gastroenterol Clin N Am. 2006;35:113-123.
44. Fekaj E, Jankulovski N and Matveeva N. Obstructive Jaundice. Austin Dig Syst. 2017;2(1):1006.
45. Tang Z, Yang Y, Meng W, Li X. Best option for preoperative biliary drainage in Klatskin tumor. Medicine (Baltimore). 2017;96(43):e8372.
46. Dellinger RP, Levy MM, Rhodes A, et al. Surviving Sepsis Campaign: International guidelines for management of severe sepsis and septic shock. Intensive Care Med. 2013;39(2):165-228 and Crit Care Med. 2013;41(2):580-637.
47. Biliary cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up; 2016.
48. LCA Hepato-pancreatobiliary Cancer Clinical Guidelines. Nov 2014.
49. Tokyo Guidelines 2018: updated Tokyo Guidelines for the management of acute cholangitis / acute cholecystitis.
50. Moole H, Bechtold М, Puli SR. Efficacy of preoperative biliary drainage in malignant obstructive jaundice: a meta-analysis and systematic review. World Journal of Surgical Oncology. 2016;14:182.
51. Pereiras RV, Rheingold OJ, Huston D, et al. Relief of malignant obstructive jaundice by percutaneous insertion of a permanent prosthesis in the biliary tree. Ann Intern Med. 1978;89:589-583.
52. Soehendra N, Reynders-Frederix V. Palliative bile duct drainage — a new endoscopic method of introducing a transpapillary drain. Endoscopy. 1980;12(1):8-11.
53. Dumonceau J-M, Tringali A, Blero D, et al. Biliary stenting: Indications, choice of stentsand results: European Society of Gastrointestinal Endoscopy (ESGE) clinical guideline. J Endoscopy. 2012;44:277-292.
54. Expert Panel on Interventional: Fairchild AH, Gipson MG, Hohenwalter EJ, et al. ACR Appropriateness Criteria. Radiologic Management of Biliary Obstruction. J Am Coll Radiol. 2019 May;16(5S):S196-S213.
55. Harsha Moole1, Matthew Bechtold, Srinivas R Puli. Efficacy of preoperative biliary drainage in malignant obstructive jaundice: a meta-analysis and systematic review. World Journal of Surgical Oncology. 2016;14:182.
56. Scheufele F, Schorn S, Demir IE, et al. Preoperative biliary stenting versus operation first in jaundiced patients due to malignant lesions in the pancreatic head: A meta-analysis of current literature. Surgery. 2017 Apr;161(4):939-950.
57. Sauvanet A, Boher JM, Paye F, et al. Severe jaundice increases early severe morbidity and decreases long-term survival after pancreaticoduodenectomy for pancreatic adenocarcinoma. J Am Coll Surg. 2015; 221:380-389.
58. Liu F, Li Y, Wei Y, et al. Preoperative biliary drainage before resection for hilar cholangiocarcinoma: whether or not? A systematic review. Dig Dis Sci. 2011;56(3):663-672.
59. Celotti A, Solaini L, Montori G, et al. Preoperative biliary drainage in hilar cholangiocarcinoma: Systematic review and meta-analysis. Eur J Surg Oncol. 2017;43:1628-1635.
60. Yoshitsugu N, Takahiro T, Keisuke O, et al. Risk factors for a high Comprehensive Complication Index score after major hepatectomy for biliary cancer: a study of 229 patients at a single institution. HPB. 2016;18:735-741.
61. Taylor MC, McLeod RS, Langer B. Biliary stenting versus bypass surgery for the palliation of malignant distal bile duct obstruction: a meta-analysis. Liver Transpl. 2000;6:302-308.
62. De Lima SLA, Bustamante FAC, de Moura EGH et al. Endoscopic palliative treatment versus surgical bypass in malignant low bile duct obstruction: A systematic review and meta-analysis. Int J Hepatobiliary Pancreat Dis. 2015;5:35-46.
63. Glazer ES, Hornbrook MC, Krouse RS. A meta-analysis of randomized trials: immediate stent placement vs. surgical bypass in the palliative management of malignant biliary obstruction. J Pain Symptom Manage. 2014;47:307-314.
64. Martin DJ, Vernon DR, Toouli J. Surgical versus endoscopic treatment of bile duct stones. Cochrane Database Syst Rev. 2006:CD003327.
65. Rhodes M, Sussman L, Cohen L, et al. Randomised trial of laparoscopic exploration of common bile duct versus postoperative endoscopic retrograde cholangiography for common bile duct stones. Lancet. 1998;351:159-161.
66. Ryozawa S, Itoi T, Katanuma A, et al. Japan Gastroenterological Endoscopy Society guidelines for endoscopic sphincterotomy. Dig Endosc. 2018 Mar;30(2):149-173. Epub 2018 Jan 18. Review. PubMed PMID: 29247546. https://doi.org/10.1111/den.13001
67. Dasari BV, Tan CJ, Gurusamy KS, et al. Surgical versus endoscopic treatment of bile duct stones. Cochrane Database Syst Rev. 2013;(12): CD003327.
68. Williams E, Beckingham I, El Sayed G, Gurusamy K, Sturgess R, Webster G, Young T. Updated guideline on the management of common bile duct stones (CBDS). Gut. 2017 May;66(5):765-782. Epub 2017 Jan 25. PubMed PMID: 28122906. https://doi.org/10.1136/gutjnl-2016-312317
69. Kuzu UB, Ödemiş B, Dişibeyaz S, et al. Management of suspected common bile duct stone: diagnostic yield of current guidelines. HPB (Oxford). 2017 Feb;19(2):126-132. Epub 2016 Nov 30. PubMed PMID: 27914763. https://doi.org/10.1016/j.hpb.2016.11.003
70. ERCP Group, Chinese Society of Digestive Endoscopology; Biliopancreatic Group, Chinese Association of Gastroenterologist and Hepatologist; National Clinical Research Center for Digestive Diseases. Chinese guidelines for ERCP (2018). Zhonghua Nei Ke Za Zhi. 2018 Nov 1;57(11):772-801.
71. Nárvaez Rivera RM, González González JA, Monreal Robles R, et al. Accuracy of ASGE criteria for the prediction of choledocholithiasis. Rev Esp Enferm Dig. 2016 June;108(6):309-314. PubMed PMID: 27063334. https://doi.org/10.17235/reed.2016.4212/2016
72. Singhvi G, Ampara R, Baum J, Gumaste V. ASGE guidelines result in cost-saving in the management of choledocholithiasis. Ann Gastroenterol. 2016 Jan-Mar;29(1):85-90.
73. Dumonceau JM, Tringali A, Papanikolaou IS, et al. Endoscopic biliary stenting: indications, choice of stents, and results: European Society of Gastrointestinal Endoscopy(ESGE) Clinical Guideline — Updated October 2017. Endoscopy. 2018 Sept;50(9):910-930.
74. Kint JF, van den Bergh JE, van Gelder RE, et al. Percutaneous treatment of common bile duct stones: results and complications in 110 consecutive patients. Dig. Surg. 2015;32:9-15.
75. Deo KB1, Adhikary S1, Khaniya S1, Shakya VC1, Agrawal CS1 Laparoscopic Choledochotomy in a Solitary Common Duct Stone: A Prospective Study. Minim Invasive Surg. 2018 May 14.
76. Rogers SJ, Cello JP, Horn JK, et al. Prospective randomized trial of LC+LCBDE vs ERCP/S+LC for common bile duct stone disease. Arch Surg. 2010;145:28-33.
77. Testoni PA, Mariani A, Aabakken L, et al. Papillary cannulation and sphincterotomy techniques at ERCP: European Society of Gastrointestinal Endoscopy (ESGE) Clinical Guideline. Endoscopy. 2016;48:657-683.
78. American Society for Gastrointestinal Endoscopy (ASGE) consensus guidelines. The role of ERCP in benign diseases of the biliary tract. Gastrointest Endosc. 2015;81(4):795-803.
79. Asia-Pacific consensus guidelines for endoscopic management of benign biliary strictures. Gastrointest. Endosc. 2017;86(1):44-58.
80. European Society of Gastrointestinal Endoscopy (ESGE) Clinical Guideline. Endoscopic biliary stenting: indica-tions, choice of stents, and results: Updated October 2017. Endoscopy. 2018;50(9):910-930.
81. Aparício DPDS, Otoch JP, Montero EFS, et al. Endoscopic approach for management of biliary strictures in liver transplant recipients: A systematic review and meta-analysis. United European Gastroenterol J. 2016;5:827-845.
82. Coté GA, Slivka A, Tarnasky P, et al. Effect of covered metallic stents compared with plastic stents on benign biliary stricture resolution: a randomized clinical trial. JAMA. 2016;315:1250-1257.
83. Huszár O, Kokas B, Mátrai P, et al. Meta-analysis of the long term success rate of different interventions in benign biliary strictures. PLoS One. 2017;12.
84. Khan MA, Baron TH, Kamal F, et al. Efficacy of self-expandable metal stents in management of benign biliary strictures and comparison with multiple plastic stents: a meta-analysis. Endoscopy. 2017;49:682-694.
85. Haapamäki C, Kylänpää L, Udd M, et al. Randomized multicenter study of multiple plastic stents vs. covered self-expandable metallic stent in the treatment of biliary stricture in chronic pancreatitis. Endoscopy. 2015;47:605-610.
86. Hu B, Sun B, Cai Q, et al. Asia-Pacific consensus guidelines for endoscopic management of benign biliary strictures. Gastrointest Endosc. 2017 July;86(1):44-58.
87. Kaffes A, Griffin S, Vaughan R, et al. A randomized trial of a fully covered self-expandable metallic stent versus plastic stents in anastomotic biliary strictures after liver transplantation. Therap Adv Gastroenterol. 2014;7:64-71.
88. Martins FP, De Paulo GA, Contini MLC, Ferrari AP. Metal versus plastic stents for anastomotic biliary strictures after liver transplantation: a randomized controlled trial. Gastrointest Endosc. 2018 Jan;87(1): 131.e1-131.e13.
89. Siiki A, Helminen M, Sand J, et al. Covered self-expanding metal stents may be preferable to plastic stents in the treatment of chronic pancreatitis-related biliary strictures: a systematic review comparing 2 methods of stent therapy in benign biliary strictures. J Clin Gastroenterol. 2014;48:635-643.
90. Lau WY, Lai EC, Lau SH. Management of bile duct injury after laparoscopic cholecystectomy: a review. Aust N Z J Surg. 2010;80:75-81.
91. Лекции по гепатопанкреатобилиарной хирургии. Под ред. Э.И. Гальперина и Т.Г. Дюжевой. М.: Видар-М; 2011.
92. Bonnel DH, Fingerhut AL. Percutaneous transhepatic balloon dilatation of benign bilioenteric strictures: long-term results in 110 patients. Am J Surg. 2012 June;203(6):675-683.
93. Fidelman N1.Benign Biliary Strictures: Diagnostic Evaluation and Approaches to Percutaneous Treatment. Tech Vasc Interv Radiol. 2015 Dec;18(4):210-217.
94. Azeemuddin M, Turab NA, Chaudhry MBH, Hamid S, Hasan M, Sayani R. Percutaneous Management of Biliary Enteric Anastomotic Strictures: An Institutional Review. Cureus. Epub 2018 Feb 26;10(2):e2228.
95. Cantwell CP1, Pena CS, Gervais DA, Hahn PF, Dawson SL, Mueller PR. Thirty years’ experience with balloon dilation of benign postoperative biliary strictures: long-term outcomes. Radiology. 2008 Dec; 249(3):1050-1057.
96. Hoffmeister A, Mayerle J, Beglinger C, Buchler MW, Bufler P, Dathe K, et al. English language version of the S3-consensus guidelines on chronic pancreatitis: Definition, aetiology, diagnostic examinations, medical, endoscopic and surgical management of chronic pancreatitis. Z Gastroenterol. 2015;53(12):1447-1495.
97. Singham J, Yoshida EM, Scudamore CH. Choledochal cysts part 3 of 3: management. Can J Surg. 2010;53(1):51-56.
98. Tsai S, Pawlik TM. Primary sclerosing cholangitis: the role of extrahepatic biliary resection. Adv Surg. 2009;43(1):175-188.
99. Huszár O, Kokas B, Mátrai P, et al. Meta-Analysis of the Long Term Success Rate of Different Interventions in Benign Biliary Strictures. PLoS One. 2017;12(1):e0169618.
100. Гальперин Э.И., Чевокин А.Ю., Дюжева Т.Г. Особенности симптоматики и хирургического лечения разного типа рубцовых стриктур желчных протоков. Анналы хирургической гепатологии. 2017;22(3):19-28. https://doi.org/10.16931/1995-5464.2017319-28
101. Вишневский В.А., Ефанов М.Г., Икрамов Р.З., Варава А.Б., Трифонов С.А. Современная хирургическая тактика при рубцовых стриктурах желчных протоков. Тенденции и нерешенные вопросы. Анналы хирургической гепатологии. 2017;22(3):11-18. https://doi.org/10.16931/1995-5464.2017311-18
102. Pancreatic Adenocarcinoma. NCCN Clinical Practice Guidelines in Oncology. 2015.
103. Sasahira N, Hamada T, Togawa O, et al. Multicenter study of endoscopic preoperative biliary drainage for malignant distal biliary obstruction. World J Gastroenterol. 2016;22(14):3793-3802.
104. Crippa S, Cirocchi R, Partelli S, Petrone MC, Muffatti F, Renzi C, Falconi M, Arcidiacono PG. Systematic review and meta-analysis of metal versus plastic stents for preoperative biliary drainage in resectable periampullary or pancreatic head tumors. Eur J Surg Oncol. 2016;42(9):1278-1280.
105. Pancreatic Adenocarcinoma. NCCN Clinical Practice Guidelines in Oncology. 2015.
106. Valle JW, Borbath I, Khan SA, et all. Biliary cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up: clinical practice guidelines. Annals of Oncology. 2016;27(5):28-37.
107. Saad WEA, Wallace MJ, Wojak JC, et all. Quality improvement guidelines for percutaneous transhepatic cholangiography, biliary drainage, and percutaneous cholecystostomy. J Vasc Interv Radiol. 2010;21:789-795.
108. Al-Kawas F, Aslanian H, Baillie J, et all. Percutaneous transhepatic vs. Endoscopic retrograde biliary drainage for suspected malignant hilar obstruction: study protocol for a randomized controlled trial. Trials. 2018;19:108.
109. Wiggers JK, Coelen RJS, Rauws EAJ, et al. Preoperative endoscopic versus percutaneous transhepatic biliary drainage in potentially resectable perihilar cholangiocarcinoma (DRAINAGE trial): design and rationale of a randomized controlled trial. BMC Gastroenterology. 2015;15:20.
110. Scheufele F, Schorn S, Demir IE, et al. Preoperative biliary stenting versus operation first in jaundiced patients due to malignant lesions in the pancreatic head: A meta-analysis of current literature. Surgery. 2017;161(4):939-950.
111. Бурдюков М.С., Гусев Д.В., Гвоздев А.А. и др. Индивидуальный подход к выбору тактики билиарной декомпрессии у больных с опухолями гепатобилиопанкреатодуоденальной зоны. Доказательная гастроэнтерология. 2014;3:52-56.
112. Moole H, Bechtold M, Puli SR. Efficacy of preoperative biliary drainage in malignant obstructive jaundice: a meta-analysis and systematic review. World Journal of Surgical Oncology. 2016;14:182.
113. Moole H, Dharmapuri S, Duvvuri A, et al. Endoscopic versus Percutaneous Biliary Drainage in Palliation of Advanced Malignant Hilar Obstruction: A Meta-Analysis and Systematic Review. Canad J Gastroenterol and Hepatol. 2016;8:1-8.
114. Hameed A, Pang T, Chiou J, et al. Percutaneous vs. endoscopic pre-operative biliary drainage in hilar cholangiocarcinoma — a systematic review and meta-analysis. HPB. 2016;18(7):400-410.
115. Mansour JC, Aloia TA, Crane CH, et al. Hilar cholangiocarcinoma: expert consensus statement. HPB. 2015;17(8):691-699.
116. Tang Z, Yang Y, Meng W. Best option for preoperative biliary drainage in Klatskin tumor: A systematic review and meta-analysis. Medicine. 2017;97:1-9.
117. Mahjoub A, Menahem B, Fohlen A, Dupont B, Alves A, Launoy G, Lubrano J. Preoperative biliary drainage in patients with resectable perihilar cholangiocarcinoma: is percutaneous transhepatic biliary drainage safer and more effective than endoscopic biliary drainage? A meta-analysis. J Vasc Intervent Radiol. 2017;28(4):576-582.
118. Liu JG, Wu J, Wang J, Shu GM, Wang YJ, Lou C, Zhang J, Du Z. Endoscopic Biliary Drainage Versus Percutaneous Transhepatic Biliary Drainage in Patients with Resectable Hilar Cholangiocarcinoma: A Systematic Review and Meta-Analysis. J Laparoendosc Adv Surg Tech A. 2018;28(9):1053-1060.
119. Chan C, et al. Biliary decompression in perichilar cholangiocarcinoma improves survival: a single center retrospective analysis. Dig Dis Sci. 2019 Feb;64(2):561-569. Epub 2018 Sep 20.
120. Кукушкин А.И., Давыдов М.И., Долгушин Б.И., Виршке Э.Р. и др. Осложнения чрескожных чреспеченочных рентгеноэндобилиарных вмешательств у больных с механической желтухой опухолевой этиологии. Вестн. РОНЦ им. Н.Н. Блохина РАМН. 2004;3: 108-110.
121. Vienne A, Hobeika E, Gouya H, et al. Prediction of drainage effectiveness during endoscopic stenting of malignant hilar strictures: the role of liver volume assessment. Gastrointest Endosc. 2010;72:728-735.
122. Shim DJ, Gwon DI, Han K, et al. Percutaneous Metallic Stent Placement for Palliative Management of Malignant Biliary Hilar Obstruction. Korean J Radiol. 2018 July-Aug;19(4):597-605.
123. Pu LZ, Hourneaux de Moura EG, Bernardo WM et al Endoscopic stenting for inoperable malignant biliaryobstruction: A systematic review and meta-analysis. World J Gastroenterol. 2015 Dec 21;21(47): 13374-13385.
124. Долгушин Б.И., Сергеева О.Н., Францев Д.Ю. и др. Внутрипротоковая фотодинамическая терапия при воротной холангиокарциноме у неоперабельных больных. Анналы хирургической гепатологии. 2016;21(3):106-118.
125. Zoepf T, Jakobs R, Arnold JC, Apel D, Riemann JF. Palliation of nonresectable bile duct cancer: improved survival after photodynamic therapy. Am J Gastroenterol. 2005;100(11):2426-2430.
126. Lu Y, Liu L, Wu J-C, Bie L-K, Gong B. Efficacy and safety of photodynamic therapy for unresectable cholangiocarcinoma: a meta-analysis. Clinics and Research in Hepatology and Gastroenterology. 2015; 39(6):718.
127. Taylor MC, McLeod RS, Langer B. Biliary stenting versus bypass surgery for the palliation of malignant distal bile duct obstruction: a meta-analysis. Liver Transpl. 2000;6:302-308.
128. De Lima SLA, Bustamante FAC, de Moura EGH et al. Endoscopic palliative treatment versus surgical bypass in malignant low bile duct obstruction: A systematic review and meta-analysis. Int J Hepatobiliary Pancreat Dis. 2015;5:35-46.
129. Glazer ES, Hornbrook MC, Krouse RS. A meta-analysis of randomized trials: immediate stent placement vs. surgical bypass in the palliative management of malignant biliary obstruction. J Pain Symptom Manage. 2014;47:307-314.
130. Artifon EL, Sakai P, Cunha JE et al. Surgery or endoscopy for palliation of biliary obstruction due to metastatic pancreatic cancer. Am J Gastroenterol. 2006;101:2031-2037.
131. Andersen JR, Sørensen SM, Kruse A, et al. Randomised trial of endoscopic endoprosthesis versus operative bypass in malignant obstructive jaundice. Gut. 1989;30:1132-1135.
Статьи по теме
Рекомендуемые статьи
При эндоскопическом исследовании в случае бронхоэктазов в стадии ремиссии выявляется
частично диффузный бронхит I степени воспаления
Активируйте PUSH уведомления в браузер
Отключите PUSH уведомления в браузер
Содержание
Интернет магазин
Популярное
- О нас
- Правовые вопросы
- Политика
обработки персональных
данных EndoExpert.ru - Связаться с нами
- Стать партнером
© 2016-2022 EndoExpert.ru

Вы находитесь в разделе предназначенном только для специалистов (раздел для пациентов по ссылке). Пожалуйста, внимательно прочитайте полные условия использования и подтвердите, что Вы являетесь медицинским или фармацевтическим работником или студентом медицинского образовательного учреждения и подтверждаете своё понимание и согласие с тем, что применение рецептурных препаратов, обращение за той или иной медицинской услугой, равно как и ее выполнение, использование медицинских изделий, выбор метода профилактики, диагностики, лечения, медицинской реабилитации, равно как и их применение, возможны только после предварительной консультации со специалистом. Мы используем файлы cookie, чтобы предложить Вам лучший опыт взаимодействия. Файлы cookie позволяют адаптировать веб-сайты к вашим интересам и предпочтениям.
Я прочитал и настоящим принимаю вышеизложенное, хочу продолжить ознакомление с размещенной на данном сайте информацией для специалистов.















.jpg)


.png)















Комментарии